Last Updated on September 29, 2023
Lumbar discography is an invasive diagnostic procedure that involves, the instillation of iodinated contrast into the nucleus pulposus after inserting a needle under fluoroscopy. This procedure is done with the aim of getting information on the morphology and integrity nucleus pulposus, vertebral endplates, and annulus fibrosus.
In addition to this, the measured contrast injection allows the determination of intradiscal pressures and the response of the patient to this stimulation is a measure of pain caused by disc.
Chronic low back pain is a very common occurrence.
Quite often, it becomes difficult to locate the source of pain given the complex nature of spinal structures. The intervertebral disc is a common pain generator in about forty percent of cases.
Many patients complain of low back pain but have no structural abnormalities on MR imaging. Discography is a diagnostic option that may link a patient’s subjective complaints of spinal pain to symptomatic disk disease.
Thus lumbar discography not only defines the anatomical architecture of the disc but also tells whether a particular disc is painful.
Relevant Anatomy and Pathophysiology
The cervical, thoracic, and lumbar vertebrae are stacked together and separated by a soft tissue called intervertebral disc. The disc specifically lies between vertebral bodies [vertebral bdy forms the anterior part of the vertebra]
The posterior half of the vertebra consists of the spinous process and the lamina and pedicles connect the posterior and anterior portions.
Thus vertebra is anteriorly connected to the adjacent vertebra via a disc whereas posteriorly facet joints act as the connectors.
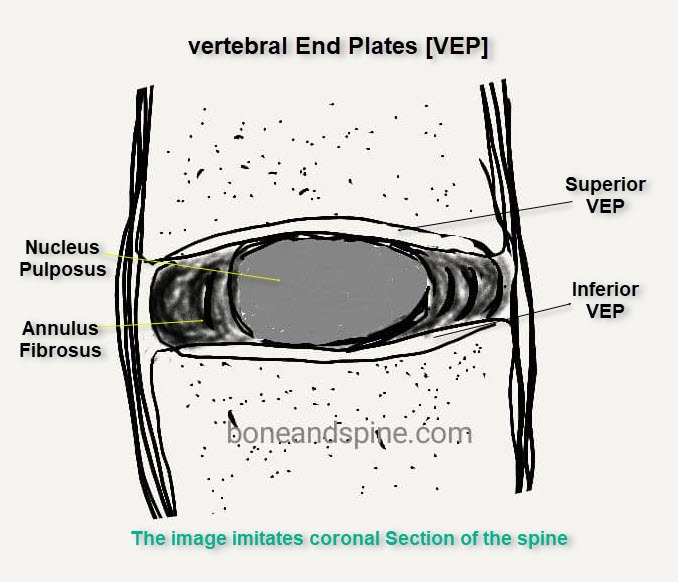
Each vertebra is connected to the disc via vertebral end plates which also act as a medium of nutrition.
 The intervertebral discs are complex structures that consist
The intervertebral discs are complex structures that consist
- The thick outer ring of fibrous cartilage, the annulus fibrosis
- A more core is known as the nucleus pulposus.
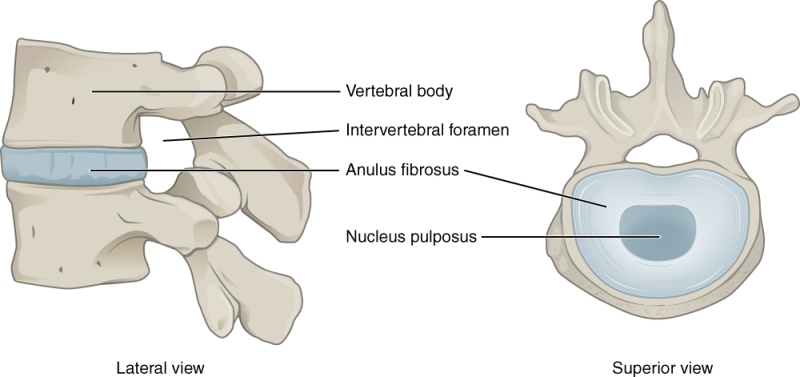
The intervertebral discs are approximately 7–10 mm thick and 4 cm in diameter in the lumbar region
The anterior and posterior, innervate and supply the annulus fibrosus in the anterior part and posterior part of the disc respectively.
The degeneration process leads to disc dehydration and desiccation of the nucleus. Often it is not symptomatic.
Weakening and tearing of the annulus occur due to repetitive loading and degeneration. This causes nuclear material to touch the passing nerve roots causing pain. Disc herniation may occur releasing inflammatory factors. The stimulation of pain receptors in the following may cause pain of discogenic origin.
- Posterolateral annulus
- Ligamentum flavum
- Posterior longitudinal ligament,
Alterations in the internal structure and metabolic function of one or more discs lead to painful discs.
Basis of Lumbar Discography
Lumbar discography is done to establish and confirm discogenic pain.
Lumbar discography provokes pain by the following mechanisms. An increase of intradiscal pressure by the injection of contrast material into the disc may increase
- Neurochemical stimulation that causes pain
- An increase in intravertebral pressure.
Lumbar discography is not indicated or necessary to confirm the unequivocal presence of herniated discs that coincide with findings on clinical examination.
Indications of Lumbar Discography
It should be noted though that in most of the cases clinical examination and magnetic resonance imaging can identify the offending disc with sufficient certainty and discography is not routinely needed.
Lumbar discography should be performed only if adequate attempts have failed to reveal the etiology of the back pain.
Lumbar discography should be considered when surgery is being considered and all the following conditions are met
- Pain for > 3 months
- Pain is not improving with conservative measures
- No evidence of
- Stenosis
- Intraspinal obstruction
- Infection
- The pain of psychogenic origin
Lumbar discography can be considered in any of the following
- Severe pain that is highly likely to be discogenic and needs surgery
- Failed back surgery
Contraindications
- Any bleeding disorder
- Patients on anticoagulation therapy
- Pregnancy
- Infection over the puncture site
- Known allergies [Risk of allergic reaction to contrast medium]
- Mental illnesses
- Sever canal compromise
- Uncooperative patient because of severe pain or other reasons [The desired position may not be obtained]
How Lumbar Discography Is Done?
Obtain a thorough history of the patient and ask for the exact location of his/her pain. The patient should complete a pain diagram. The amount of back pain compared with buttock pain and leg pain should be noted. Allergy to contrast is noted and the need for prophylactic medications is addressed.
Anticoagulants should be stopped at an appropriate time. For example, warfarin is stopped about 5 days prior to the procedure.
Blood pressure and pulse oximetry should be monitored throughout the procedure.
The patient should be awake to provide feedback of pain. Mild sedation may be used in anxious patients.
Procedure
After obtaining intravenous access, fluid is started. The patient may be given prophylactic antibiotics.
The patient is placed in the desired position.
- For the lateral approach- decubitus position [person lies on the side]
- For the posterolateral approach- Lateral, slightly oblique, rotated forward, and at a 45° angle to the bed.
For this text, we are using the posterolateral approach.
The back is cleaned with betadine and prepared.

The fluoroscope is positioned.
A local anesthetic (1% lidocaine) is infiltrated to the skin and musculature at the right paramedian region of the desired level.
A 3.5-inch spinal needle of 18 gauge is inserted at the same location as where the anesthetic was given, pointing it slightly to the lateral to superior articular process and at a midpoint between the endplates, as visualized in fluoroscopy.
The stylet is removed and a 22-gauge 7-inch spinal needle is inserted through the previously positioned needle under fluoroscopic guidance. ideally, it should pass lateral to superior articular process and medial to exiting nerve root. Slight resistance is encountered at the annulus. The final position of the needle tip should be in the center of the disc space on both of these views for the needle to be in pulposus.
Water-based iodine contrast [iodohexol] is injected with a pressure syringe and the following are noted
- opening pressure
- at the onset of pain,
- maximum pressure
Pressure values can indicate the integrity of the disc.
A typical nonpainful lumbar disc should be able to hold pressure up to at least 90 psi.
- If there is no pain till this pressure, the disc is negative for pain.
- A pain occurs below 50 psi, the disc is likely the source
- Pain occurring below 15 psi indicates chemical sensitivity of the disc
- Between 50-90 psi, other sources of pain should be looked
The patient is questioned for the location, intensity, and quality of pain produced by injection of the material and should quantify pain as follows
- P0- No pain on injection
- P1- Partial concordant (pain partially covers the area of the usual pain)
- P2- Discordant pain (pain in a different area than the usual pain)
- P3- Concordant back pain (pain covers the same distribution of the usual pain)
Videotaping during discography is of both of the disc injection phases and the patient’s facial expression can help the surgeon to determine the response and mannerisms. Exaggerated pain mannerisms may suggest poor surgery-related outcomes.
Attention should be paid to note whether the pain is similar to or exactly like the symptoms for which the patient seeks relief. The location of the pain and its intensity should be noted.
Inference
Pain at low pressures is mostly due to chemical irritation. If low resistance is encountered, a tear through the annulus should be suspected. Pain at high pressures is generally due to mechanical irritation, end-plate deflection, or stimulation of pressure receptors.
If a large volume of contrast can be injected, the disc has degenerated or there is a fissure extending through the outer annular wall.
Complications of Lumbar Discography
Complications associated with lumbar discography include
- Discitis
- Accidental intradural injection
- Damage to the disk
- Urticaria
- Retroperitoneal hemorrhage
- Nausea
- Seizures
- Increased pain
In rare cases, discography has been found to result in disk herniations
References
- Carragee EJ, Lincoln T, Parmar VS, Alamin T. A gold standard evaluation of the “discogenic pain” diagnosis as determined by provocative discography. Spine. 2006;31(18):2115–23. [PubMed]
- Carragee EJ, Alamin TF, Miller JL, Carragee JM. Discographic, MRI, and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain. Spine J. 2005;5:24–35. [PubMed]