Last Updated on October 29, 2023
Phosphorus in body is present in organic and inorganic forms of phosphorus. Apart from ionic form, phosphorus participates in activities in form of phosphate salts. Phosphorus is present as phosphate, and these two terms are commonly used interchangeably. Phosphorus metabolism regulates serum phosphate levels.
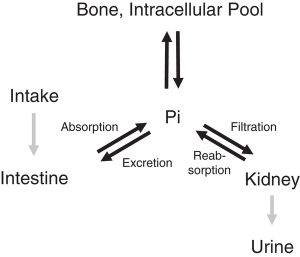
Image Credit: Nature
Like calcium, the regulation of phosphate balance is by intestinal absorption, renal excretion, and bone accretion.
Dietary phosphorus is present in abundance in most foods, unlike calcium. The body is twice more efficient for absorption of phosphorous than calcium present in the diet. Thus nutritional phosphorus deficiency is rare.
Thus, phosphorus absorption, unlike calcium, is rarely a nutritional problem. In fact, in kidney disease, a diet low in phosphate or phosphorus is recommended.
Functions of Phosphorus
Phosphorus is central to energy metabolism, intracellular signaling, and cell structure. It is stored mainly in the bones but there are stores in soft tissues also. In fact, phosphorus stores are more in soft tissues than calcium stores.
Phosphorus t makes up 1% of a person’s total body weight. It is the second most abundant mineral in the body.
The main function of phosphorus is in the formation of bones and teeth.
Phosphorus plays an active role in the metabolism of carbohydrates and fats.
It is also used in protein building by the body.
It is also used in muscle contraction and nerve signaling.
Phosphorus Rich Foods
Proteins in the diet are the main sources of phosphorus. It is found in abundance in milk and meat. Cheese, beans, soya foods fish, poultry eggs, peanuts, and lentils are other examples. Any diet that provides protein and calcium would be rich in phosphorus also.
Fruits and vegetables contain only small amounts of phosphorus.
The recommended dietary intakes of phosphorus are as follows:
- 0 to 6 months: 100 milligrams per day (mg/day)
- 7 to 12 months: 275 mg/day
- 1 to 3 years: 460 mg/day
- 4 to 8 years: 500 mg/day
- 9 to 18 years: 1,250 mg
- Adults: 700 mg/day
Pregnant or lactating women:
- Younger than 18: 1,250 mg/day
- Older than 18: 700 mg/day
Diet of a healthy adult has about 1400 mg of phosphorus in the diet. Of this, >900-mg net is absorbed.
The absorbed phosphorus enters the extracellular fluid pool and moves in and out of bone as needed.
Phosphorus Metabolism and Its Regulation
Maintaining physiological phosphate balance is of crucial biological importance for bone health. Body phosphate homeostasis is determined by regulation of intestinal uptake of dietary phosphate, renal phosphate reabsorption and excretion, and phosphate between bone and extracellular pools.
About 85% of phosphate is present in bone and teeth and about 1% in extracellular fluid. Rest is found in soft tissues.
In bones, phosphate and calcium form hydroxyapatite crystals and the remaining phosphate appears as amorphous calcium phosphate
Serum phosphate concentration varies with age. Infants have the highest concentration [normal range 4.5–8.3 mg/] as they require a higher amount for growth and build up.
The concentration decreases as the kids grow. In adults, the normal range is 2.5–4.5 mg/dL.
Phosphate serum levels are regulated by a complex set of processes occurring in the intestine, skeleton, and kidneys. The currently known main regulators of phosphate homeostasis include parathyroid hormone, calcitriol, and a number of peptides collectively known as the “phosphatonins” of which fibroblast growth factor-23 (FGF-23) has been best known.
Parathyroid hormone
The primary function of PTH is to tightly regulate serum calcium concentration. It increases proximal tubular expression of 25(OH)D 1?-hydroxylase, resulting in increased production of 1,25(OH)2D3.
This leads to
- Increased calcium absorption in the gut
- Increased calcium reabsorption in the distal convoluted tubule
- Release of calcium into the extracellular fluid by increasing osteoclastic bone resorption.
- Decrease in serum phosphate
Recent studies have indicated that probably FGF-23 acts as a counter-regulatory hormone for 1,25(OH)2D3.
Calcitriol or 1,25 Dihydroxy Vitamin D3
1,25(OH)2D3 production acts to suppress parathyroid hormone. Thus, 1,25(OH)2D3 largely regulates serum phosphate concentration directly by increasing its intestinal absorption along with calcium absorption and also indirectly by increasing its tubular reabsorption through its suppression of parathyroid hormone.
These two regulators are tightly intertwined with FGF-23 physiology.
Fibroblast growth factor-23
The phosphatonins [FGF-23, FGF-7, sFRP-4, and MEPE ] are a group of proteins involved in the regulation of phosphate homeostasis. FGF 23 is best defined among them.
They cause a reduction in NaPiIIa protein expression, causing increased renal phosphate excretion.
FGF-23 is predominantly expressed in bone and receptors to FGF-23 are present in many tissues
The main effect of FGF-23 is on phosphate metabolism and the maintenance of phosphate homeostasis.
Increased oral phosphate intake results in increased secretion and higher serum levels of FGF-23. This causes increased loss of phosphorus in urine and decreased calcitriol production. With higher blood levels of FGF-23, there will also be decreased absorption of phosphate from the intestine.
The mechanism by which dietary phosphate affects FGF-23 levels is as yet unknown.
Intestinal phosphate absorption
All foods composed of animal or plant cells are rich in phosphate, with the major sources being protein-rich foods and cereal grains. An increase in dietary magnesium results in a decrease in phosphate absorption, whereas an adequate luminal concentration of sodium is essential to ensure phosphate absorption.
Dietary phosphate, 1?, 25-dihydroxyvitamin D (1,25(OH)2D3), and parathyroid hormone are the main effectors of phosphate absorption.
Epidermal growth factor, glucocorticoids, estrogens, metabolic acidosis and, as more recently shown, phosphatonins also affect the absorption.
Bone
Inorganic phosphorus is one of the two main ionic components required for hydroxyapatite formation. The enzymatic activity of alkaline phosphatase is required to generate enough of the free mineral.
In cases of hypophosphatemia [low serum phosphate levels], alkaline phosphatase activity rises in order to try to provide more phosphate to the bone cells. Once adequate amounts of phosphate are provided, the enzyme’s activity decreases
Renal phosphate reabsorption
The kidney is the major organ involved in the regulation of phosphate homeostasis by a variety of hormonal and non-hormonal factors including serum PTH, calcium, 1,25(OH)2D3 and bicarbonate concentrations.
Sodium reabsorption, hypercapnia or hypocapnia, dopamine, and serotonin also affect the phosphate excretion.
Almost nil reabsorption in the proximal straight tubule occurs in the presence of the parathyroid hormone. When the parathyroid hormone is not acting, phosphate is reabsorbed resulting in very low urinary excretion.
These changes are almost invariably paralleled by changes in the apical expression of NaPiIIa and NaPiIIc receptors in the proximal tubules.
Insulin, epidermal growth factor, thyroid hormone increase phosphate reabsorption.
Reduced or increased phosphate intake results in the increased or decreased expression of NaPiIIa receptors
Hypophosphatemia and Hyperphosphatemia
Kidneys are mainly responsible for decreased or increased levels of phosphates. Intestinal absorption or bone metabolism rarely cause changes in phosphate levels
Reabsorptive hyperphosphatemia occurs in diseases with decreased parathyroid secretion as in hypoparathyroidism. It also occurs in hereditary diseases in which the FGF-23 receptor/Klotho receptor complex is disrupted.
Reabsorptive hypophosphatemia occurs in diseases with increased parathyroid secretion, including primary and secondary hyperparathyroidism.
It also occurs in diseases with increased serum FGF-23, including oncogenic osteomalacia and various forms of hereditary osteomalacia.
GFR hyperphosphatemia occurs in chronic kidney disease because of the inability of the kidney to excrete the dietary phosphorus load. IT occurs in the face of increased serum concentrations of both PTH and FGF-23.