Last Updated on November 11, 2019
Coxa vara describes a deformity of the hip where the angle formed between the head and neck of the femur and its shaft is decreased, usually defined as less than 120 degrees. This angle is also known as Mikulicz angle.
It can be congenital or acquired. The common mechanism in congenital cases is a failure of medial growth of the physeal plate.
As coxa vara is a symptom of many diseases, it is usually classified according to the condition which causes it.
Relevant Anatomy
Read about proximal femoral anatomy here.
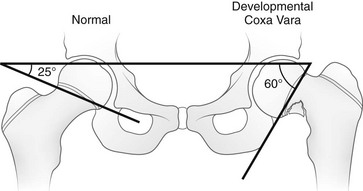
Adult femoral shaft and femoral neck make an angle that ranges between 120 degrees to 140 degrees.
If this angle is more than 140 degrees, one is said to have coxa valga. Conversely, a decrease in this normal neck—haft angle to <120 degrees, coxa vara is said to be present.

In anatomical positions, the neck is depressed than normal. The depression of the neck results in a certain mechanical disadvantage. The normal apposition between the joint surfaces is lost since the head of the femur no longer accurately fits the acetabulum.
The trochanter is displaced upwards, and hence, during the abduction, is liable to imping on the side of the pelvis.
The marked shortening of the limb leads to a waddling gait, not unlike that of congenital dislocation of the hip.
Classification of Coxa Vara
- Idiopathic:
- Congenital – mild or severe coxa vara, with associated congenital anomalies
- Developmental – progressive, usually appearing between 2-6 years
- Mucopolysaccharidoses (e.g. Morquio’s disease)
- Dysplasia epiphysealis multiplex
- Cleidocranial dysostosis
- Rachitic – usually associated with active rickets
- Adolescent: secondary to slipped capital femoral epiphysis
- Traumatic – usually following fracture of the femoral neck (rare in children)
- Inflammatory – secondary to tuberculosis or other infection
- Secondary to other underlying bone diseases such as:
- Osteogenesis imperfecta
- Cretinism
- Dyschondroplasia
- Paget’s disease
- Osteoporosis
- Fibrous dysplasia
- Severe osteoarthritis
- Legg-Perthes’ disease
Associations
- Congenital dislocation of hip – developmental hip dysplasia
- Faulty development of the femur
- Craniocleidodysostosis
- Camptodactyly arthropathy coxa vara pericarditis syndrome
Clinical Presentation
The patient is brought because of abnormal painless gait or limp. Patient walks with Trendelenburg limp in unilateral coxa vara and a waddling gait in bilateral coxa vara.
Following findings can be seen on examination
- Limb length discrepancy
- Prominent greater trochanter
- Limitation of abduction and internal rotation of the hip.
- Patients may also show femoral retroversion or decreased anteversion.
Imaging
X-rays
The recommended views are anteroposterior view of the hip with limb internally rotated.
Findings are
- Neck-shaft angle <120 degrees
- Increased Hilgenreiner’s epiphyseal angle (normal <25 degrees)
- Determined on AP view of the pelvis as the angle between Hilgenreiner’s line [Line drawn horizontally through the inferior aspect of both triradiate cartilages.] and a line through the proximal femoral physis
- Triangular metaphyseal fragment in the inferior femoral neck. It appears as inverted-Y radiolucency
- Decreased femoral anteversion

CT
- CT along with 3D image reconstruction is done to plan for surgery, mark proximal femur defects and gauge the orientation of deformity.
- It helps to find deformity configuration, bone stock, and physeal widening
Treatment of Coxa Vara
Treatment objective is to restore the neck-shaft angle so that the epiphysial plate is restored to decrease shear forces and promote ossification of the femoral neck defect. The treatment is corrective osteotomy.
Indications for surgical intervention are
- Neck – shaft angle < 90 degrees
- Progressive deformity.
- Vertical physis and a significant limb length discrepancy
- HE angle> 60 degrees
Patients with HE angle 45 – 60 degrees is closely followed up. Patients with HE angle < 45 degrees are known to have spontaneous resolution.
A valgus osteotomy reduces the deformity, normalize the neck-shaft angle, improves the gluteal forces, improves joint congruency and increases limb length to reduce the limb length discrepancy.
Congenital Coxa Vara
Coxa vara may be primary congenital deformity or may occur in association with other congenital.
The patient is usually small in stature and limps, and, in bilateral cases, rather resembles a patient with congenital dislocation. Often there is pain and stiffness. On examination, the greater trochanter is on a level higher than the normal, with consequent shortening, while there may be a flexion contracture present.
Radiographic features are
- The angle of the neck is reduced to something below a right angle.
- The neck varies in length but is short and may even be non- existent
- The head is unusually translucent and may be fluffy in outline.
- Acetabular deformity due to the malposition of the head.
- In extreme cases, greater trochanter curves inwards and may articulate with the ilium above the acetabulum.
Untreated, it can result in severe deformities and disability.
Treatment is a corrective osteotomy. This involves a wedge removal with the base on the lateral side.