Last Updated on October 28, 2023
Adjacent Segment Disease is defined as new degenerative changes at a spinal level adjacent to a surgically treated level or levels in the spine, leading to symptoms of radiculopathy, myelopathy, or instability. It is denoted as ASDis
This condition may or may not result in any symptoms.
The term adjacent segment degeneration (ASDeg) is used to represents the radiographic changes without the symptoms.
At present, there is no clearcut or accurate definition of an adjacent segment disease. It refers to a condition in which after a cervical or lumbar spinal fusion, the levels adjacent to the fused level show degeneration which are readily seen radiographically. Thus it is a broad term encompassing many complications of spinal fusion, listhesis, instability, herniated disc, facet hypertrophy and compression fracture of the vertebra.
Due to this complication, current studies are encouraging motion sparing spinal surgery though long-term data are required.
In contrast to adjacent segment degeneration, which is a common radiographic finding, adjacent segment disease is less common. The incidence of ASDis in both the cervical and lumbar spine is between 2% and 4% per year, and ASD is a significant contributor to reoperation rates after spinal arthrodesis.
Why does Adjacent Segment Disease Occur?
ASD is seen more in people who have other risk factors like arthritis or other condition that predispose them to disc degeneration or disease.
The etiology is probably multifactorial, stemming from existing spondylosis at adjacent levels, the predisposed risk to degenerative changes, and altered biomechanical forces near a previous fusion site. Numerous studies have sought to identify both patient and surgical risk factors for ASD, but a consistent, single predictor is not found yet to be found.
Some researchers have pointed out that a damage done to the structures of the spine, during the surgery may be responsible.
The unanswered question is whether the degeneration is due to degenerative changes caused by further aging or fusion of the adjacent level or levels which have put excessive stress.
The answer is not confirmed yet and research is still going on.
Studies have shown that after fusion surgery, there is an increased load on adjacent segments.
This is seen in both cervical and lumbar spine after fusion.
Although no conclusive etiology exists, natural history seems to be an important factor.
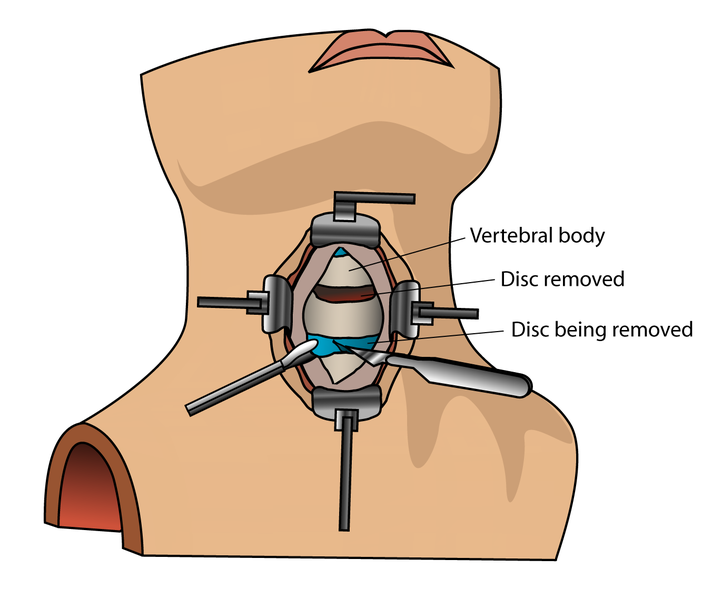
Spinal fusions are used for treatment of back pain and/or instability of the spine.
Soft tissue disruption adjacent to the surgical level is considered a potential cause.
Fusion kills the painful motion and therefore, the pain generator. But it also means loss of a motion segment.
This creates abnormal loads for the spine segments above and below the fusion leading to stress to the nearby facet joints and discs. Wear and tear also cause thickening of the spinal ligaments, which could lead to spinal stenosis.
Disc herniation may occur and spinal instability could result leading to spondylolisthesis.
The patient symptoms would be back pain, radiation of the pain and that of myelopathy.
Treatment of Adjacent Segment Disease
Treatment strategies for ASDis are initially nonoperative.
Conservative treatments can help ease the pain in the early stages.
Physical therapy exercises, injections, anti-inflammatory medications, and modification of activities will all address the symptoms.
But the disease may progress and when severity increases, another fusion surgery may become necessary.
Prevention of Adjacent Segment Disease
Spinal motion preserving surgeries are thought to help by preserving the motion of the spine which spinal fusion blocks. It should minimize the risk but long-term clinical outcome studies are needed to quantify its efficacy.
References
- Cho SK, Riew KD. Adjacent segment disease following cervical spine surgery. J Am Acad Orthop Surg. 2013 Jan;21(1):3–11.
- Matsumoto M, Okada E, Ichihara D, et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 2010 Jan 1;35(1):36–43.
- Dmitriev AE, Cunningham BW, Hu N, Sell G, Vigna F, McAfee PC. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine (Phila Pa 1976) 2005 May 15;30(10):1165–1172.
- Levin DA, Hale JJ, Bendo JA. Adjacent segment degeneration following spinal fusion for degenerative disc disease. Bull NYU Hosp Jt Dis. 2007;65(1):29–36
- Nunley PD, Jawahar A, Kerr EJ. 3rd, et al. Factors affecting the incidence of symptomatic adjacent-level disease in cervical spine after total disc arthroplasty: 2- to 4-year follow-up of 3 prospective randomized trials. Spine (Phila Pa 1976) 2012 Mar 15;37(6):445–451
- Radcliff KE, Kepler CK, Jakoi A, et al. Adjacent segment disease in the lumbar spine following different treatment interventions. Spine J. 2013. Jun 14.