Last Updated on November 22, 2023
The posterolateral corner injury is commonly associated with anterior cruciate or posterior cruciate ligament injuries.
Isolated injuries to posterolateral corner are rare.
The injury usually occurs by a blow to the anteromedial knee, a varus blow to the flexed knee, hyperextension injuries and knee dislocation.
Peroneal nerve injuries are commonly associated.
Once referred to as dark side of the knee, posterolateral corner of the knee is well-understood part of knee anatomy and biomechanics.
A high level of suspicion is recommended based on the trauma setting and the patient symptoms. Failure to address this condition may place other reconstruction graft at risk and result in poor outcomes
Anatomy of Posterolateral Corner
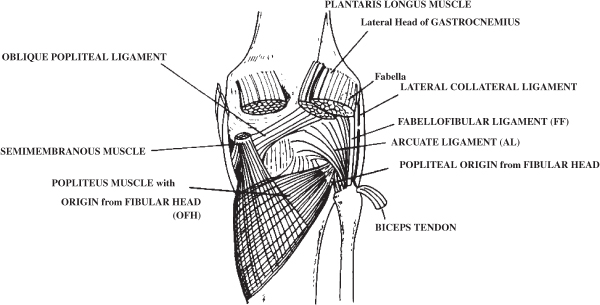
Posterolateral corner is constituted by the following structures
Static structures
- Lateral Collateral Ligament(most anterior structure inserting on the fibular head)
- Popliteus tendon
- Popliteofibular ligament
- Lateral capsule
- Arcuate ligament
- Fabellofibular ligament
Dynamic structures
- Biceps femoris (inserts on the posterior aspect of the fibula posterior to LCL)
- Popliteus muscle
- Iliotibial tract
- Lateral head of the gastrocnemius
These structures can be seen as primary and secondary stabilizers
Primary Stabilizers
Lateral Fibular Collateral Ligament
The fibular collateral ligament is the primary varus stabilizer of the knee. It attaches to the femur in a small bony depression slightly proximal and posterior to the lateral epicondyle. It courses distally to insert on the fibular and peroneus longus fascia.
Popliteus Tendon
The femoral insertion of the popliteus is about 20mm anteriorly from the FCL attachment with the knee at 70°. It courses posterodistally in an oblique fashion to insert into the posteromedial tibia. It becomes tendinous in the lateral third of the popliteal fossa
Popliteofibular Ligament
The popliteofibular ligament originates at the musculotendinous junction of the popliteus. It has anterior and posterior divisions that insert distally into the posteromedial aspect of the fibular head.
Secondary Stabilizers
These structures are:
- The lateral capsular thickening with its components consisting of the meniscofemoral and meniscotibial ligaments.
- The coronary ligament
- Attaches the posterior aspect of the lateral meniscus to the tibia.
- Lateral gastrocnemius tendon
- Attaches nearly 14 mm posterior to the femoral attachment of fibular collateral ligament.
- Courses distally in an intimate relationship with the posterolateral capsule to fuse with the medial gastrocnemius and the soleus.
- Serves as an important landmark during surgical reconstruction.
- The fabellofibular ligament
- Distal thickening of the capsular arm of the short head of the biceps femoris
- Extends vertically from the fabella to the fibular styloid.
- The fabella is a sesamoid bone found within the proximal lateral gastrocnemius tendon in 30% of individuals.
- The long head of the biceps femoris
- It divides approximately 1 cm proximal to the fibular head into direct and anterior arms.
- The direct arm inserts onto the posterolateral aspect of the fibular head
- The anterior arm has a small insertion site on the more distal and anterior aspect of the fibular head.
- Both arms enclose the fibular collateral ligament distal attachment
- The iliotibial band
- A broad layer that attaches onto Gerdy’s tubercle in the anterolateral aspect of the tibia.
- Numerous peripheral attachments to the patella, the lateral intermuscular septum, and the capsule exist
Layering of structures
Lateral Structures of Knee by Layer
Layer I
Iliotibial tract, biceps
common peroneal nerve lies between layer I and II
Layer 2
Patellar retinaculum, patellofemoral ligament
Layer 3
Superficial
LCL, fabellofibular ligament
The lateral geniculate artery runs between deep and superficial layer
Deep
Arcuate ligament, coronary ligament, popliteus tendon, popliteofibular ligament, capsule
Biomechanics of Posterolateral Corner
The posterolateral corner structures provide the primary restraint to varus forces of the knee as well as posterolateral rotation of the tibia relative to the femur.
When a knee is cruciate deficient, these structures are also important secondary stabilizers to anterior and posterior tibial translation.
The fibular collateral ligament is the primary restraint to varus stress across the knee, the rest of the posterolateral structures act as secondary varus stabilizers.
Fibular collateral ligament and the popliteus complex are the primary restraints for tibial external rotations, especially between 30° and 40° of flexion. Posterior cruciate ligament acts as a secondary restraint. popliteus works synergistically with the posterior collateral ligament to control varus, and posterior translation too.
Popliteus and popliteofibular ligament function maximally in knee flexion to resist external rotation
The popliteus tendon is a minor primary stabilizer (the anterior cruciate and anterolateral ligament being the main stabilizer)
Minimal contribution of the posterolateral corner has been reported for anteroposterior tibial translation specifically in full extension and with anterior or posterior cruciate deficient knees.
The lateral collateral ligament is a primary restraint to varus stress at 5° and 25° of knee flexion
Classification of Injury
Grade I (0-5mm of lateral opening and minimal ligament disruption)
Grade II (5-10mm of lateral opening and moderate ligament disruption)
Grade III (>10mm of lateral opening and severe ligament disruption and no endpoint)
Clinical Presentation of Posterolateral Corner Injury
There would be a history of a specific trauma that occurred to their knee. A direct blow to the anteromedial knee is the common mechanism of injury to the posterolateral corner.
Hyperextension and non-contact varus stress injuries can also injure posterolateral corner.
Most often, PLC tears are associated with ACL and/or PCL injuries.
Pain is the most frequently reported symptom. Instability in mediolateral direction is reported especially in extension and the patient finds it difficult to walk on uneven surfaces and stairs. There would be difficulty with pivoting and cutting.
Instability and difficulty walking can lead to as a varus thrust gait during the initiation of the stance phase.
A paraesthesia or numbness may indicate peroneal nerve injury.
On examination, the patient would walk with a varus thurst or hyperextension thrust. There would be varus laxity on giving varus stress.
Special Tests
All tests should be performed bilaterally to compare to the uninjured knee.
Varus Stress Test
It is performed both in full extension and at 20-30° of flexion.
For testing in full extension, the femur is stabilized to the examination table with one hand [the Same hand also assesses the amount of lateral compartment opening]. The other hand holds foot or ankle of the limb. Lateral compartment gapping is noted. The test is repeated with contralateral limb nd the gapping compared.
The test is repeated with the knee flexed to 30°.
An abnormal opening at 30 degrees of knee flexion indicates an injury to the FCL and potentially to the secondary stabilizers of the posterolateral corner of the knee. If stability is restored when tested in full extension, an isolated injury to the FCL is presumed. However, if the varus instability persists in full extension, a combined FCL, PLC and cruciate ligament injury are assumed.
Dial test
The dial test measures the external rotation of the tibia relative to the femur. It is done in the prone or supine position with the knee flexed to 30 degrees.
The femur is fixed with one hand while the ankle and foot are externally rotated. An increase of more than 10° of external rotation compared with the contralateral side suggests an injury to the posterolateral corner.
The knee is then flexed to 90°. Because of its role as an important secondary stabilizer, a knee with an intact PCL will see a decrease in external rotation. If, at 90°, there is an increase in external rotation, as compared with 30°, a combined PLC and PCL injury is presumed.
Reverse pivot shift test
The knee is positioned at 90° and external rotation and valgus force applied to the tibia. As the knee is extended the tibia reduces with a palpable clunk because tibia reduces from a posterior subluxed position at ~20° of flexion to a reduced position in full extension. This reduction is the result of the iliotibial band function changing from knee flexor to knee extender with extension and indicates injury to posterolateral corner with a positive predictive value of 68%.
External rotation recurvatum
The patient is in the supine position with legs extended. The great toe is grasped and the leg lifted from the table while securing the femur to the table by applying gentle pressure to the anterior distal femur. The height of the heel knee is then measured and compared with the contralateral side. A positive external rotation recurvatum test predicted a combined ACL and PLC injury though the test is not sensitive.
Posterolateral drawer test
This test is performed with the hip flexed 45 degrees, knee flexed 80 degrees, and foot is 15 degrees of external rotation.
A combined posterior drawer and external rotation force is then applied to the knee to assess for an increase in posterolateral translation i.e. lateral tibia externally rotates relative to the lateral femoral condyle.
Imaging
Radiographs
Standard anteroposterior, lateral and sunrise view radiographs of the knee should be obtained. In acute injuries, these x-rays are often normal.
For chronic posterolateral corner injuries, a standing long-leg AP alignment radiograph is a requirement because malalignment needs to be recognized and corrected with a biplanar osteotomy before the surgical reconstruction.
Stress Views
Varus stress radiographs at 20 degrees of knee flexion evaluate the severity of these lesions objectively. The radiograph is obtained for both limbs.
Lateral compartment gapping is determined by measuring the shortest distance between the subchondral bone surface of the most distal aspect of the lateral femoral condyle and the corresponding tibial plateau.
An isolated complete FCL tear has a side-to-side difference of 2.7 to 4.0 mm, while a difference of greater than 4 mm represents an associated grade III PLC injury.
MRI
MRI assists in the diagnosis of acute lesions assesses concurrent injuries and determines the location of the damaged structures.
Treatment of Posterolateral Corner Injury
Non-operative Treatment
This consists of immobilization of knee in full extension with protected weight bearing for about two weeks.
This treatment is indicated in grade I or II injuries of the posterolateral corner which are not associated with any other injury.
This immobilization is followed by progressive functional rehabilitation.
Grade III PLC injuries show poor outcomes with non-operative treatment.
Operative Treatment
This treatment is indicated in isolated posterolateral corner injuries grade II or injuries associated with other concomitant injuries.
Following surgical options are available
PLC repair
This is indicated in isolated PLC injuries with bony or soft tissue avulsion and in patients which could be operated within 2 weeks of injury.
A free graft may be used for augmentation.
PLC reconstruction
It is used in most grade III isolated injuries. It is also indicated when the repair is not possible or the tissue quality is poor.
The goal is to reconstruct lateral collateral ligament and the popliteofibular ligament using a free tendon graft from semitendinosus or Achilles.
Improved outcomes are associated with early treatment
PLC repair/reconstruction, ACL and/or PCL reconstruction with or without High Tibial Osteotomy
It is indicated in combined ligament injuries. High tibial osteotomy is indicated in patients with varus mechanical alignment. Achievement of bony alignment favors the outcome of ACL and PLC reconstruction success
The limb is immobilized and make protected weight bearing for 4 weeks, after which passive range of motion is begun.
Constructions have fewer revision rates than ligament repair.
References
- LaPrade RF, Resig S, Wentorf F, Lewis JL. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med. 1999;27(4):469–75.
- LaPrade RF, Muench C, Wentorf F, Lewis JL. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: a biomechanical study. Am J Sports Med. 2002;30(2):233–8.
- Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am. 1987;69(2):233–42.
- Ranawat A, Baker CL, 3rd, Henry S, Harner CD. Posterolateral corner injury of the knee: evaluation and management. J Am Acad Orthop Surg. 2008;16(9):506–18.
- Cooper DE. Tests for posterolateral instability of the knee in normal subjects. Results of examination under anesthesia. J Bone Joint Surg Am. 1991;73(1):30–6.
- Krukhaug Y, Molster A, Rodt A, Strand T. Lateral ligament injuries of the knee. Knee Surg Sports Traumatol Arthrosc. 1998;6(1):21–5.
- Clancy WG, Jr, Sutherland TB. Combined posterior cruciate ligament injuries. Clin Sports Med. 1994;13(3):629–47.
- McCarthy M, Camarda L, Wijdicks CA, Johansen S, Engebretsen L, Laprade RF. Anatomic posterolateral knee reconstructions require a popliteofibular ligament reconstruction through a tibial tunnel. Am J Sports Med. 2010;38(8):1674–81.
- Black BS, Stannard JP. Repair versus reconstruction in acute posterolateral instability of the knee. Sports Med Arthrosc. 2015;23(1):22–6.