Last Updated on October 16, 2023
Biceps tendon rupture may occur in the proximal part of the biceps muscle or distal. Proximal biceps tendon rupture accounts for 97% of all biceps ruptures and typically occurs at the bony attachment or tendon labral junction. The long head of the biceps is vulnerable as it travels through the shoulder joint. Fortunately, the biceps has two attachments at the shoulder.
Distal tendon ruptures occur on insertion on the radial tuberosity. Biceps tendon rupture of short head is less common. Biceps tendon ruptures are more common in men and dominant arm is involved more commonly. The difference seems related to use of arm and vocation and as such there appears no gender predisposition to biceps tendon rupture.
Anatomy of Biceps
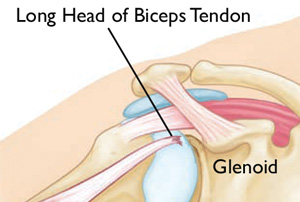
Biceps, as the name suggests, takes its origin from two heads – long head which arises from supraglenoid tubercle and passes over the humeral head within the capsule of the joint and the short head which arises from the coracoid process.
Near midshaft humerus, the two origins join to form a single muscle belly which then goes down and attaches to radial tuberosity below the elbow joint and blends with the bicipital aponeurosis, at cubital fossa.
Biceps muscle functions to flex elbow and supinate forearm. In addition, long head of biceps also acts as stabilizer of humeral head especially in external rotation and abduction.
Proximal biceps rupture results in a decrease of strength during shoulder flexion, elbow flexion, and forearm supination. Distal ruptures cause weakness of supination, elbow flexion, and grip strength.
The tears of biceps tendon could be partial or Complete tears.
Risks and Causes of Biceps Tendon Rupture
Older age, heavy overhead activities, shoulder overuse, smoking and corticosteroid medications and statins increase the risk of biceps tendon rupture.
Overuse can cause a range of shoulder problems, including tendonitis, shoulder impingement, and rotator cuff injuries. Having any of these conditions puts more stress on the biceps tendon, making it more likely to weaken or tear.
Most of the ruptures occur in individuals between the age of 40-60 years following chronic wear of the tendon. The causes of chronic wear are repetitive injury, chronic inflammation as in rheumatoid arthritis and rotator cuff injury.
Acute traumatic injury, heavy weightlifting, or injury during sporting activities may be the reason for rupture in younger patients.
Distal biceps tendon rupture is caused by chronic irritation on an irregular surface, such as in persistent cubital bursitis. Acute distal ruptures result from the forceful extension of the elbow from a flexed and supinated position.
Rapid flexion and adduction of the arm during elbow extension activities may cause short-head rupture though it is very rare.
Presentation of Biceps Tendon Rupture
Sudden, sharp pain in the upper arm, sometimes with an audible pop or snap is the general complaint in proximal biceps tendon rupture. There may be a history of pain in the upper arm prior to the incident especially on overhead activities or pain in the shoulder that may worsen at night.
In contrast to this, there are patients who never experience anything and present with a palpable mass after rupture has occurred. A bulge in the upper arm above the elbow [Popeye Muscle see image below] may appear, with a dent closer to the shoulder.

Tenderness may be present in course of the biceps muscle, especially in bicipital groove. Rotator cuff injuries and impingement may accompany a proximal biceps tendon rupture and shoulder joint should be examined for the range of motion and any weakness.
Speed test and Yergason sign, are used to rule out partial tears or biciptal tendonitis.
In distal biceps tendon ruptures, the symptoms are present near or at the elbow. A palpable gap is in the front of the elbow.
Imaging Studies
In most cases, proximal and distal ruptures can be detected on the basis of history and physical examination alone and imaging generally is not required.
However, AP and axillary views may reveal spurring or bony irregularities which increase the risk of biceps rupture.
Ultrasonography can reliably identify rupture of the proximal end of the long head of biceps but degenerative changes may not be identified easily.
Magnetic resonance imaging provides the best anatomic detail.
Treatment of Biceps Tendon Rupture
The pain of proximal biceps tendon rupture resolves with time. Resulting weakness is generally acceptable to patients with low demands. Because of this second attachment, many people can still use their biceps even after a complete tear of the long head.
Conservative management is considered appropriate for middle-aged or older patients and for those who do not require a high degree of supination strength in daily activities.
In the acute phase, ice for 20 minutes, several times a day should be applied. NSAIDs reduce pain and swelling. A sling is used to provide rest.
After the acute phase, the patient is put on flexibility and strengthening exercises.
Surgical treatment for a long head of the biceps tendon tear is rarely needed. Athletes or manual laborers who need strength may require surgery. Surgery can also be considered for partial tears where symptoms are not relieved with nonsurgical treatment.
Surgical repair consists of tenodesis and subacromial decompression. Successful surgery can correct muscle deformity and return strength and function.
Following surgery, the patient is gradually put on a range of motion exercises which are advanced to strengthening exercises.