Last Updated on August 2, 2019
Intramedullary nailing of the bone involves the use of an intramedullary nail or rod to fix the fractured bone.
It is called intramedullary nailing because a metal rod forced into the medullary cavity of a bone to fix the fractures. Intramedullary nailing is commonly used to fix the long bone fractures. As of today, there are many types of nails available. Nails made for specific fracture patterns are also available now. For example Recon nail for fracture of the subtrochanteric region.
An intramedullary nail functions as a form of the internal splint which stabilizes long bone fracture with minimal damage to the surrounding soft tissues. Because they are sturdy and usually approximately round in shape, they withstand the heavy load of the body well in any direction, rather like the bone itself. Limbs with nailed fractures may be mobilized early after surgery with weight bearing before the bony union.
Küntscher nail has been used commonly but now is more of historical importance. It was a nail with triangular or cloverleaf cut-section without any locking mechanism. Gerhard Küntscher is credited with the first use of this device in 1939, during World War II.
Most of the modern nails come with a locking mechanism. Locking is a process of fixing the nail to the bone using premade holes in the nail both on the proximal and distal end of the nail for a stable fixation.
Nails which can be locked are called interlocking nails.
Nails are made of stainless steel and titanium
Locked intramedullary nailing is the standard today.
Modern nailing is a technique whereby the nail is inserted into the bone from one end whilst not disturbing the fracture site at all under an X-ray image intensifier.
Biomechanics of Intramedullary Nailing
The length of a nail that transmits the load from one main fragment of a fractured bone to the other is known as the working length. The stiffness of a nail in both rotation and bending is related inversely to its working length.
The longer the working length, the greater the relative movement between the main bone fragments.
Nails may be either solid or hollow. Solid nails are stronger than hollow ones of the same diameter simply because they have more metal for their volume.
Hollow nails are less stiff in bending than solid ones, although their stiffness may be altered by making the walls thicker or thinner. The thicker the wall the stronger and stiffer the nail.
The advantage of having a somewhat flexible nail is that it will have a little “give” in it on insertion which will make it easier to put in and will let the nail to deform slightly to conform to the natural shape of the bone. This slight flexibility does not affect the rigidity of the nail to support the broken bone.
Very stiff nails may damage the bone if there is any discrepancy between the nail of a shape and that of the bone.
Note: Nails are of a standard shape but people are not, even after reaming.
One way of reducing stiffness is to put a longitudinal slot in the wall of a nail. This makes it much more flexible but does so at the cost of it losing overall bending strength and torsional strength.
Nail design, like that of any engineering structure, is always a compromise between including as many desirable properties as possible whilst trying to keep undesirable properties to a minimum.
Nails are curved according to the bone involved and slotted along their length. The wall thickness of 1.2 mm and the slot give an optimal balance between strength and flexibility and permit good contact between nail and femur when the nail is not locked.
Advantages of Nailing over Plating
Intramedullary nail, biomechanically, offer several advantages over plate and screw fixation-
- Intramedullary nails are subjected to smaller bending loads than plates and are thus less vulnerable to fatigue failure. This is because the intramedullary canal is closed to the central axis of the femur than the usual plate position on the external surface of the bone.
- Intramedullary nails act as load- sharing devices in fractures that have cortical contact of the major fragments. If the nail is not locked at both the proximal and distal ends, it will act as gliding splint and allow continued compression as the fractures are loaded.
- Stress shielding with resultant cortical osteopenia, commonly seen with plates and screws, is avoided with intramedullary devices.
- Refracture after implant removal is rare with the use of intramedullary devices
- The intramedullary implant does not usually require the extensile exposures required for plate application. With the use of image intensification, these devices can be implanted in a “closed” manner, without exposing the fracture site. These closed techniques result in low infection and high union rates, with a minimum of soft tissue scarring.
Indications for Intramedullary Nailing
Femur and tibia are bones where nails are most commonly and successfully used. The ideal indications for nailing are:
- Transverse and short oblique fractures of the tibial and femoral shafts.
- Comminuted fractures of tibia and femur, provided cross locking facilities are available.
- Pathological fractures
- Delayed or non-union of femur or tibia.
- Selected open fractures
In children, as the nail may damage growth plates and should be avoided.
Technique of Interlocked Intramedullary Nailing – General Points
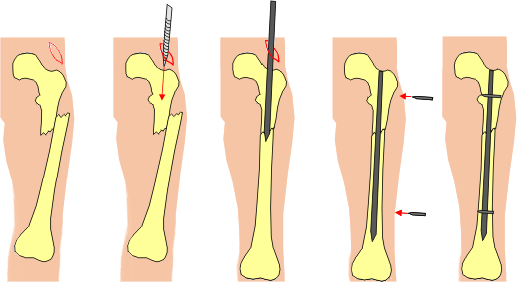
Image credit: rob.cs.tu-bs.de
Entry Point
Nails are inserted at the one end of the bone, generally, proximal end into the intramedullary cavity, travel across the fracture site to reach the other end.
This point where nail enters the bone is called the entry point. In femur, this is piriformis fossa or tip of the greater trochanter.
Initially, a small hole is made using a bone awl or drill and gradually enlarged with reamers to accommodate the nail diameter.
Guidewire Insertion
Guide wires are thin wires which are inserted in the intramedullary canal after initial entry point is made with awl or drill.
The guide wire is pushed into the medullary cavity through the entry hole made. Its position is ascertained by C-arm image intensifier.
Guide wires are passed through fracture fragments till the other end of the bone is reached.
Reaming
Using cannulated reamers, the intramedullary cavity is reamed to increase the size of the cavity. Reamers could be manual or power reamers. The reaming is done over the guide wire which guides the reamer and protects it from getting astray in the bone.

Depending on the final reamer size allowed by bone, the diameter of the nail is chosen which generally is smaller by one size.
For example, if we can ream till size 11mm, the desired nail size would be 10mm in diameter.
It is pertinent that the fracture fragments should be aligned while reaming is done.
Fracture Reduction and Nail Insertion

After length and diameter of the nail is determined, the nail is assembled with its inserting jig and inserted over the guide wire [in case of hollow nails, in solid nails guide wire needs to be removed before nail insertion.]
The nail could also aid in the reduction of the fracture.
Locking
Interlock nails have two holes at either end. A hole is drilled into the bone at the right angle to the nail. It passes through the hole in the nail and then drills the opposite cortex. When a bolt is passed through this, it engages cortices on either side while engaging the nail hole too, thus locking nail and bone together.

The introduction of paired holes which align at right angles to the long axis of a nail permits cross locking to give axial and rotational stability.
Holes may be round, as they are usually at the distal end, to accommodate a screw or bolt. The holes are slightly bigger than the thread diameter of either bolt to allow smooth gliding through the nail.
Following image illustrates the concept of dynamization very well.

Some proximal holes may instead be oval-shaped slots. This permits slight axial movement of the bone but still prevents rotation.
This allows increased bone contact during loading and encourage callus formation and rapid healing. The process is called dynamization.
Proximal locking is achieved by passing bolts through the aligned holes across the nail guided by a jig which attaches into the top of the nail.
Locking in the distal screw holes of the nail is achieved under X-ray image intensification.
Routine removal of screws later in fracture treatment to ensure dynamization is seldom necessary as the natural flexibility of the nail is sufficient to stimulate callus formation.
Concept of Unreamed Nailing
Some authors contend that reaming damages the interior blood supply of the bone. If a fracture is extensive and there is a lot of soft tissue damage, there is a risk that the outer blood supply will also be impaired. At best this will delay healing and at worst may lead to bone death.
By using a smaller solid nail, reaming may be avoided.
The concept of an undreamed nail as a way of stabilizing open fractures in cases where such severe damage to the blood supply is a distinct possibility is now being actively explored.
Instrumentation for Interlocked Intramedullary Nailing
Nail and bolts constitute the implants. Nails of all sizes should be kept on the table for a particular case. Preoperative length could be measured by measuring the contralateral bone length.
Each nail has its own instruments and these are generally not interchangeable. Major instruments are as below
Guide wires

A guide wire is used to provide an initial crossing of the fracture site after the medullary canal of the fractured bone has been opened. It provides alignments and is essential to facilitate the passage of the reamers.
There are two types of the guide wire, each with a different diameter.
One of the wires has a blunt bulbous tip so that reamers cannot pass beyond the end of this guide wire. It is called beaded guide wire. [Shown in the image above]
Beyond the bulbous stop, the guide wire is slightly bent to 15 degrees. By rotating it during the insertion process a degree of manipulative control may be achieved when trying to cross the fracture site.
The second wire has no bead at the tip and inserted after reaming before the actual insertion of the nail as otherwise, the nail may snag on the bulbous tip when the guide wire is extracted.
In the femur, the thin guide wire is 3mm in diameter and the thicker one 4mm. not that in the tibial set the bulbous tipped and plain ended guide wires are both 3mm in diameter.
Reamers

There are two sorts of reamers with different cutting ends.
The first reamer of 9mm diameter has a front cutting end to force an initial passage down the medullary canal of the bone.
The rest of the reamers are side cutting and are used to widen the pilot hole. They come in o.5mm increments and because they are side cutting will get jammed unless used sequentially without missing out any steps.
Flexible shafts are constructed of wound coils of wire and are designed to rotate only in one direction. Under no circumstances should they be reversed or the wire will uncoiled.
Cross bolt guides
Also proximal cross bolts can be placed without the image intensifier using an outrigger jig.
The distal holes positions can vary as the nails tend to twist slightly. The holes, therefore, will not always be in the expected plane.
C-arm image intensifier is required for distal holing [Some nail companies do provide jig which may often produce the desired results]
Universal Femoral Nail
It is called universal to indicate that the nail can be used unblocked and has a side to side symmetry so that it may be used in either the left or the right femur.
Proximally, there is one hole and another slot, providing an ability to lock in static [using round hole] or dynamic [using slots]
The nail has a “cloverleaf” cross-section which maintains good contact with the bone whilst preventing excessive nail distortion when twisted.
The nail comes in different outer diameter from 9mm to 13mm.
The wall of the nail is The wall is 1.2mm thick which balanced strength and flexibility
There is a continuous longitudinal slot that makes the nail flexible and deformable enough to make contact with the bone.
The upper end has a conical “female” threads in it to accommodate a conical “male” threaded bolt, used to attach the insertion and extraction devices
The nail has a curvature which corresponds to part of the circumference of a circle which has a radius of 1500 mm, which reflects the average shaped femur.
Universal Tibial Nail

It is also called universal for the same reasons as described for the femoral nail.
It has a different overall shape and a range of dimensions that are slightly different from the femoral nail.
Shape
The tibial nail has a bend one-third of the length of the nail so that the nail can be inserted from a point on the anterior surface of the tibia behind and slightly to one side of the patellar tendon. It is called Herzog’s notch or bend.
The entry canal, on average, makes an angle of eleven degrees with the tibial medullary canal. This is the angle built into the shape of the nail.
Holes
The holes in the universal tibial nail differ from those in the femoral nail in that there are three holes at the bottom, two orientated in the coronal plane and one in the sagittal plane. Some nails also come with three proximal holes.
Bolts
For tibial nails size 8 mm, the bolts are smaller in size. These bolts are 3.9 mm as compared to 4.9 bolts used for bigger tibial and femoral nails.
Complications of Intramedullary Nailing
- Compartment syndrome
- Infection
- Implant Failure
- Fractures near metaphyses
- Smaller diameter nail used
- Early weight-bearing
- Shortening
- Often due to dynamic interlocking with excessive weight-bearing
- Limb length inequality < 1.2 cm – no intervention
- Higher values may need corrective measures
- Malunion
- Malrotation> 10 degrees
- Varus/ valgus angulation > 7 degrees
- Anteroposterior angulation > 10 degrees
- Heterotopic Ossification
- Soft tissues irritation over entry points [usually longer sized nail]
Save