Last Updated on November 20, 2019
Phalanx fractures are common hand injuries. Phalanges are small long bones of the hand that make our fingers and thumb.
A similar arrangement of bones is also found in toes and those bones are also called phalanges.
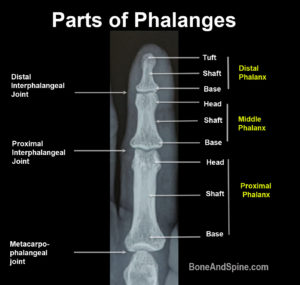
Each finger is formed by three phalanges.
- Proximal phalanx
- Middle phalanx
- Distal phalanx
Thumb has only two phalanges, proximal and distal.
Phalanx fractures account for 10 % of all the fractures.
Phalanx fractures are found twice as common in males than females.
Distal phalanx fractures are most common, followed by middle and proximal phalanx.
Little finger accounts for almost 40% of the cases.
Injuries due to sports are the most common cause in less than 30 years of age and fall after 70.
In group 40-70 years, machine injury is most common.
Nail injuries could be associated with distal phalanx fractures
Distal Phalanx Fractures
Distal phalanx fracture is most common as the distal phalanx of the hand is terminal contact of the upper limb with surroundings and is at risk of injury with nearly every use of the hand.
Distal phalanx can be divided into tuft, shaft and base.

Distal phalanx fracture can be conceived of as occurring in three primary regions [Anatomy of the distal phalanx]
- The tuft (63%)
- The shaft (36%)
- The base (18%)
Sudden axial load as in ball sports or crush injuries are mainly responsible for injuries to the distal phalanx. Fractures of the tuft are usually communicated but stable due to internal splinting by fibrous septae. However, the proximal fractures are often displaced due to due to flexor and extensor forces.
Intraarticular fractures [involving distal interphalangeal joint] occur usually due to axial loading.
Mallet avulsion fractures are caused by rupture or avulsion of the extensor tendon, often following a direct blow to the tip of the finger causing forced flexion of the distal joint. They result in mallet deformity of the finger.
The Seymour fracture is a pediatric injury of distal phalalnx which produces mallet finger type deformity and is physeal fracture.
It has an associated nail bed injury and with ungual subluxation.


Here is the view from the side

Middle Phalanx Fracture

Most of the fractures of the middle phalanx are caused by crushing injury or blunt force.
Fracture of the middle phalanx can be in the head, neck, shaft, and base of the phalanx.
Location of the fracture and the type of injury-causing it determines the pattern of the fracture.
For example, fractures of the neck have volar angulation because proximal phalanx is flexed [by flexor tendons] and the distal extends [by extensor tendons]
In contrast, those at the base would angulate in the opposite direction.
If the forces are axial, it may result in unicondylar or bicondylar fractures of the head or intra-articular fractures of the base.
Fractures of the base could have a dorsal, volar or lateral base depending on the direction of the fracture.
Intra-articular fractures involving proximal interphalangeal joints, shaft fractures [oblique, longitudinal and transverse] and fractures of the head are other injuries that occur.

Proximal Phalanx Fracture

Fractures of proximal phalanx can be
- Intra-articular
- Fractures of the head
- Fractures of the base
- Extra-articular
- Fractures of the neck
- Fractures of the shaft
- Fractures of the base
Fracture pattern can be transverse, short oblique, long oblique or spiral for shaft fractures. Intra-articular fractures can be partial or complete.

Dislocations of Interphalangeal Joints

The proximal interphalangeal joint is more commonly dislocated. Dorsal dislocations are common and are often associated with rupture of volar plate or ligament. Volar dislocations are less common and may be associated with extensor tendon rupture.
Dislocations of the DIP joint are rare and are often caused by hyperextension forces. Quite a number of them are open.
Most of the dislocations are reducible by closed methods.
Irreducible dislocations of the distal interphalangeal joint may occur due to joint occur due to
- Volar plate entrapment
- Flexor digitorum profundus is trapped behind a single condyle of middle phalanx
- Middle phalanx is buttonholed through the volar plate
- Middle phalanx is buttonholed through a rent in the FDP
- The extensor tendon is displaced around the head of the middle phalanx
Clinical Presentation
The history will guide about the mechanism of injury. A physical examination would reveal deformity and tenderness.
Neurovascular status should be assessed.
Imaging Studies
Most hand fractures are diagnosed and managed with the help of x-rays. Three views are often desired
- Anteroposterior
- True lateral
- Oblique


Treatment of Phalanx Fractures
Each of the phalangeal fractures needs to be treated on an individual basis. Fracture pattern, fracture location, whether open or closed, associated soft injuries and presence of other system injuries and whether dominant or non-dominant hand ar ethe various factors that affect the treatment.
Distal Phalanx Fractures
For nailbed injuries, please read Fingernail injuries.
Closed reduction with or without splinting works in most of the cases. Operative treatment is required in fractures which are open, displaced, not reducible or unstable.
Fractures of the base with more than 25% of joint are treated surgically. Another indication is displaced volar base fracture with large fragment.
The fracture can be fixed by longitudinal or crossed K wires, extension block pinning [for mallet finger]. Small fragments can be fixed by lag screws.
Middle Phalanx Fractures
These middle phalanx fractures are treated conservatively [buddy taping or splinting for three weeks followed mobilization]

Image Credit: About First Aid
Extraarticular fractures with no rotational deformity
- < 10° angulation
- < 2mm shortening
- Undisplaced intraarticular fractures
Surgery
Closed reduction and percutaneous pinning under C-arm image intensifier is most commonly done the procedure. Open reduction and internal fixation using miniplate or screws. The volar plate is repaired where required.
Screws ate specially indicated in long oblique fractures. Following fractures need surgery-
- Extraarticular fractures
- More than 10 degrees of angulation
- More than 2mm shortening
- Rotational deformity
- Displaced intraarticular fractures
- irreducible or unstable fractures
Proximal Phalanx Fracture
The indications of conservative or operative treatment are similar to that of the middle phalanx.
Interphalangeal Joint Dislocations
The proximal interphalnageal joint receives static stability from the proper and accessory collateral ligaments and the volar plate. It is further supplemented by the dynamic stability of the dorsal plate and balanced tendon forces acting across the joint.
Some of the dislocation may be subtle and missed. These should be diagnosed on stress views.
For collateral ligament injury with dislocation on stress views, splinting alone would suffice.
For clear cut dislocations, closed reduction and splinting for stable dislocations and closed reduction and internal fixation [kwire] for unstable ones.
Open injury and irreducible dislocation would require open reduction and internal fixation.
Other Injuries of Fingers
Mallet finger, Jersey finger and Seymour fracture have been discussed in separate articles