Last Updated on October 27, 2023
This article focuses on hip osteoarthritis. For details on Osteoarthritis, read Osteoarthritis Symptoms, Diagnosis and Treatment
Hip osteoarthritis is common and can result in severe pain and disability. It can make it hard to do everyday activities like bending over to tie a shoe, rising from a chair, or taking a short walk.
It is a chronic disease and takes months to years to appear and gradually worsens over time. Earlier detection and intervention is important to lessen its impact on life. It cannot be cured but treatment can help the patients manage pain and stay active. Most people with osteoarthritis of the hip can be managed without surgery.
Hip osteoarthritis can be primary or secondary.
Primary osteoarthritis of hip is said to occur when there is no antecedent cause. In secondary osteoarthritis, there is a preceding cause like old trauma.
It occurs most often in people 50 years of age and older, though it may occur in younger people, too.
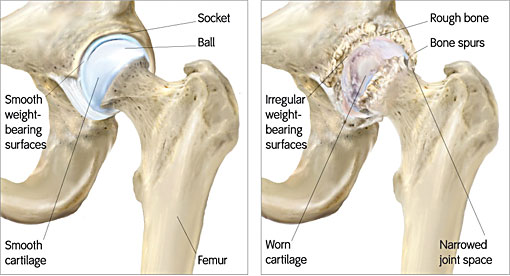
The hip is a “ball-and-socket” joint. The socket is formed by the acetabulum, and the ball is the femoral head, which is the upper end of the femur.
The bone surfaces of the ball and socket are covered with articular cartilage, a smooth, slippery substance that protects and cushions the bones and enables them to move easily.
The surface of the joint is covered by a thin lining called the synovium. In a healthy hip, the synovium produces a small amount of fluid that lubricates the cartilage and aids in movement.
Read detailed Anatomy of Hip
Causes and Risk Factor of Hip Osteoarthritis
In osteoarthritis, the cartilage in the hip joint gradually wears away over time. As the cartilage wears away, it becomes frayed and rough, and the protective joint space between the bones decreases. The damaged bones may start to grow outward and form bone spurs or osteophytes.
Osteoarthritis develops slowly and the pain it causes worsens over time.
Risk factors that may increase the likelihood of hip osteoarthritis
- Genetics.
- Developmental hip dysplasia
- Legg-Calve-Perthes Disease
- Slipped capital femoral epiphysis
- Avascular necrosis of Hip
- Hip impingement or femoroacetabular impingement
- Severe trauma to the hip
Presentation of Hip Osteoarthritis – Symptoms and Signs
Pain and stiffness are the main symptoms of hip arthritis. Usually, the pain develops slowly and worsens over time. Sudden onset of pain can also occur. Pain and stiffness may be worse in the morning, or after sitting or resting.
When it becomes more advanced joint deformities and leg-length inequalities may result.
The typical pain from hip arthritis is located in the groin thigh or buttock. The pain may even radiate to the knee.
Pain may flare up with vigorous activity. Locking or sticking of the joint, and a grinding noise may be reported. This occurs due to movement caused by loose fragments of cartilage and other tissue.
As arthritis worsens, the symptoms can become more persistent or more severe and can remain even after the activity stops.
Limp may occur with advanced diseases and ability to walk is affected as well.
Osteoarthritis of the hip can affect one’s ability to walk, climb stairs, enter or exit a vehicle, sit or arise comfortably, perform housework and enjoy one’s day-to-day activities.
On examination, the hip joint may be tender. The patient would have painful gait or in case of shortening, short limb gait.
Sometimes, crepitus may be felt with hip movement. Depending on the severity of the disease, the movement may be painful in some arc of motion. Generally, extremes of motion are found to be painful.
Many patients indeed find that the chronic pain associated with osteoarthritis of the hip does contribute to fatigue.
Osteoarthritis of the hip does not affect metabolism but some patients attribute weight gain to the inactivity that results from the hip pain caused by osteoarthritis of the hip.
Differential Diagnoses
There are many other pathologies that can affect the hip that can present in a similar manner.
- Spinal stenosis
- Greater trochanteric bursitis
- Osteonecrosis of hip
- Rheumatoid arthritis.
Imaging
Xray is basic imaging procedure and provides enough information to diagnose and differentiate osteoarthritis. Both anteroposterior and lateral views are sought. Reduction of joint space, osteophyte formation, the absence of osteopenia, and the presence of subchondral sclerosis are features that suggest the presence of hip osteoarthritis.
Xrays are able to reveal other bony changes such as avascular necrosis etc.
MRI is able to reveal mild arthritis even before it is visible on plain x-rays. But the clinical utility of early diagnosis is not cost-effective.
MRI has a very well defined to rule out soft tissue involvement, bone tumors, infection, and avascular necrosis.
Treatment
There is no cure for osteoarthritis, there are treatment options that relieve pain and improve mobility. Most of the patients do well with nonsurgical treatment.
Non-surgical Treatment
Lifestyle modification
Lifestyle modification aims to reduce the stress on the hip joint. Following measures are adopted-
- Reduce activities that aggravate the condition, such as climbing stairs.
- Switching from high-impact activities like jogging to lower impact activities like swimming or cycling)will put less stress on your hip.
- Weight reduction
- Change of job – light duty alternative to heavy manual labor
Exercises
Specific exercises can help increase the range of motion and flexibility, as well as strengthen the muscles in your hip and leg. A physical therapist can help to individualize the exercise program.
Aids
Walking supports like a cane, crutches, or a walker can improve mobility and independence. Similarly to avoid bending a long-handled reacher to pick up low-lying things will help.
Leg-length inequalities can be managed with a shoe lift.
Drugs
Drugs may be added for those who are not relieved by non-pharmaceutical means and pain is affecting daily routine, or is not relieved by other nonsurgical methods, your doctor may add medication to your treatment plan.
Acetaminophen [Paracetamol] is the first drug to be used. NSAIDs like ibuprofen and diclofenac can also be used. Prolonged use ain relievers have cause side effects and should be judiciously used under the supervision of a doctor.
Glucosamine and chondroitin are helpful to some patients although the literature is equivocal about their use.
Intra-articular steroids are also used to relieve pain. These are prescribed and injected by a qualified doctor. These appear to be less useful for hip arthritis than they are for arthritis. This probably is because hip joint is a deep joint and difficult to locate.
Injection of hyaluronic acid in the joint is also called viscosupplement injections. Hyaluronic acid is a component of the normal joint fluid. Commercially prepared injections are available for use.
Surgical Treatment
Total hip replacement is the most common and very successful surgery for painful hip and hip osteoarthritis. This involves the removal of the damaged acetabulum, removal of the femoral head, and replacement by the implant.