Last Updated on November 20, 2019
Pyogenic infection of the spine is rare, constituting only about 2-8% of overall pyogenic infection. The spectrum of pyogenic infections includes spondylitis, discitis, spondylodiscitis, pyogenic facet arthropathy, epidural infections, meningitis, and myelitis.
The incidence of spinal infections has increased recently due to globalization, improved life expectancy, comorbidities like diabetes, overuse of antibiotics, immunosuppression and other immunocompromised conditions and spinal surgery.
The rise in intravenous drug use is also responsible for increased incidence.
It is difficult to differentiate the pyogenic infection of the spine from degenerative processes, inflammatory disorders, metabolic disorders, and tumors.
The reported incidence is 0.2-2 cases per 100000 per year.
Men are affected twice as compared to women and peak incidence is in the sixth decade.
However, it is being reported more commonly in 20-40 years old people. This is secondary to intravenous drug abuse and HIV infection. This group also has more cases of the atypical location of infection and presentation.
Vertebral osteomyelitis, discitis, and epidural abscess are the types of pyogenic infections of the spine. SPondylodiscitis is the name given when vertebra and disc are affected together.
Risk Factors or Predisposing Factors for Pyogenic Infection of Spine
- Immunocompromised person
- Diabetes
- HIV positive
- Malignancy
- Chronic use of steroid
- Renal failure
- Recent spinal surgery
- Presence of intravascular devices
- Presence of focus of organisms or wound contamination
- Radiation therapy
- Smoking
- Rheumatoid arthritis
- Intravenous drug abuse
- Poor nutritional status
Pathology of Pyogenic Infections of Spine
To understand pathology, an idea about anatomy of spine is needed. Following anatomy articles would guide you through the anatomy of the spine and its constituents.
- Anatomy of spine
- Vertebral canal Anatomy
- Cervical Spine Anatomy
- Thoracic Spine Anatomy
- Lumbar Spine Anatomy
- Anatomy of Intervertebral Disc
About 95% of pyogenic spinal infections involve the vertebral body and only 5% involve the posterior elements of the spine. The difference is due to the volume of supply that anterior vertebra receives
Hematogenous spread, direct inoculation and spread from adjacent sites [contoguous spread] are main routes infections of the spine.
Infection of the spinal column may typically manifest as discitis, vertebral osteomyelitis or epidural abscess.] though the spectrum includes meningitis, subdural empyema, and spinal cord abscess too.
The organism causing Pathogenic organisms reach the spine hematogenously through arteries or veins (via Batson’s plexus), or by direct inoculation from a diagnostic or a surgical procedure.
[Note: Batson venous plexus is a network of veins with no valves that connect deep pelvic veins to the internal vertebral venous plexus. These form an important route for infections and tumors to spread]
Discitis or isolated infection of the intervertebral disc occurs initially in the children and involvement of end plates is subsequent. It occurs more commonly in children because of the presence of extensive anastomosis between the metaphyseal arteries and arteries of vertebral endplates.
In adults, a small septic embolus may lodge in the subchondral spongy bone is supplied by nutrients end arteries leading to bone infarction and eventually vertebral osteomyelitis. [spondylitis]
Contiguous spread to the disc can cause discitis in addition to osteomyelitis. [Spondylodiscitis]
Spread to the adjacent vertebra occurs through anastomotic vessels between the metaphysis.
The postoperative or iatrogenic infection is caused by direct inoculation.
The lumbar spine is the most common location, followed by the thoracic and cervical spine.
Posterior surgeries at higher risk than anterior. Those surgeries where instrumentation is carried have a higher risk.
Epidural abscess the pus collection as a collection of pus and is seen in about 18% of patients with spondylodiscitis. An epidural abscess can be seen in facet joint infections and posterior infections too.
The neural deficit is seen in about 20% of the patients of pyogenic infection of the spine and in almost 50% of epidural abscess cases. The deficit results from direct infection of neural elements, compression by an abscess or due to instability.
Very rarely intradural abscess is seen.
Facet joint infection is also rare but has increased recently probably as a result of the increased elderly population, immunocompromised patients, and spine procedures.
Facet joint can result in epidural/paraspinal abscesses too.
The infection of a facet joint is often hematogenous but epidural anesthesia and spinal procedures can also cause it.
It has more acute presentation than the spondylodiscitis.
L4–L5 facet joints are most commonly involved.
Degenerated facet joints may pose an increased risk for infection.
Organisms
Gram-positive aerobic cocci are the most common organisms causing pyogenic infections of the spine. Staphylococcus aureus is the predominant organism (55%).
In infants and children, S. aureus is the commonest organism like adults but Streptococcus pyogenes is seen more frequently than in adults.
Gram-negative bacteria could be the common organism in cases where the lesion is secondary to urinary tract infection or instrumentation. Common gram negative bacteriae include E. coli and rarely Proteus, Klebsiella, Enterobacter, and Serratia.
Anaerobic infections are responsible for 3% of axial skeleton infections. They are more common in diabetic patients.
Main anaerobic bacgteria are Bacteroides spp., Peptococcusspp., and Propionibacterium acnes.
Pseudomonas is frequently seen in Intravenous drug users.
Postoperative wound infection is most commonly due to S. aureus. But multiple organisms are frequently seen in this group.
Polymicrobial infections are much more common in sacral osteomyelitis.
Clinical Presentation
Presentation in Adults
A history of infection somewhere [UTI, pneumonia, skin infection] or of an organ transplant may be present. common
Gradual onset back pain is the commonest presentation. Pain is worse at night and activity may aggravate pain.
Pain may mimic mechanical back pain but paravertebral muscle spasm and stiffness may be out of proportion to pain.
A pain that wakes the patient up in the night should be investigated for infection or malignancy.
Fever is not a consistent feature. Only one-third of patients have it.
Pain may radiate to the abdomen, hip, leg, scrotum, groin or perineum.
On examination, there would be tenderness and spasm in paravertebral muscle spasm. The movements of the spine would be limited.
Atypical presentations may occur
- Acute abdomen or chest pain
- Osteomyelitis may present as non-traumatic compression fracture.
- A patient with a fracture with fever and raised ESR is considered to have an infection
- Intra-venous drug abusers and diabetics have an acute presentation
- Progression of spinal pain to radicular signs followed by weakness/paralysis suggest
- Formation of an epidural abscess
- The collapse of the infected vertebra
Presentation in Children
The presentation of discitis in children depends on age.
Younger than 3 years
- Irritability
- Refusal to walk or even sit
- Prefer lying
Between 3-10 years
- Abdominal pain
- Tight hamstrings
- Back tenderness
- Rigidity
>10 years
These children usually present with predominant back pain. Marked fever is less likely. History of trauma may be present but usually unrelated to the cause of infection.
In infants, vertebral osteomyelitis presents with pain, fever, gibbus, raised leucocyte count, and complete dissolution of the vertebral body. These patients require a very aggressive treatment.
Post-operative infection
Postoperative wound infection is most often diagnosed between 10 days and 2 weeks. Fever beyond the first few days, and continued wound discharge beyond 10 days and discharges which initially wanes and then increases often indicate infection.
Fever may not be present in nearly half the patients. Treatment must be initiated aggressively and early on the basis of clinical diagnosis.
Differential Diagnoses
Degenerative spine
- Primary tumors or Metastases
- Disc herniation
- Vertebral compression fracture
- Inflammatory spondyloarthropathies
- Visceral Infection/inflammation
- Pyelonephritis
- Appendicitis
- Abdominal abscess
Lab Studies
The white blood cell count is often normal. It may be elevated in 35-50% of patients but rarely exceeds 12,000 cells/mm3.
An elevation of the erythrocyte sedimentation rate (ESR), is usually seen in almost all cases.
CRP, like ESR, is also elevated in most of the patients. Serial measurements of both can be used to monitor disease progression. CRP is said to be more reliable than ESR.
Blood, urine and any other infective focus should be cultured.
About 50% of the patients have blood cultures positive.
Cultures help to isolate the organism and are helpful in guiding the choice of antimicrobial therapy.
If the cultures listed above are negative, tissue should be obtained from the lesion by CT guided percutaneous needle biopsy can be performed.
In difficult cases, open biopsies may be considered.
Whenever possible, antibiotics should be held until cultures have been obtained.
Biposy, tisssue cultures for fungi and mycobacteria may also be done where there is a higher suspicion for such infections [A subacute presentation, negative gram stain, and bacterial culture.]
Imaging
X-rays
The nonspecific changes of infection may take as long as 2 to 12 weeks to appear in plain radiographs. The earliest changes usually observed are an erosion of the endplate and loss of disc height, and these usually occur within 3 to 6 weeks.
More destructive changes occur during the next 6 to 12 weeks, which includes osteolytic compression of the vertebral body, paravertebral soft tissue shadows.
With the progress of infection, the erosion of the end-plate and adjacent bone becomes more prominent. This leads to the narrowing of the disc space and segmental collapse.
Reactive sclerosis may be observed after 2 months, followed later by bone bridges across the disc, and then, typically, autofusion. Fusion may take as long as 5 years.
Others develop a fibrous union.
Children with discitis present early radiological findings. Narrowing of disc space may be observed within 2 weeks of first symptoms. Endplate erosion occurs later, progressing to reactive sclerosis without vertebral body destruction. Restoration of disc height may occur within 3-12 months with successful early treatment.
Radionuclide Bone Imaging
Radionuclide bone scanning is able to identify infection in the early days.
Sequential bone/gallium imaging and 67Ga-SPECT are currently the radionuclide procedures of choice.
The specificity of bone scintigraphy is in the range of 75–80%.
CT
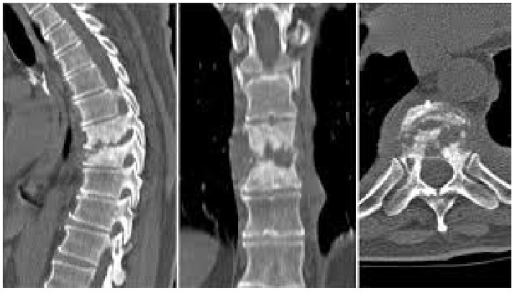
CT offers a superior definition of extra-spinal soft-tissue abscess and epidural abscess. It is also useful in distinguishing between pyogenic and tubercular infections and tumors.
The pyogenic infection causes diffuse bony destruction and soft tissue involvement whereas tuberculosis exhibits patchy lytic lesions with sclerosed margins at times, and a large well defined paravertebral mass or abscess.
CT scan with metrizamide myelography may be useful to define epidural abscess. The commonest use of the CT lies in CT guided biopsy and aspiration of the paravertebral abscess.
CT scan is particularly useful tool for surgical planning too.
MRI
This is the most helpful diagnostic imaging test for pyogenic infection in the spine. MRI is more sensitive than the bone scan and became the gold standard in the evaluation of pyogenic infections of the spine.
It has a sensitivity of 96%, a specificity of 92%.
MRI is especially helpful in detecting the epidural abscesses that often have signal characteristics similar to CSF and may be missed in unenhanced MRI, but show rim enhancement with gadolinium. T
MRI can also be used for monitoring of the treatment response.
Treatment
If recognized early, the treatment is simple and effective but is often recognized late due to the non-specific picture of the disease.
The goals of treatment are relief from pain, regaining neural functions if affected, eradicate infection, prevent relapse, and establish spinal stability.
Conservative treatment
The conservative treatment consists of following
- Identification of organism
- Appropriate antibiotics
- Spinal immobilization
- Monitor for progression of disease and evidence of spinal instability
After samples are sent to the lab for microbiological diagnosis, the patient is put on bed rest or spine is immobilized, depending on the site of disease. Tissue diagnosis may be required in certain cases.
Cervical spine is placed in a halo halo immobilization or cervical collar.
For rest of the spine, bed rest is prescribed until the pain diminishes and then a brace [TLSO] is provided for becoming upright.
Spinal immobilization and activity restriction should be continued for 10–12 weeks or until radiographic evidence of healing is present.
Either the antibiotics are held until the organism is identified or started on empiric broad antibiotic therapy based on the clinical assessment.
Once an organism has been identified, antibiotics should be administered intravenously for 4-6 weeks. It is followed by oral antibiotics for the next 6-8 weeks. The total duration of antibiotic therapy is 12 weeks.
Choice of antibiotics is guided by the sensitivity report. A rough guide of various antibiotics used is given below.
Gram positive bacteria i.e. Staph Aureus
Pencillinase producing
- Semisynthetic Peniciliin
- Oxacillin
- Nafcillin
- First generation cephalosporins
- Cephalothin
- Cefalexin
- Cefazolin
- Second generation cephalosporin
- Cefuroxime
Methicillin resistant
- Vancomycin
- Teicoplanin
- Tigercyline
- Daptomycin
Gram Negative Bacteria
Pseudomonas aeruginosa
- Ticaricillin
- Piperacillin
- Mezocillin
- Ceftazidime
- Cefepime
- Carbapenem
- Aztreonam
- Ciprofloaxillin
Aminoglycosides [Gentamycin, Tobramycin, Amikacin] may or may not be added.
Other than Pseudomonas
- 2nd or third generation cephalosporins [as per sensitivity results]
- Resistant bacteria are treated as same as Pseudomonas
CRP level can be used to monitor the course of the disease.
Operative Treatment
Over one-third of patients fail to respond to conservative therapy.
Indications for surgery are
- Significant neurological impairment
- Presence of large abscess
- Severe intractable pain
- Progressive deformity
- Gross instability
Surgical treatment should
- Removal of infected tissue
- Decompression of neural elements
- Restoration of alignment
- Correction of instability
In most of the cases, anterior vertebral elements are involved in infection and intact posterior elements provide some stability, thus preventing significant subluxation.
Therefore posterior decompression like laminectomy without stabilization may my alone may further destabilize the spine.
Most of the authors advocate anterior surgeries or a posterolateral approach that preserves the laminae, facets, and pedicles.
Some recent studies have recommended additional posterior spinal fixation after anterior decompression and fusion depending on the quality of bone, the number of segments involved, and the presence of pre-existing kyphotic deformity
Bone graft is used where spinal fusion is contemplated.
Anterior decompression with or without autologous bone graft and instrumentation:
The most satisfactory method to achieve a thorough debridement of the destructive lesion is by an anterior approach. It is often necessary to use autograft or allografts to restore stability.
Instrumentation may be done to decrease the need for prolonged immobilization. Depending on the condition of the lesion and patient, it could be done as a single stage procedure or in two stages.
Posterior decompression without fusion
As mentioned before, isolated posterior decompression further destabilizes the spine producing progressive deformity and worsening the neurological deficit. In rare instances, when infection principally involves posterior elements, or the epidural abscess is posterior or lateral to the dural sac, a laminectomy may be indicated.
Posterior decompression with fusion and instrumentation
Extensive surgery than just a abscess drainage is required when the disease includes anterior elements too. To approach the disease posteriorly various approaches like posterolateral approaches, transpedicular decompression or costotransversectomy approaches are often required to achieve decompression.
Following debridement, it is usually necessary to restore stability with interbody bone grafts, using autograft rib or fibular allograft. Posterior instrumentation is often required for adequate stabilization.
When instrumentation is required, it could be done in the second stage after the posterior wound is healed following the initial debridement.
Alternately one stage procedure can be done.
Complications
- Pharyngeal abscess in cervical spine lesions
- Mediastinitis in thoracic spine lesions
- Epidural abscess
- Subdural abscess
- Meningitis
- Segmental collapse with spinal instability
- Progressive neurological defici