Last Updated on May 10, 2020
Cervical spondylosis is a term for degenerative changes (wear and tear) of the vertebral discs and facets of the cervical spine. It is considered to be a normal part of aging. It is not symptomatic in many people but may cause recurring neck pain.
Cervical Spondylosis often progresses with age and frequently involves multiple levels.
Though it is a natural degenerative process of the cervical motion segment it may lead to clinical conditions like cervical radiculopathy [radiating pain in the regions supplied by cervical spine nerves], cervical myelopathy [due to progressive stenosis], and cervical disc disease.
Age-related wear and tear is the biggest factor for the development of cervical spondylosis. However repeated occupational trauma like carrying loads, professional dancing, gymnastics etc. which put repeated strains on the neck may contribute.
Familial cases have also been reported suggesting possible genetic factors also. Smoking is another suggested risk factor.
Conditions that cause increased mobility or instability to a segment of the cervical spine like the congenitally fused spine, cerebral palsy, Down syndrome etc may be risk factors for cervical spondylosis.
Anatomy and Pathophysiology
Read Detailed Anatomy of Cervical Spine
The cervical spine is formed by the seven vertebrae which are named C1 to C7.
Atlas or C1 vertebra along with the Axis (C2) forms the joint connecting the skull and spine and are specialized to allow a greater range of motion.
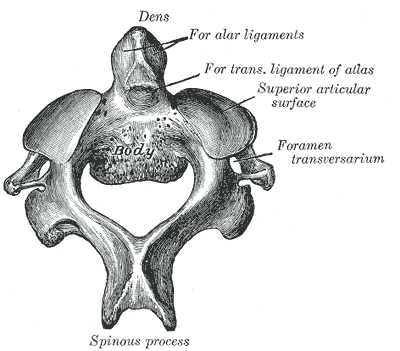
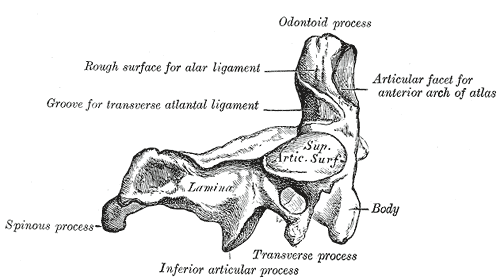
C3 to C7 vertebrae have a relatively uniform anatomic configuration but are quite different than C1 and C2 vertebrae.
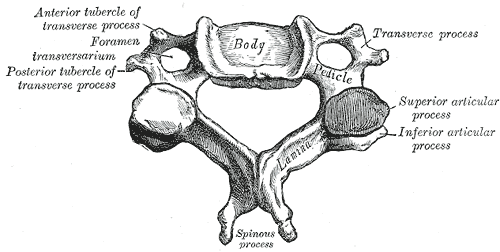
- The vertebral body is larger in coronal than its sagittal diameter and separated by intervertebral discs
- The upper surface of the vertebral body is concave transversely
- The lower surface is concave from front to back
- The transverse processes are each pierced by the foramen transversarium [not consistent in C7]
- From vertebral bodies, pedicles project from anteromedial to the posterolateral direction.
- Facet joints
- Superior articular facets face backward, upward, and slightly medially
- The Inferior facets are forward, downward, and slightly laterally.
- The laminae arise from the posteromedial border of the lateral masses project posterior and toward the midline to form bifid spinous processes.
- The spinous process is short and bifid.
-
- C7 has an enlarged spinous process called vertebra prominens.
Ligaments and muscles provide stability and motion.
From the spinal cord, at each vertebral level spinal nerves exit through neural foramina to supply their respective regions.
Boundaries of neural foramen are
- Anteromedially – uncovertebral joints
- Posterolaterally – facet joints
- Superiorly – pedicle of the superior vertebra
- Inferiorly- pedicle of the lower vertebra
- Medially- Edge of the endplates and the intervertebral discs.
The foramina are largest at C2-C3. they progressively decrease in size down to C6-C7. Spinal nerve occupies 25-33% of the foraminal space.
The spinal nerves exit above their correspondingly numbered vertebral body from C2-C7.
The first nerve C1 is between the occiput and the atlas (C1) and the eighth nerve exits between C7 and T1.
Pathoanatomy
In cervical spondylosis, the edges of the vertebrae often develop small, rough protrusions of the bone (osteophytes) which are in response to thinning of discs.
There is a loss of hydration and elasticity with age leading to fissures.
Ligaments also lose the water content and develop bony spurs due to traction.
The cracks lead to biomechanical incompetence of the disc causing the annulus to bulge outward. This reduces disc space and overriding of facet joints.
This leads to increased motion at that spinal segment, leading to further damage.
The changes may lead to a decrease in the area of the canal due to hypertrophy of facet joints and ligamentum flavum. Facet joint hypertrophy and hypertrophy of the uncinate process of the vertebral body cause a decrease in intervertebral foraminal space posterolaterally and anterolaterally respectively.
Intervertebral foramina is the canal through which the nerve root comes out of the spine.
Marginal osteophytes then begin to develop due to stress. The process could be hastened by trauma or long term heavy use of the neck.
The osteophytes tend to stabilize the vertebral bodies and increase the weight-bearing surface of the vertebral endplates.
Mostly asymptomatic, these osteophytes may cause compression on nearby muscles, ligaments, or nerves to cause pain in the neck and surrounding area. The involvement of a nerve leading to pain and other symptoms in the upper limb is called cervical radiculopathy.

Degradation of intervertebral discal proteoglycans also causes irritation of nerve root leading to cervical radiculopathy.
Cervical spondylotic myelopathy occurs when the changes in cord occur because of degenerative changes causing mechanical compression, spinal cord ischemia, and stretch injury to the spinal cord.
The patients with narrow spinal canal are predisposed to developing cervical spondylotic myelopathy. Space may be further worsened by hypertrophy of the ligamentum flavum, thickening of bone, degenerative kyphosis, and subluxation.
[Cervical spondylotic myelopathy]
Presentation of Cervical Spondylosis
Cervical spondylosis presentation depends on the severity and duration though all cases do not progress. The spectrum of the presentation can be
- Cervical pain
- Cervical radiculopathy
- Cervical spondylotic myelopathy
Intermittent neck and shoulder pain [Cervical pain] is the most common complaint in cervical spondylosis.
The pain is often accompanied by stiffness, with radiation into the shoulders or skull.
When the degeneration causes compression of nerves it could lead to sensory and motor dysfunction [pain, numbness and weakness].
The patients with cervical pain usually have symptoms due to degenerative disc disease, pain in facet joints or ligamentous lesions leading to ligamentous instability.
- Neck pain and/or suboccipital headaches
- The pain may radiate to shoulder, scapula or arm
- The pain may interfere with sleep
Paresthesiae may accompany pain in the cervical region, the upper limb, shoulder or interscapular region. Radiation to the chest may also occur.
Cervical radiculopathy occurs due to the compression of cervical nerve roots.
The symptoms are
- Radiating pain to the upper limb when sensory fibers are affected
- Muscle weakness when there is the involvement of motor nerve fibers
Cervical myelopathy is often seen in severe spondylosis of long-standing origin. It has a different combination of symptoms consisting of a motor and sensory loss depending on the part of the cord involved.
Physical examination reveals neck stiffness and numbness in the affected root. Neural findings aer often seen in myelopathy.
Differential Diagnosis
- Cervical Myofascial Pain
- Whiplash Injury
- Brachial Plexopathy
- Normal aging associated weakness
- Vitamin B12 deficiency
Lab Studies
Lab studies are mostly not needed and are often normal.
Imaging in Cervical Spondylosis
Routine anteroposterior and lateral x-rays of the cervical spine demonstrate
[See what is normal in cervical spine x-ray]
- Loss of cervical lordosis
- Disc space narrowing
- Osteophytes
- Facet joint arthritis
- Degenerative changes of uncovertebral joints
- Endplate sclerosi
Other findings that should be looked into for there presence or absence
- Sagittal diameter
- Normal is about 17mm
- <13mm causes cord compression
Oblique view of the cervical spine is done to look for
- foraminal stenosis [Often due to uncovertebral joint arthrosis]
Flexion-extension views may be needed to detect cervical spine instability and look for compensatory subluxation above or below the spondylotic stiff segment.
MRI
MRI is not routinely done for cervical spondylosis. MRI may be indicated in cases where radiculopathy is not amenable to treatment or in cases of spondylotic myelopathy to assess cord damage.
MRI is the best modality to evaluate the health of neural structures like nerve roots and spinal cord. Therefore it has greater role in cervical radiculopathy and myelopathy than cervical pain.
It can reveal disc protrusion and provides direct imaging in multiple planes.
The findings of MRI need to be correlated clinically to avoid false-negative and false-positive results.
CT and CT Myelography
CT is useful to provide a better bony definition, osteophytes and also reveals ossification of the posterior longitudinal ligament.
CT myelography can provide a good amount of information on degrees of spinal cord compression and can be done in patients where MRI cannot be done [as in patients with metal implants or pacemakers]
Treatment of Cervical Spondylosis
The pain of cervical spondylosis and cervical radiculopathy usually resolves without intervention. The treatment includes neck immobilization, drug treatments, lifestyle modifications, and physical modalities like traction, manipulation, and exercises.
In general, the treatment of cervical spondylosis can be nonoperative or operative.
Nonoperative treatment
Neck Immobilization
Immobilization of the neck can be done by
- Soft cervical collar
- Philadelphia collar
- Rigid orthoses
- Minerva jacket [rare]
The orthoses are worn as long as long as possible during the daytime. With the improvement of symptoms, the wearing of orthoses should be during strenuous activity.
Prolonged use of orthoses may reduce muscle tone and cause neck stiffness from disuse.
Drugs
Nonsteroidal anti-inflammatory drugs are the mainstay of drug treatment for reducing inflammation and pain. Patients with chronic symptoms should receive tricyclic antidepressants like amitriptyline.
Muscle relaxants such as thiocolchicoside, tizanidine, carisoprodol, and cyclobenzaprine may help patients with neck spasms.
Use of opioid drugs is restricted to patients who are not relieved with the above drugs or do not tolerate nonsteroidal anti-inflammatory drugs or have moderate-to-severe pain due to significant structural spondylosis.
Gabapentin and pregabalin are also effective on nerve pains.
Lifestyle Modification
Lifestyle modifications include
- Posture improvements
- Ergonomic changes in the workplace
- Neck relaxation methods to avoid strain on cervical spine techniques to avoid strain on the cervical spine.
Other Measures
- Physical therapy
- Neck strengthening
- Balance and gait training
- Cervical traction
Surgical Treatment
Surgery is indicated in patients with
- Intractable pain [Pain that is not responding to treatment]
- Progressive neurologic deficits
- Documented compression of nerve roots or of the spinal cord
The aim of surgical treatment is decompression of the neural structures/spinal cord and fusion of the unstable spine.
The choice of surgical method depends on the site and extent of the compression. These are
- Foraminotomy
- Anterior cervical discectomy with fusion
- Cervical disc replacement
Laminoplasty is a procedure used for cervical myelopathy.
References
- Kuo DT, Tadi P. Cervical Spondylosis. StatPearls. 2020 May
- Kuijper B, Tans JT, van der Kallen BF, Nollet F, Lycklama A Nijeholt GJ, de Visser M. Root compression on MRI compared with clinical findings in patients with recent-onset cervical radiculopathy. J Neurol Neurosurg Psychiatry. 2011 May. 82(5):561-3.