Last Updated on October 29, 2023
Congenital scoliosis is the curvature due to the imbalance of growth of the spine caused by the presence of vertebral defects.
Congenital scoliosis is the most frequent congenital deformity of the spine, the two others being congenital kyphosis and congenital lordosis.
The prevalence of congenital scoliosis is estimated at 1-4%.
Causes and Associations
Most of the cases occur spontaneously. Genetic causes have been suggested but there is uncertainty about it.
It is believed that there is an insult to the fetus during embryological development of the spine between the 5th and 8th week of gestation. Therefore, there is a frequent association of other malformations such as congenital heart disease, spinal cord dysraphism, or kidney malformations etc.
Most of the cases are not hereditary. However, cases with syndromic associations (Jarcho-Levin, spondylocostal dysplasia) or multiple defects of segmentation can have a hereditary factor.
Maternal diabetes, maternal exposure to valproate [an antiepilpetic drug] and alcohol are thought to be responsible.
Maternal hypothermia is also suggested to be a causative factor.
Congenital scoliosis may occur in isolation or with associated conditions like cardiac defects [10%], genitourinary defects [25%] and spinal cord malformations like diastematomyelia.
Association with following underlying syndromes has been noted.
- VACTERL Syndrome [38-55%]
- Goldenhar/OculoAuricularVertebral Syndrome
- Jarcho-Levin Syndrome/Spondylocostal dysostosis
- Klippel-Feil syndrome
- Alagille syndrome
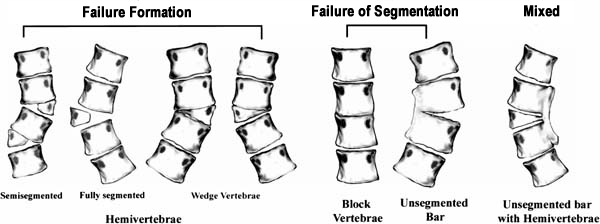
Classification of Congenital Scoliosis
Failure of Formation
- Fully segmented hemivertebra
(has normal disc space above and below) - Semisegmented hemivertebra
(hemivertebra fused to adjacent vertebra on one side with disk on the other) - Unsegmented hemivertebra
(hemivertebra fused to vertebra on each side) - Incarcerated hemivertebra
(found within lateral margins of vertebra above and below) - Unincarcerated hemivertebra
(laterally positioned) - Wedge vertebra
Failure of Segmentation
- Block vertebra
(bilateral bony bars) - Bar body
(unilateral unsegmented bar is common and likely to progress)
Mixed
- Unilateral unsegmented bar with contralateral hemivertebra
The deformity produced by a failure of formation is much more difficult to predict than that caused by the failure of segmentation.
The patient is evaluated as per routine spinal evaluation first. In addition, specific findings should be looked for in congenital scoliosis
Problems in Congenital Scoliosis
The five major problems in congenital scoliosis are
- Trunk deformation
- Trunk decompensation
- Truncal shortening
- Altered neurology
- Other congenital anomalies
The major target site for deformation in congenital scoliosis is the vertebral bone itself.
Trunk Deformation
Trunk deformation arises out of growth imbalance on the two sides of the spine. The reason for this growth imbalance is structural –
- Presence of wedge or hemivertebrae on one side of the spine
- Presence of an unsegmented bony bar with or without contralateral hemivertebrae.
Unilateral unsegmented bar with a convex hemivertebra produces the most progressive curve followed by a unilateral unsegmented bar and a double convex hemivertebra. Thoracolumbar curves have maximum progression, followed by lower thoracic and upper thoracic regions. The least severe scoliosis is caused by a block vertebra.
The site of the bony anomaly is important as lower thoracic and thoracolumbar curves have a larger propensity to increase. Upper thoracic or cervical scoliosis has a high visibility and becomes a cosmetic problem much earlier.
Hence it is important to identify the structural defect responsible for the spinal deformity.
Truncal Decompensation
A solitary hemivertebra located strategically may give rise to truncal decompensation. This happens at the junctional zones e.g. the lumbosacral junction (patient has oblique take off), the thoracolumbar or cervicothoracic junction.
Large rigid curves may show poor compensation above or below the curve.
Trunk balance is an important aspect to be considered in treatment planning.
Truncal Shortening
Due to reduced growth potential, truncal shortening may be visible. Secondarily due to early spinal fusion the truncal height may be reduced. However, a short straight trunk is better than a deformed one. We have currently no means available to increase truncal height and this remains a research area
Neural Problems
Congenital scoliosis is characterized by a high incidence of intraspinal problems ranging up to 30% in some series. These comprise pathologies like those of diastematomyelia, fibrous splitting of the cord, low filum terminale, cord or root tethering, etc. These may be responsible for altered neurological signs prior to treatment. They also have important implications for surgical treatment e.g. distraction instrumentation. This may demand rectification of the intraspinal pathology prior or along with the definitive surgical treatment.
Other congenital anomalies
The VATER association and presence of other anomalies e.g. cardiac or genitourinary may have a bearing on treatment and all congenital scolioses need to be evaluated for the presence of other congenital problems.
Diastematomyelia, tethered cord, spinal cord tumor, kyphosis, Arnold Chiari malformation and syringomyelia in the spine are frequently associated abnormalities. Apart from this congenital heart defects, pulmonary dysfunction, cor pulmonale and back pain can be associated.
Presentation and Diagnosis
The patient presents with deformity of the back. Subtle deformities may not be seen unless the patient is evaluated for some other reason.
In addition to the routine spinal evaluation, some specific physical findings should be sought in patients with congenital scoliosis.
- Hair patches, lipomata, dimples, and scars may indicate an underlying vertebral defect and should be looking for.
- A complete neurological evaluation should be done.
- Clubfoot, calf atrophy, absent reflexes, and limb atrophy could be signs of neurological involvement or associated anomalies
Prenatal ultrasound may sometimes pick the deformity though in most cases the exact diagnosis cannot be made.
Presence of associated conditions such as spina-bifida, or heart, urogenital or other syndromic malformations can alert the radiologist.
After birth, the deformity may be found on routine chest x-rays done for any other reason.
Otherwise, the deformity might be picked by the family or pediatrician.
Presence of a hairy patch or a skin hemangioma in the midline, or sacral dimple should raise the suspicion of an underlying congenital malformation. Findings such as a foot malformation or a leg asymmetry, or urinary symptoms and an unusual and rigid curve should include spine examination to look for a malformation.
The examination of the patient includes measurement of the balance of the trunk and shoulders.
The former is measured by dropping a plumb-line from C7 and the skull whereas the latter is checked by using a spirit level.
The curve is assessed for rigidity. Rib hump if any is evaluated.
Look for associated malformations like any foot or leg asymmetry, any craniofacial malformation, a Klippel-Feil web neck, and cardiac and urinary malformations.
A thorough neurological examination is done.
Age, remaining growth, presence of other congenital defects and neurological status are important in clinical examination. A thorough clinical and radiological evaluation should include analysis of the type and site of a vertebral anomaly, trunk balance, presence of laminar defects and signs of occult dysraphism, etc.
Work up includes
- Standing whole spine X-rays**
- Anteroposterior and lateral radiographs
- Serial x-rays would tell about the progression of the curve with the legs in extension and the pelvis level, to compensate for any leg length discrepancy
- Can differentiate between failure of segmentation or formation
- Measurement of the Cobb angle
- Cervical spine X-rays [ to rule out a Klippel-Feil or a cervical hemivertebra]
- Spot views of the malformation
- Thin slices CT with reconstruction
- Magnetic resonance imaging
- Mandatory before surgery
- Spinal cord anomalies like [seen in 40% of the cases]
- Tethered cord
- Diastematomyelia
- Syrinx
- Chiari malformation
- MRI with cartilage sequences provides the best quality pictures of the cartilage end-plates for the best information on growth potential
- Chest cage X-rays
- To look for rib synostosis in thoracic curve
- Ultrasound
- For renal abnormalities
- Cardiac echography for any associated cardiac malformation
**Can be compared with x-ray at birth, if available
Treatment of Congenital Scoliosis
Treatment consists of either observation of the curve or surgery. Bracing is ineffective and rarely indicated.
Observation
A non-progressive curve with a balanced spine may be just observed. The objective evidence that goes in favor of non-progressive curve is
- Incarcerated hemivertebrae
- Nonsegmental hemivertebrae
- Some partially segmented hemivertebrae
Bracing
Bracing in congenital scoliosis is inefficient.
Bracing when used is considered for
- Long flexible curves
- To control the compensatory lumbar curve
- To help to rebalance the spine
- After surgery until the fusion is solid.
bracing now is not indicated in the primary treatment of congenital scoliosis.
Operative Treatment
Surgery remains the main treatment in congenital scoliosis.
Operative management is indicated for congenital scoliosis in the following situations
- Progressive increase in deformity
- Trunk decompensation
- Neural deficit
Following operative procedures are used in the treatment of congenital scoliosis
Posterior fusion with or without bar osteotomies
The procedure is indicated in
- Hemivertebrae opposite a unilateral bar that does not require a vertebrectomy at any age. Fusion is done to stop the progression.
- Older patients with worsening of the condition
- Significant progression
- Neurologic deficits,
- declining respiratory function
- To prevent the crankshaft phenomenon and thus obviate the need for an anterior fusion.
Anterior/posterior spinal fusion with or without Vertebrectomy
It is indicated in
- Young patients with worsening of the condition
- Significant progression
- Neurologic deficits,
- declining respiratory function
- Girls < 10 yrs, Boys < 12 yrs
- Failure of formation with contralateral failure of segmentation at any age that requires hemivertebrectomy and/or significant correction. T
Distraction based growing-rod construct
- For controlling deformity during spinal growth and delay arthrodesis
- Need to be lengthened approximately every 6 months for best results
Osteotomies between ribs.
- More than four fused ribs
- Risk of potential for thoracic insufficiency syndrome
Hemivertebrectomy
This procedure is usually indicated in 3-8 years of age in the presence of progressive or significant deformity
Hemiepiphysiodesis
This procedure is in indicated in patients with intact growth plates on the concave side of the deformity. The patients are younger than 5 years with a curve less than 40-50 degrees.
Spinal column shortening resection
It is indicated in patients with deformities that present late and have severe decompensation. It is also indicated in rigid severe deformities or fixed pelvic obliquity.
Prognosis
Congenital scoliosis progresses most rapidly in the first 3 years of life. The progression is determined by the morphology of the vertebrae.
Rate of progression in decreasing order is seen as
- Unilateral unsegmented bar with contralateral hemivertebra[greatest, 5-10 degrees/year]
- Unilateral unsegmented bar
- Fully segmented hemivertebra
- Unincarcerated hemivertebra
- Incarcerated hemivertebra
- Unsegmented hemivertebra
- Block vertebrae [least, less than degrees/year]