Last Updated on August 24, 2019
Pronator syndrome is a compressive neuropathy of the median nerve at the level of the elbow.
The median nerve, one of the three major nerves of the upper limb mainly supplies the hand and is also known as the eye of the hand.
Pronator syndrome or pronator teres syndrome results in a predominantly sensory alteration in the median nerve distribution of the hand and the palmar cutaneous distribution of the thenar eminence.
It is one the compression neuropathies of the median nerve. Other two compression neuropathies of median nerve are anterior interosseous nerve and carpal tunnel syndrome which are described separately.
Pronator syndrome is more common in women, especially in the fifth decade. It has been associated with well-developed forearm muscles as in weightlifters.
Relevant Anatomy
The median nerve is formed in the axilla by the lateral and medial cords of the brachial plexus. It has contributions from has roots in C5, C6, C7, C8, and T1. In the axilla, it lies in the vicinity of the artery.
[Read more on brachial plexus]
In its course to elbow, the nerve lies close to the brachial artery, crossing it anteriorly to medially. It enters the cubical fossa lateral to the brachialis tendon.
After that, the median nerve passes between the two heads of the pronator teres. This is a possible site of compression. Further, it gives branches to the pronator teres, the flexor carpi radialis, the palmaris longus, and the flexor digitorum superficialis.
A significant branch is the anterior interosseous nerve, which is given off within the pronator teres and supplies the flexor pollicis longus, the pronator quadratus, and the lateral half of the flexor digitorum profundus.
The median nerve continues its course in the distal forearm, under the flexor digitorum superficialis, and on the flexor digitorum profundus. The palmar cutaneous branch just above the wrist and supplies the thenar eminence and central palm.
After branching, the median nerve continues into the hand via the carpal tunnel anterior and lateral to the tendons of the flexor digitorum superficialis. The carpal tunnel is formed by the carpal bones and the pronator quadratus on the inferior and side borders of the carpal tunnel. The flexor retinaculum forms the roof of the canal.
In the hand, the nerve divides into a muscular branch [supplies thenar eminence muscles] and a palmar digital branch
[supplies supply the palmar surface of the thumb, index, and middle finger and the lateral half of the ring finger, including the nail beds on the dorsal surface. – Read hand anatomy for more details]
The palmar nerves also give off branches to supply the two lateral lumbrical muscles.
Causes of Pronator Syndrome
Potential sites of entrapment are
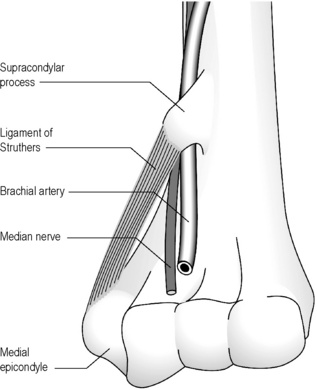
- Supracondylar process or spur [residual osseous structure on the distal humerus present in 1% of the population]
- Bony or cartilaginous
- On the anteromedial aspect of the humerus
- About 5 cm proximal to the medial epicondyle
- Often visible on x-rays
- Ligament of Struthers [travels from tip of the supracondylar process to medial epicondyle ]
- Bicipital aponeurosis or lacertus fibrosus
- Between ulnar and humeral heads of pronator teres
- Aponeurotic arch of flexor digitorum superficialis
Clinical Presentation
Aching discomfort in the forearm is the common presentation especially pain over the median nerve distribution distal to the elbow.
Weakness in the hand and paresthesia in the thumb, index, middle finger and radial half of ring finger are seen especially after repeated pronation and supination.
[Aches and sensory disturbances over the distribution of palmar cutaneous branch of the median nerve (palm of the hand) [ arises 4 to 5 cm proximal to carpal tunnel] and lack of night symptoms differentiate from carpal tunnel syndrome.]
Provocative tests
Development of paresthesia in the hand after 30 seconds or less of manual compression of the median nerve suggests pronator syndrome and may also indicate the possible site of entrapment in pronator syndrome
Provocative tests include
- Reproduction of symptoms upon flexion of the elbow against resistance between 120° and 135°
- Suggests ligament of Struthers compression of the median nerve
- Resisted elbow flexion and supination while forearm is in the pronated position
- Suggests compression at bicipital aponeurosis
- Resisted forearm pronation with the elbow extended and wrist flexed [flexed to relax flexor digitorum superficials]
- Suggests compression at two heads of pronator teres
- Resisted contraction of fibrous digitorum superficialis to the middle finger
- Compression at the flexor digitorum superficialis fibrous arch
Compression by pronator is also suggested by direct pressure on the leading edge of the pronator while the forearm is in maximum supination and the wrist in a neutral position.
Motor and sensory examination of the limb should be done as well.
Imaging
X-rays
X-rays of the elbow are done to view any bony abnormality. The supracondylar process may be visualized
EMG and NCV
Usually inconclusive
Ultrasonography and MRI
These may be useful in the evaluation. Atrophy can be appreciated in the involved muscles.
Treatment of Pronator Syndrome
Nonoperative Treatment
For mild to moderate symptom
- Rest
- Splinting to avoid forearm rotation
- NSAIDS
The treatment is carried out for 3-6 months. A splint is applied to avoid forearm rotation.
Operative Treatment
It is considered when nonoperative management fails for 3-6 months. Patients who do not respond to conservative treatment and/or experience motor deficits require decompression surgery.
Surgical treatment is done by decompression of the median nerve at possible sites of compression
Compression points are determined by physical examination in preoperative assessment.
The incision begins a few centimeters above the elbow crease at the antecubital fossa and continues distally in an S or zigzag fashion.
The bicipital aponeurosis should always be divided. The median nerve is then exposed by dividing the superficial fibers of the pronator teres where the areas of compression are addressed individually.
A soft dressing is used postoperatively. Elbow is Splinting, however, is done by keeping the elbow slightly flexed and the wrist in a neutral position.
The sutures are removed 12-14 days after carpal tunnel release. Patients are allowed activity without restrictions after 6-8 weeks
Outcomes of surgical decompression are variable. About 80% of patients have relief of symptoms.