Last Updated on May 20, 2022
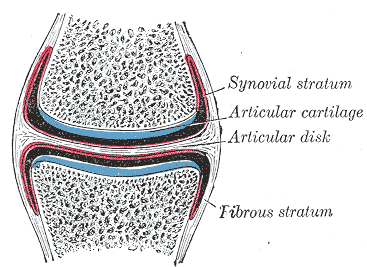
Articular cartilage is the layer covering the joint surfaces. Its main function is to produce smooth articulations between the joint surfaces.
Articular cartilage is the highly specialized connective tissue of diarthrodial joints. Articular cartilage lacks blood vessels, lymphatics, and nerves.
Asa result it has limited healing and repairing mechanisms.
In most joints, adult human articular cartilage is of the hyaline type. The thickness of human articular cartilage varies from area to area within a single joint and from joint to joint. In large joints, the thickness is 2 mm to 4 mm. Knowing the structure of articular cartilage is important so that abnormalities could be noted.
Structure of Articular Cartilage
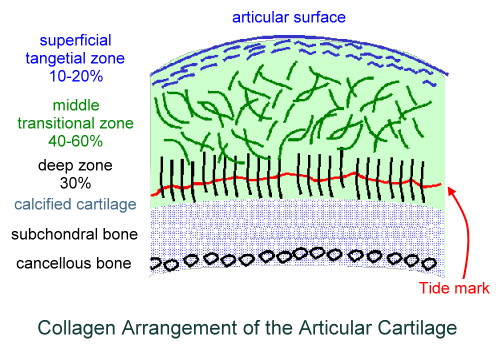
Articular cartilage structure consists of different molecular components consisting of four zones. These zones include:
Superficial or tangential zone
This is the smallest zone that constitutes 10 percent of the cartilage. Collagen fibers are thin and are oriented horizontally to subchondral bone. Low glycan content. This zone is called the lamina splendens.
Middle or transitional zone
it is the largest zone that constitutes 50% of the cartilage. Collagen fibers are thicker and start to be arranged into radial bundles. It has got High proteoglycan and water content.
Deep or radial zone
It constitutes 20% of the cartilage. it carries largest collagen fibers arranged perpendicular to subchondral bone and possesses many chondrocytes.
Calcified zone
This zone separates cartilage from the subchondral bone. Collagen fibers penetrate into this zone and anchor the cartilage to the bone.
Tidemark is a basophilic line that straddles the boundary between calcified and uncalcified cartilage;
Articular cartilage is avascular and lacks nerve structures.
Microscopic Composition of Articular Cartilage
The tissue is composed of a relatively small number of cells and an abundant extracellular matrix. Chondrocyte activity is necessary for the synthesis of the matrix and probably its physiologic degradation and removal.
Extracellular Matrix
The matrix is responsible for maintaining the homeostasis of the environment and is the main component providing the biomechanical properties of the articular cartilage.
The matrix contains a large amount of water, a network of collagen fibers, and a ground substance composed mainly of carbohydrate and noncollagenous protein. A small amount of lipid and inorganic compounds is also present
- Water
- 65% to 80% of the mass of the cartilage
- Accounts for 80% of the weight near the surface.
- In the deep zone, it is about 65%.
- Water content decreases with normal aging
- Water content increases with osteoarthritis
- Increased permeability
- Decreased strength
- Collagen
- 10 to 20% of total cartilage mass
- Provides framework and tensile strength
- Type II is most abundant [ 90% to 95%]
- Small amounts of types V, VI, IX, X, and XI collagen
- Proteoglycans
- 10 to 15% of cartilage
- Provide compressive strength
- Produced by chondrocytes
- Composed of glycoaminoglycans subunits which are mainly chondroitin sulfate and keratin sulfate
- Retain water
- Aggrecan is the most responsible for hydrophilic behavior.
Noncollagenous protein is also present in the matrix
The pericellular matrix contains a delicate meshwork of fine filaments. In mature adult articular cartilage, there is a sharply defined boundary between the pericellular and the intercellular matrix. This zone contains a high concentration of protein and glycoprotein.
The collagen fibers at this site are arranged circumferentially to form a strong enclosure about the chondrocyte.
Cells
Cells of the cartilage are chondrocytes which are derived from their precursor cells called chondroblasts. These cells produce collagen, proteoglycans, and enzymes.
They respond to mechanical stimuli like load and chemical stimuli like growth factors.
Immature articular cartilage also has stem cells but adult articular does not.
Chondrocytes are involved with the physiologic turnover of extracellular ground substances, which is responsible for the biomechanical and biologic properties of this tissue. Chondrocytes exhibit different properties in different zones.
Lubrication of Articular Surfaces
Joint cartilage is lubricated by various mechanisms
Synovial joints serve as mechanical bearings with low coefficients of friction. Their three major sources of lubrication are:
Hydrodynamic Lubrication
Loading of the articular cartilage causes compression that forces water out of the cartilage. This fluid forms an aqueous layer that separates and protects the opposing surfaces.
Boundary-Layer Lubrication
A small glycoprotein called lubricin, which is produced by synovial lining cells, binds to articular cartilage where it retains a protective layer of water molecules.
Hyaluronic Acid
It is produced by synovial lining cells and lubricates the contact surface between synovium and cartilage.
Biomechanics of Articular Cartilage
Articular cartilage is unique in its ability to withstand high cyclic loads without getting damaged.
From our understanding of cartilage structure we can consider the articular cartilage in two phases
- Fluid phase
- Solid-phase
The main component of the fluid phase is water along with inorganic ions such as sodium, calcium, chloride, and potassium are also found in the fluid phase.
Extracellular matrix forms the solid phase.
The extracellular matrix is porous and permeable to allow movement of the fluid in and out.
Initial loading of the joint leads to the outflow of the fluid from the extracellular matrix causing a frictional drag. When the compressive load is removed, interstitial fluid flows back into the tissue.
The fluid pressure thus reduces the stress acting upon the solid matrix.
Age-Related Changes in Articular Cartilage
Age determines
- Composition of the matrix
- Organization of chondrocytes
- Chondrocyte response to external factors such as cytokines.
What happens when the age increases?
- Zonal distribution of chondrocytes changes
- The total number remains the same
- Become less in superficial regions and number increases in deep regions
- This leads to an increase in stiffness causing increased transmission of forces to the subchondral bone
- The size of proteoglycan aggregates decreases
- Increased ratio of keratin sulfate to chondroitin sulfate
Nutrition of Articular Cartilage
Adult cartilage is avascular [does not have any blood supply], and chondrocytes obtain nutrients through diffusion. The nutrients are derived from the synovial fluid whose diffusion is facilitated during joint loading.
With joint loading, some of the water in cartilage is squeezed out into the synovial space. When the joint is unloaded, the hydrophilic properties of the cartilage proteoglycans cause the water to be sucked back into the cartilage. As the water returns to the cartilage, diffusion of nutrients from the synovial fluid is facilitated.
In normal articular cartilage, chondrocytes rarely divide. Chondrocytes synthesize and replace the extracellular matrix components. Proteoglycans have a faster turnover rate compared with collagen.
The degradation of these is accomplished by proteolytic enzymes like Metalloproteases, such as collagenases, stromelysins, and gelatinases.
Cytokines such as interleukin-1 and tumor necrosis factor can increase or upregulate the degradative process, whereas transforming growth factor and insulin-like growth factor-1 have an opposite effect on chondrocyte metabolism.
Diseases of Cartilage
Articular cartilage can be affected by many diseases. The diseases cause degradation of the cartilage
Articular cartilage breakdown can be detected by assays using monoclonal antibodies to measure type II collagen and proteoglycans in bodily fluids.
Important diseases affecting the articular cartilage are
Arthritides
In osteoarthritis, the patients experience pain due to irritation of the subchondral bone, which gets exposed as the cartilage degenerates. Additionally, accumulation of synovial fluid can cause pain through distention of the innervated joint capsule and synovium. Accompanying mild synovial inflammation also causes pain.
Rheumatoid arthritis causes inflammation of the synovial membrane and involves small joints of hands and feet.
Cartilage Injury
A substantial cartilage injury may require repair.
References
- Buckwalter JA. Articular cartilage: injuries and potential for healing. J Orthop Sports Phys Ther. 1998;28:192-202
- Buckwalter JA, Rosenberg LA, Hunziker EB. Articular Cartilage and Knee Joint Function: Basic Science and Arthroscopy. New York, NY: Raven Press; 1990
- Chen FH, Rousche KT, Tuan RS. Technology insight: adult stem cells in cartilage regeneration and tissue engineering. Nat Clin Pract Rheumatol. 2006;2:373-382
- Guilak F, Mow VC. The mechanical environment of the chondrocyte: a biphasic finite element model of cell-matrix interactions in articular cartilage. J Biomech. 2000;33:1663-1673