Last Updated on August 2, 2019
Elbow instability refers to a laxity in the elbow joint that may cause the joint to catch, pop, or slide out of place during certain arm movements.
It most often occurs as a result of an injury — typically, an elbow dislocation.
The instability associated with elbow injury is called acute elbow instability whereas the instability that is presented over a period and occurs, again and again, is called recurrent/chronic.
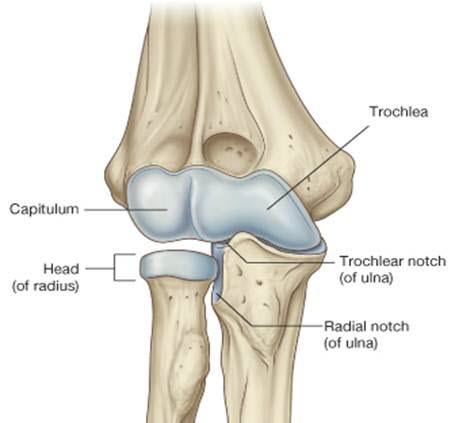
Relevant Anatomy of Elbow
The elbow joint has three bony articulations: ulnohumeral, radiocapitellar, and proximal radioulnar. Stability of the elbow is maintained by these bony articulations, capsuloligamentous and musculotendinous structures.
At the extremes of motion, specifically at less than 20° and greater than 120° of elbow flexion bony stabilizers are most important, while the lateral and medial ligamentous complexes are the primary stabilizers throughout the remainder of the motion arc. [see the list of stabilizers given below]
The lateral ligament complex is Y-shaped and is comprised of four ligaments
- The radial collateral ligament (RCL)
- Lateral ulnar collateral ligament (LUCL)
- Accessory ligament
- Annular ligament
The lateral ulnar collateral ligament is deemed to be the most important restraint to varus stress, though other parts are also considered to play an important role.
The inherent stability of the elbow relies on a combination of bony articulations and soft tissue restraints.
The coronoid is the most important stabilizer to anterior and posterior translation. It forms a buttress against posterior dislocation of the ulna on the humerus. It also provides attachment to the anterior medial collateral ligament, the middle third of the anterior capsule and the deep head of the brachialis.
The medial collateral ligament (MCL) complex has three components: the anterior, the posterior and transverse bands.
The anterior band is the most important restraint to elbow valgus and the posterior band is the primary restraint to pronation of the ulna on the humerus.
Stabilizers of the elbow
The elbow has both static and dynamic stabilizers
Static Stabilizers
Primary Stabilizers
- Ulnohumeral articulation
- Medial collateral ligament
- Lateral collateral ligament
Secondary Stabilizers
- Radial head
- The common flexor and extensor origins
- The capsule.
Dynamic stabilizers
- The muscles that cross the elbow joint
- Anconeus- preventing postero¬lateral rotational displacement of the elbow
- Triceps – posterior
- Brachialis – anteromedial
- An elbow with its three primary constraints intact will be stable.
If the coronoid process is fractured or lost, the radial head becomes a critical stabilizer.
- Normal elbow carrying angle: males: 5-10 degrees; females: 10-15 degrees
- Normal range of motion: 0-150 degrees flexion/extension, 80 degrees supination, 80 degrees pronation
- Functional range of motion of the elbow: 30-130 degrees of flexion/extension and 50 degrees of pronation and 50 degrees of supination.
- In full extension, 60% of axial load is transmitted through the radiocapitellar joint
Acute Elbow Instability
Acute elbow instability usually develops after injuries involving the bony or ligamentous stabilizers of the joint.
Usually, it is associated with dislocation or fracture-dislocation of the elbow but can occur after isolated valgus or varus overloading can also be leading to ligament ruptures.
Untreated, acute instability may lead to chronic instability.
The injuries of the elbow especially those associated with dislocation need to be managed well to avoid the lingering instability.
Severe injuries are evident. Injuries of lesser degree will be revealed by bruising and swelling on the medial or lateral aspect of the elbow, suggesting an acute injury to the underlying structures. Tenderness to palpation will further suggest injury.
Further, the range of motion is documented and stress tests are if the severity of the injury allows.
Crepitus during movement is may suggest an osteochondral fragment or fracture. A neurovascular examination must also be performed.
Imaging
Plain x-rays [AP, lateral and oblique views] should be done. Presence of bony injuries should be noted. If bony injuries are not visualized, draw a line drawn through the long axis of the radius. In a well contained joint, should intersect the capitellum on all views.
Computed Tomography is useful for further assessment of fractures in terrible triad injuries
Treatment
The injuries should be treated depending on the nature of the injury.
After the fractures or dislocations have been treated, the limb should be assessed for post-treatment elbow stability. Any instability should be documented and contemplated whether treatment is required or just rehabilitation would take care of the instability. Few of injuries are discussed below
After closed reduction has been performed the elbow is examined and plain radiographs are taken. If the elbow is stable through the full range of motion and a congruent reduction is seen on x-rays, the patient is given a broad arm sling for comfort and is encouraged to mobilize the elbow.
Surgery is seldom necessary in the management of a simple posterior dislocation.
The indications for surgery include
- Failure to obtain and maintain a congruent reduction
- Persistent instability of the elbow joint requiring immobilization beyond 30–45° of flexion
- Suspected entrapment of intra-articular fragments or the median nerve in the joint.
In acute elbow instability, ligament repair may be undertaken for the indications.
The hinged external fixator is used most commonly as a secondary device to protect surgically repaired or healing structures while permitting and assisting proper kinematic motion.
The three primary indications are: (1) persistent instability in association with an acute fracture-dislocation despite attempted ligament repair and fracture fixation or radial head replacement, or both; (2) gross acute instability in a patient who is not a candidate for surgery; and (3) delayed treatment (approximately four weeks or more after the time of injury) of a dislocated and stiff elbow.
In most cases, the patient has one or more of the following features:
- High-energy injury
- Previous failed attempts at reduction or surgical repair of the dislocation
- Multidirectional instability on examination after attempted or achieved reduction
- Concomitant fracture of the radial head or the coronoid process, or both (the terrible triad of the elbow).
Chronic or Recurrent Elbow Instability
The lateral collateral ligament is the essential lesion leading to elbow instability. This insufficiency gives rise to recurrent posterolateral rotatory instability which is the most common type of chronic elbow instability.
Types of Chronic or Recurrent Elbow Instability
There are three different types of recurrent elbow instability.
Posterolateral rotatory instability
There is an injury to the lateral collateral ligament complex resulting in looseness of the joint. It is the most common type of recurrent elbow instability.
It may develop following trauma, as a result of a previous surgery, or longstanding elbow deformity.
Valgus instability
There is an injury to the ulnar collateral ligament, which is a soft tissue structure located on the inside of the elbow. Valgus instability is most often caused by repetitive stress as seen in overhead athletes as in baseball pitchers. It may also be caused by trauma resulting in medial disruption.
Varus posteromedial rotatory instability
There is an injury of the lateral collateral ligament complex along with the fracture of the coronoid portion of the ulna bone on the inside of the elbow. Varus posteromedial rotatory instability is usually caused by a traumatic event.
As the posterolateral rotatory instability is the most common type of instability, it is the instability being discussed in detail hence further.
Posterolateral Rotatory Instability
Pathoanatomy of Chronic Elbow Instability
Instability of elbow is a spectrum of presentation, at the farther end of which is dislocation of the elbow. Elbow instability occurs due to disruption of soft tissue or bony stabilization.
In a usual course, it usually begins on the lateral side of the elbow, often initiated by trauma and progresses to the medial side in three stages.
It can be classified into the following stages
Stage 1
the lateral collateral ligament is partially or completely torn. There is posterolateral rotatory subluxation of the elbow, which can reduce spontaneously
Stage 2
Stage 2 also involves additional disruption anteriorly and posteriorly.
It may result in incomplete posterolateral dislocation of the elbow. This subluxation can be reduced with the use of minimal force or by the patient manipulating his or her own elbow.
Stage 3
It is further subdivided into three parts.
Type 3A
All or the soft tissues around and including the posterior part of the medial collateral ligament are disrupted, leaving only the important anterior band (the anterior medial collateral ligament) intact. This permits posterior dislocation by a posterolateral rotatory mechanism.
The elbow pivots on the intact anterior band of the medial collateral ligament. The reduction can be achieved by gentle manipulation.
This stage is mostly seen in the fractures of the radial head and coronoid process.
Type 3B
The entire medial collateral complex is disrupted. Varus, valgus, and rotatory instability are all present following reduction.
Type 3C
The instability is so severe that the elbow can dislocate even when it is immobilized in a cast in 90 degrees of flexion. This degree of instability means that the entire distal aspect of the humerus has been stripped of soft tissues.
Thus, the dislocation is the final stage of three sequential stages of elbow instability resulting from posterolateral ulnohumeral rotatory subluxation, with the soft-tissue disruption that progresses from the lateral to the medial side.
This is also known as the circle of Horri.
Clinical Presentation
Most of the patients would have a preceding history of trauma. Sometimes the problem is quite obvious, as the patient is able to demonstrate the instability but it may be more subtle. Sometimes the patient has noticed only pain and discomfort and is not aware of instability. Additional symptoms include painful catching, slippage, or clicking with flexion and extension. A feeling of slippage of the joint in and out of place may be reported by the patient.
The patient usually presents with pain, mechanical symptoms or a decreased level of performance in sporting activities.
There may be a history of recurrent elbow subluxation or dislocations, with each subsequent dislocation requiring less force. B
The symptoms are usually produced in the extension half of the arc of motion with the forearm in supination.
Apprehension sign
These can be demonstrated in two ways.
- The patient performs a floor push up with the elbow fully supinated.
- The patient pushes up on the arms of a chair to stand, again with the elbow fully supinated.
In both tests, a subjective feeling of apprehension, instability or frank dislocation is considered positive for posterolateral rotatory instability.
Pivot-shift maneuver
It is also known as posterolateral rotatory instability test.
The patient is positioned supine on the examination table with the arms overhead, the shoulder in full external rotation to stabilize the shoulder joint and the forearm in full supination.
From the extended and supinated position, the examiner brings the arm from extension to flexion, a valgus stress is placed on the elbow and the forearm is allowed to be less supinated. This allows the forearm to pivot around the anterior bundle of the medial ulnar collateral ligament and results in a reduction of the elbow joint as the triceps becomes taught at around 40° of elbow flexion, often causing an audible or palpable clunk.
Apprehension during the lateral pivot shift maneuver is often considered to be a positive test even without frank instability
Varus stress-testing may suggest a lateral collateral ligament insufficiency.
Imaging
X-rays
An anterior-posterior and a true lateral view should be obtained on every patient. The congruency of the joint is noted.
On anteroposterior radiographs or there is a slight widening of the radiohumeral joint.
On lateral radiographs, the radial head may appear to be situated posterior to the capitellum. Lateral ligament laxity can be identified on the true lateral view from the “tilt sign” which is a subtle widening of the trochlea/trochlear notch interval.
Fluoroscopy
Fluoroscopy allows the surgeon to observe any joint space widening in real time, whilst a varus or valgus force is applied to the elbow.
CT/MRI
These are important in assessing assess fractures and intra-articular fragments. MRI may help to identify ligamentous and cartilaginous injuries.
Arthroscopy
In some instances, when the presentation does not suggest the injury or the findings on the physical examination are not convincing, or when there is a possibility of an intra-articular lesion, arthroscopic examination of the elbow may be helpful. Arthroscopy will reveal the laxity of the radiohumeral joint and thus confirm the lesion.
An arthroscopic evaluation of the ulnohumeral joint can demonstrate joint space widening during varus/valgus and rotational stresses.
Normal elbow the olecranon– trochlea articulation will open enough to allow a probe medially and laterally. In posterolateral rotatory instability, the arthroscope can be introduced between the trochlea and trochlear notch.
Base on arthroscopy, the instability can be divided into three groups.
- Isolated posterolateral rotatory instability – requires a lateral repair or reconstruction.
- Posterolateral rotatory instability combined with medial instability – requires a global reconstruction.
- Posterolateral rotatory instability with joint degeneration – Needs consideration of the joint stability and its articular surface.
Management of Posterolateral rotatory instability
The broken ligament does not become stable over time, except possibly when a patient is seen in the very early stages. Therefore a recurrent problem requires a surgical construction.
The reconstruction should be isometric, extracapsular and anatomical, using an autogenous graft from hamstring graft or palmaris longus tendon.
After repair, the elbow is placed in 70 to 80 degrees of flexion with the forearm in full pronation. The arm is held in this position for ten to fourteen days, and then the patient is permitted protected motion in a hinged brace for two to six weeks, with flexion allowed as tolerated. After six weeks, the patient may remove the hinged splint for sedentary activities, but otherwise, the splint is worn for most activities and is discontinues at the end of an additional six weeks.
In the setting of chronic dislocations and secondary surgery, comminution, malunion and bone loss may make the coronoid fracture irreparable. In this situation, an osteochondral graft may be required.
References
- S. Bell. Elbow instability, mechanism, and management. Current Orthopaedics, 22 (2008), pp. 90-103
- S.W. O’Driscoll, J.B. Jupiter, G.J. King, R.N. Hotchkiss, B.F. Morrey. The unstable elbow. J Bone Joint Surg Am, 82 (2000), pp. 724-725
- D.T. Leonello, I.J. Galley, G.I. Bain, C.D. Carter. Brachialis muscle anatomy. A study in cadavers.J Bone Joint Surg Am, 89 (2007), pp. 1293-1297
- L.M. Reichel, G.S. Milam, S.E. Sitton, M.C. Curry, T.L. Mehlhoff. Elbow lateral collateral ligament injuries. J Hand Surg Am, 38 (2013), pp. 184-201
- J.A. Hall, M.D. McKeePosterolateral rotatory instability of the elbow following radial head resection.J Bone Joint Surg Am, 87 (2005), pp. 1571-1579.
- B.P.H. Lee, L.H.Y. TeoSurgical reconstruction for posterolateral rotatory instability of the elbow. J Shoulder Elbow Surg, 12 (2003), pp. 476-479
- B.S. Kim, K.H. Park, H.S. Song, S.Y. ParkLigamentous repair of acute lateral collateral ligament rupture of the elbow. J Shoulder Elbow Surg, 22 (2013), pp. 1469-1473
- K.-Y. Lin, P.-H. Shen, C.-H. Lee, R.-Y. Pan, L.-C. Lin, H.-C. Shen. Functional outcomes of surgical reconstruction for posterolateral rotatory instability of the elbow.Injury, 43 (2012), pp. 1657-1661.