Last Updated on August 2, 2019
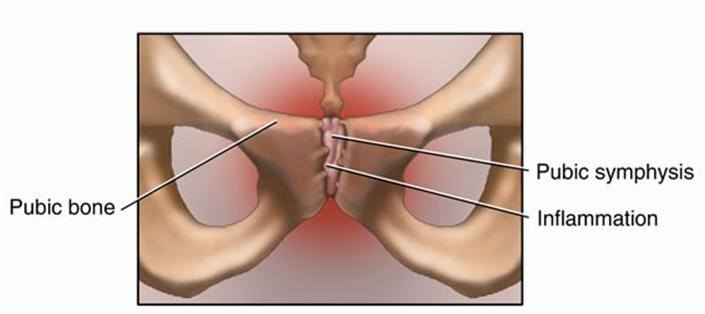
Osteitis pubis is an inflammation of the pubic symphysis and surrounding muscle insertions and is characterized by sclerosis and bony changes of the pubic symphysis. It is a known complication of pelvic surgeries and also occurs in athletes.
it is rarely encountered in the children. Men are more infected and the disorder is most commonly seen in the age group 30-50 years.
Pathophysiology of Osteitis Pubis
The pubis is part of the innominate bone of the pelvis. The pelvis is a ring, and any change in the anatomy or in the forces applied to one area of the ring may result in increased stress and pain at another. For example, sacroiliac joint motion has a very large impact on the motion about the pubic symphysis
The hip adductors (ie, the gracilis, adductor longus, adductor brevis, and adductor magnus) originate at the inferior pubic ramus. The pectineus and rectus abdominis muscles, along with the inguinal ligament, insert superiorly. The muscles of the peroneal floor insert posteriorly.
Read more on innominate bone anatomy
Read more on pelvis anatomy
Osteitis pubis is most likely caused by repetitive microtrauma or shearing forces to the pubic symphysis..
Osteitis pubis seems to be more prevalent in sports that involve running, kicking, or rapid lateral movements such as soccer, sprinting, ice-hockey or American football.
Running and rapid change of direction and kicking are frequent movements in these sports and can lead to strains of the adductor muscles, and abnormal forces across the pubic symphysis.
Apart from athletic activities, conditions associated with osteitis pubis include the following-
- Pregnancy and childbirth
- Gynecologic surgery
- Urologic surgery
- Major trauma
- Repeated minor trauma
- Rheumatologic disorders
Clinical Presentation
There is the complaint of pain over the symphysis and may radiate to the surroundings such as the groin, scrotum, perineum, medial thigh, hip, or abdomen etc
Athletes may present with adductor pain or lower abdominal pain that then localizes to the pubic area. Pain can be of abrupt or insidious onset and is often exacerbated by walking, climbing stairs, coughing, or sneezing.
A clicking or popping sensation when rising from a seated position, turning over in bed, or walking on the uneven ground may be noted.
When sacral innominate dysfunction is a cause, the SI joint pain may be there.
On examination, there is tenderness over the pubic symphysis. Pressing both pubii few centimeters laterally to each side may cause pain [pubic spring test]
An inguinal hernia should be checked.
In affected female athletes, a gynecologic examination should be performed to rule out raising the suspicion of pelvic inflammatory disease
Differential Diagnosis
- Adductor Strain
- Femoral neck fracture
- Osteomyelitis
- Pelvic inflammatory disease
- Prostatitis
- Sacroiliac Joint Injury
- Urinary tract infection
- Ankylosing spondylitis (rare)
Lab Studies
CBC should be obtained to rule out systemic infection. Counts are generally norma. Urinalysis is be performed to rule out an etiology of a urinary tract infection or prostatitis.
A blood culture can be done in febrile patients but are often negative.
Febrile patients with negative blood cultures should go for aspiration of the pubic symphysis.
Imaging
X-rays
In early osteitis pubis, x-rays do not have any finding. Widening of the pubic symphysis may be seen on anteroposterior view after a few weeks.
Sclerosis and osteolysis occur in later stages.
Erosions if the visible point to osteomyelitis.
Pubic instability is seen when stress views are taken [Flamingo views]. It is defined as > 2 mm of cephalad translation of the superior pubic ramus on standing one leg.
Bone Scanning, SPECT
Bone scanning or single-photon emission computed tomography detect the disease early.
MRI/CT
This helps to distinguish between muscle, tendon, periosteal, and bony lesions.
Treatment of Osteitits Pubis
Rest for a prolonged period is the mainstay of the treatment. For symptomatic relief heat or ice may be used. An assistive device like crutches and orthoses (eg, a lumbar/sacral corset or a sacroiliac belt) may be given to unload the pelvis for pain relief and to maintain correct anatomic alignment.
The recommended duration of rest ranges from 2 weeks to 3 months and a further period of refraining from sports for 3-6 months.
NSAIDs are given for pain control. The oral corticosteroid may be added in severe cases.
Corticosteroid injection at the site is beneficial but is rarely required.
Physical therapy is started early in the treatment and aims to restore flexibility and control pain.
It includes ultrasound, electrical stimulation, ice massage, and exercises. Exercises include stretching and strengthening of hip and abdominal muscles, hamstring, and quadriceps.
Surgery is rarely required is generally reserved for those in whom conservative management fails. Curettage, arthrodesis, wedge resection, and wide resection of the pubis are surgical procedures.
Surgery can lead to early improvement of symptoms but may cause posterior pelvic instability and necessitate a second surgical procedure for stabilization.
Ideally, return to play should occur only when the patient is pain-free with all activity.
Prevention of Osteitis Pubis
- Flexibility
- Proper body mechanics
- Sacroiliac dysfunction treatment
- Early recognition and treatment
Prognosis
With definitive diagnosis and treatment, the prognosis for osteitis pubis is excellent.
In most cases, osteitis pubis resolves with rest though it may take up to 8-10 months and in some cases more. Few patients may have recurrence and chronic pain.
The major complication is a muscle-tendon injury of the adductor muscles.
References
- Fricker PA. Osteitis pubis. Sports Med Arthrosc Rev. 1997. 5:305-12.
- Batt ME, McShane JM, Dillingham MF. Osteitis pubis in collegiate football players. Med Sci Sports Exerc. 1995 May. 27(5):629-33.
- Angoules AG. Osteitis pubis in elite athletes: Diagnostic and therapeutic approach. World J Orthop. 2015 Oct 18. 6 (9):672-9.
- Holt MA, Keene JS, Graf BK, Helwig DC. Treatment of osteitis pubis in athletes. Results of corticosteroid injections. Am J Sports Med. 1995 Sep-Oct. 23(5):601-6.
- Paajanen H, Hermunen H, Karonen J. Pubic magnetic resonance imaging findings in surgically and conservatively treated athletes with osteitis pubis compared to asymptomatic athletes during heavy training. Am J Sports Med. 2008 Jan. 36(1):117-21.
- Kunduracioglu B, Yilmaz C, Yorubulut M, Kudas S. Magnetic resonance findings of osteitis pubis. J Magn Reson Imaging. 2007 Mar. 25(3):535-9.
- King JB. Treatment of osteitis pubis in athletes: results of corticosteroid injections. Am J Sports Med. 1996 Mar-Apr. 24(2):248.
- Mehin R, Meek R, O’Brien P, Blachut P. Surgery for osteitis pubis. Can J Surg. 2006 Jun. 49(3):170-6..
- Radic R, Annear P. Use of pubic symphysis curettage for treatment-resistant osteitis pubis in athletes. Am J Sports Med. 2008 Jan. 36(1):122-8