Last Updated on November 21, 2023
Compression fractures of the spine are fractures where there is a reduction of vertebral body height due to the collapse of the vertebra.
These are also called vertebral compression fractures. Most of these fractures occur in the lower thoracic and lumbar regions.
Injuries to the spine, osteoporosis, and malignancy are the most common causes of compression fractures.
These fractures have a bimodal distribution.
In young and middle-aged adults, trauma is the main cause of these injuries such as motor vehicle injuries and fall from height. Most of these fractures are seen in the thoracolumbar region.
In elderly people, most compression fractures are due to osteoporosis and may occur with insignificant or no trauma. These are seen in the lumbar, thoracolumbar and thoracic region.
Malignancy and infections like tuberculosis may also cause these fractures.
Relevant Anatomy and Biomechanics
The vertebral column is formed by the stacking of vertebrae from below the skull to the end region of the spine called the coccyx. There are 7 cervical, 12 thoracic, and 5 lumbar vertebrae from above to below.
Thoracic and lumbar vertebrae are most commonly involved in compression fractures.
A compression fracture mostly involves the anterior half of the body of the vertebra. As neural structures are posterior to the body.
Therefore, most of the compression fractures do not have any kind of neural deficit.
Only, the burst fractures which involve almost completely the body of the vertebra have the risk of injuring neural structures.
The vertebral bodies are separated by a gel-like structure called intervertebral disc.
The spine enables humans to walk upright. The proper posture is maintained by normal curvatures of different spinal regions.
Normally, the cervical spine has lordosis, the thoracic spine has kyphosis and the lumbar spine has lordosis.
Any injury that changes the shape of a vertebra will alter the posture, changing the curve.
When it occurs in one region say the lumbar, the body in an attempt to compensate for the change, will tend to distort the curves of the thoracic and cervical spine and increase load on other joints like hips and sacroiliac joints.
In addition to being a source of pain, compression fractures, thus, can alter the mechanics of the posture.
Mechanism of Compression Fractures
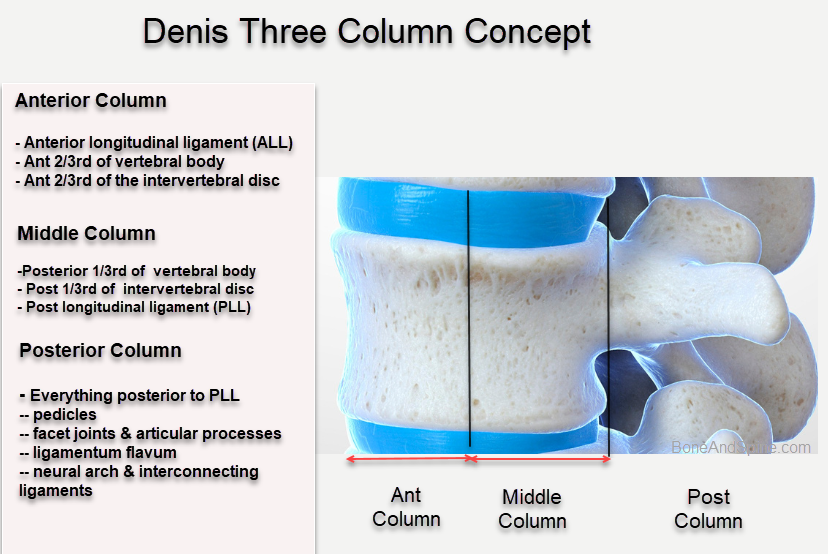
The mechanism of traumatic compression can be understood by knowing Denis’ 3-column anatomic theory. These columns are
- Anterior column
- Middle column
- Posterior column
The traumatic compression fractures involve the anterior column only. The involvement of the middle column causes burst fracture. Most of these fractures are caused by axial loading.
According to Denis’s system injury to the single column is stable and injury to more than one is not.
Compression fractures lead to wedging of the vertebra as the vertebra gets compressed anteriorly. Such fractures are also termed as wedge fractures.
These fractures occur as a result of an axially directed central compressive force combined with an eccentric compressive force. An axial force that is more than what the vertebra can tolerate results in compression fracture. A greater force results in a burst fracture.

The middle column remains intact and acts as a hinge.
Wedge fractures are usually symmetric but about 8-14% of Wedge fractures are asymmetric. These are called lateral wedge fractures.]
Nontraumatic fractures occur in weakened bone when even a minor fall on the tailbone, causing an axial load or flexion, results in one or more compression fractures.
Spontaneous fractures under physiologic loads are also known.
Causes of Compression Fractures
The compression fractures of vertebrae can occur for the following reasons. Trauma and osteoporosis are the main causes.
- Trauma
- in young patients
- Osteoporotic fractures
- in elderly
- Occur with minor trauma
- Spontaneous fractures may occur
- Malignancy
- Multiple myeloma
- Lymphoma
- Metastases
- Infection
- Tuberculosis
- Bacterial infection
Clinical Presentation
The presentation is dependent on the mode of injury.
Young people who injure their back in trauma have a spectrum of presentations that would vary from isolated non-radiating back pain when trauma is mild, to severe back pain and other injuries in case of high-energy injury.
Osteoporotic fractures may present with backache after an insignificant fall or without any trauma. The patient usually complains of pain in the back.
Often, the patient does not any pain in osteoporotic fractures and these are incidentally found on spine X-rays.
Often osteoporotic fractures are found on x-rays onlyIn osteoporotic fractures in the elderly, there could be no pain.
pathological fractures from malignancy and infection would have associated symptoms and could be preceded by a period of backache before the acute exaggeration due to the fracture event.
On examination, the patient typically has a kyphosis that cannot be corrected. in acute injuries, this kyphosis deformity is often tender.
Apart from local examination of deformity and ascertaining its level clinically, a detailed neurologic examination is done. This is normal in most of the cases of compression fractures. if a neural deficit is encountered, there is a likelihood of a burst fracture and should be ensured.
Another possible reason, though rare could be injury at a different level. The level of the neural deficit would guide us in the location of the injury.
[It is important to verify the absence of neural deficit as procedures like vertebroplasty are contraindicated in the presence of neural deficit.
Lab Studies
For most traumatic and osteoporotic fractures, lab studies are normal. In pathological fractures, the pathology would guide what lab test is required to be done.
Imaging
imaging is the mainstay of the diagnostic workup. These help define the fracture, identify the number of levels involved, and the presence of insult to neural structures if any.
X-rays

Anteroposterior and lateral views of the thoracic and lumbar spine are the usual views needed. X-rays should evaluate the entire spine because multiple spine levels are affected in 20%.
Compression wedge fractures are typical by their appearance. There is a wedge-shaped vertebra visible because of the decrease of the vertebral height anteriorly.
Burst fractures, in contrast, have the whole vertebral body fractured and therefore, the height of the whole vertebral body is decreased.
The anteroposterior view may show increased interpedicular space in burst fractures.
CT
CT helps to evaluate fractures in detail and is able to reveal the fractures not readily seen on X-rays.
One is also able to visualize the amount of spinal canal compromise.
All patients with wedge fractures > 50% loss of vertebral height should undergo CT scanning to rule out middle column injury and burst fractures.
CT also allows good visualization of the posterior element and neural arch injuries.
MRI
MRI is indicated in the presence of neurologic motor or sensory loss. It should also be done in the presence of radicular pain and suspected canal compromise.
MRI allows the visualization of the neural structures of the spine and by using contrast can reveal hemorrhage, tumor, and infection with great sensitivity.
DEXA or DXA or DRA
Dual-energy x-ray absorptiometery or radiographic absorptiometry [DXA or DRA] is used to measure the bone mineral density in cases of osteoporotic fractures. It is not an absolute requirement though it helps to label the fractures as osteoporotic compression fractures when a doubt about bone quality exists.
It can also be used to assess the response to treatment.
Treatment of Compression Fractures
Nonoperative Treatment
Nonoperative treatment consists of pain relief, bracing, and rehabilitation.
Traumatic, stable wedge compression fractures are treated by
- Initial rest
- Pain relief drugs
- Mobilization with a spinal brace as the patient is able to tolerate
- 4- 12 weeks
- Brace removal on clinical and radiographic evidence of healing
Osteoporotic compression fractures are treated with similar brace and pain relief. Treatment for osteoporosis is also initiated. In these cases too, early mobilization is desirable.
Weight-bearing and spine extension exercises are the main exercises.
Fractures need to be monitored over the course of the treatment as some fractures are known to worsen over the period.
Operative Treatment
The aim of surgical treatment is to reduce pain, decompress the spine if required, and early mobilization.
Indications for surgery are
- Worsening of symptoms on Conservative treatment
- Spinal instability
- Severe pain that does not improve or that worsens with time.
- Radiological
- Significant kyphotic deformity on plain radiographs
- Disruption of the interspinous ligaments on MRI.
- Movement of the fracture fragments on dynamic X-rays
- Unrelenting pain
- Presence of neural deficit
The surgical procedure used depends on the following factors
- Severity of fracture
- Degree of bony canal compromise
- Kyphotic deformity
- Level of fracture
- Neural deficit
- Health status of the patient
Compression fractures rarely require instrumented stabilization. the common consideration for these patients is cement augmentation in the form of vertebroplasty or kyphoplasty.
In vertebroplasty, a form of cement polymer is injected into the fractured vertebral body. This provides a better resistance to physiologic loads when the patient is upright and therefore reduces pain.
Kyphoplasty is similar to vertebroplasty but a balloon is used to expand the volume of the fractured segment before introducing the cement polymer. This Extrusion of cement into the spinal canal is less likely with kyphoplasty as the cement is delivered into a closed balloon.
Read more about vertebroplasty and kyphoplasty
The procedures are contraindicated when canal compromise is present.
References
- Denis F. The three-column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine. 1983 Nov-Dec. 8(8):817-31.
- Urrutia J, Besa P, Piza C. Incidental identification of vertebral compression fractures in patients over 60 years old using computed tomography scans showing the entire thoracolumbar spine. Arch Orthop Trauma Surg. 2019 Nov;139(11):1497-1503. [Link]
- Parreira PCS, Maher CG, Megale RZ, March L, Ferreira ML. An overview of clinical guidelines for the management of vertebral compression fracture: a systematic review. Spine J. 2017 Dec;17(12):1932-1938. [Link]