Last Updated on November 19, 2019
Secondary hyperparathyroidism is the overproduction of parathyroid hormone secondary to a chronic abnormal stimulus for its production. In contrast to primary hyperparathyroidism, the parathyroid glands are not abnormal. In contrast, the primary hyperparathyroidism is due to unregulated secretion of parathyroid hormone and is not in response to any stimuli.
But secondary hyperparathyroidism is due to alteration in calcium metabolism for one reason or other.
Chronic renal failure and vitamin D deficiency are two common causes of secondary hyperparathyroidism.
In chronic renal failure disease, overproduction of parathyroid hormone occurs in response to increased phosphate levels [hyperphopshatemia] or decreased calcium [hypocalcemia]. This occurs due to decreased 1,25-dihydroxyvitamin D production by the diseased kidneys.
Hyperphosphatemia can directly stimulate parathyroid hormone synthesis and parathyroid hyperplasia. It further contributes to secondary hyperparathyroidism by decreasing free calcium level.
Causes of Secondary Hyperparathyroidism
Secondary hyperparathyroidism is the result of another condition that lowers calcium levels. Therefore, your parathyroid glands overwork to compensate for the loss of calcium. The common thread for all of these conditions is that the intestines do not absorb enough calcium. Factors that may contribute to secondary hyperparathyroidism include:
- Kidney failure requiring dialysis
- Malabsorption leading to deficiencies of vitamin D and/or calcium
- Stomach or intestine bypass for obesity surgery
- Gastric Stapling
- Roux-n-Y Bypass
- Gastric (stomach) Bypass
- Celiac Disease (rare)
- Crohn’s Disease (rare)
- Long-term lithium therapy,
- Vitamin D-resistant rickets
- Hypermagnesemia (abnormally high blood magnesium levels).
Pathophysiology of Secondary Hyperparathyroidism
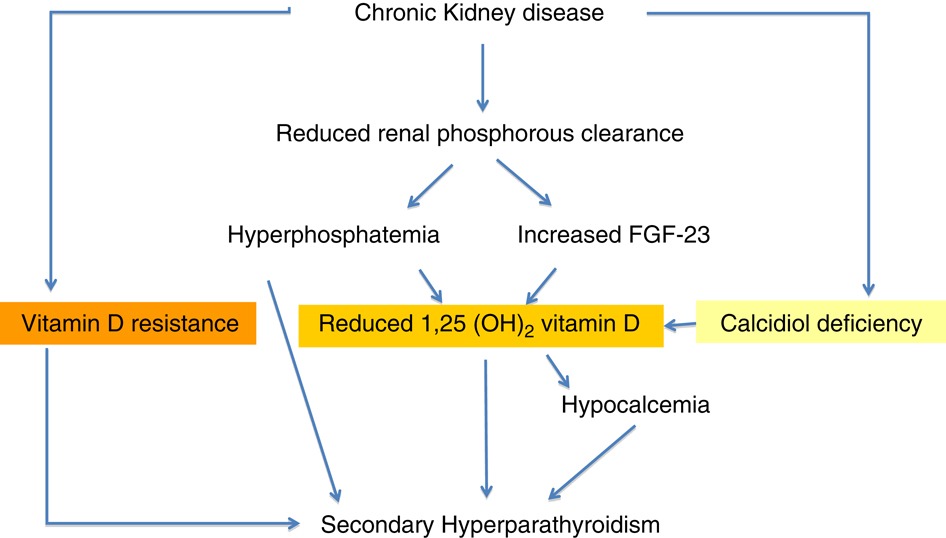
Chronic kidney failure is the most common cause of secondary hyperparathyroidism. Hyperparathyroidism due to kidney disease occurs due to a decrease in the production of vitamin D3 and nonfunctioning glomeruli. In the normal state, kidneys can eliminate phosphorus easily. Failing kidneys do not convert enough vitamin D to its active form, and they fail to excrete phosphate effectively. This leads to a decrease in calcium and an increase in phosphate levels of blood.
The hyperphosphatemia urges the parathyroids to greater activity in an effort to excrete the mineral, resulting in excessive excretion of parathyroid hormone creating a hyperparathyroid state is created. Enlargement of parathyroid gland may be noted.
Excess of parathyroid hormone causes bone resorption leading to with consequent rise of calcium and phosphorus in the bloodstream. Since these elements cannot be eliminated by the kidneys, they are deposited throughout the soft tissues as calcium phosphate forms in the body leading to renal stones and metastatic pathologic calcification in tissues.
High levels of parathyroid hormone can lead to
- Weakening of the bones
- Calciphylaxis (when calcium forms clumps in the skin and leads to ulcers and potentially death of surrounding tissue
- cardiovascular complications
- abnormal fat and sugar metabolism
- Itching
- low blood counts (anemia).
The eventual result is renal rickets in the child and renal osteomalacia in the adult.
In malabsorption diseases, there is a deficiency of calcium in the blood due to poor absorption in the diet. Lack of vitamin D and/or calcium leads to the stimulation of parathyroid hormone.
Clinical Presentation
For skeletal changes of hyperparathyroidism, read primary hyperparathyroidism.
In renal causes, chronic overproduction of parathyroid hormone in patients and the renal disease itself contributes to the spectrum of bone disease like osteitis fibrosa cystica and mixed uremic osteodystrophy.
Features suggestive of osteomalacia in adults and rickets in children occur. These include softening of bones in adults and joint deformities like valgus and varus in children. Some patients may have bone pain.
Cardiovascular calcification leads to cardiovascular complications. Soft tissue calcification, endocrine disturbances, compromised immune system, neurobehavioral changes are noted. Bone marrow cell production may be altered.
Calciphylaxis is painful skin lesions that begin as small nodules or plaques with a purplish color, grow and become necrotic. These are resistance to routine wound care. These occur due to deposition of calcium salts in the skin and tissues.
Primary versus Secondary Hyperparathyroidism
There can be confusion in a diagnosis of primary and secondary hyperparathyroidism because the presentation could be overlapping.
One simple differentiating feature is a level of high calcium in the blood. Secondary hyperparathyroidism is not associated with high blood calcium.
High parathyroid hormone levels with high blood calcium levels are diagnostic of primary hyperparathyroidism.
It is important to understand the difference as the causation and treatment are different altogether.
Primary hyperparathyroidism is caused by a tumor of a parathyroid gland which leads to an unregulated rise in blood parathyroid hormone and as a result high levels of calcium. This is treated surgically.
Causes of secondary hyperparathyroidism are many but the ultimate common thread is a deficiency of vitamin D leading to low calcium and high parathyroid levels.
So it is the calcium level that differentiates between the two types. If high calcium, high parathyroid levels – it is primary but if the calcium is low to normal and parathyroid is high – it is secondary hyperparathyroidism.
Another feature is that most of secondary hyperparathyroidism cases are present in patients with renal failure requiring dialysis.
If the patient does not have dialysis but has high parathyroid and renal problems, it could be primary hyperparathyroidism with renal disease.
Diagnostic Studies
Lab Studies
- Serum parathyroid hormone
- Serum calcium and phosphorus levels
- Serum vitamin D3 levels
The phosphate level is high in renal insufficiency and low in vitamin D deficiency.
Imaging
Xrays
Xrays have limited role in secondary hyperparathyroidism only to examine the painful bone sites.
Bony changes similar to primary hyperthyroidism can be noted subperiosteal erosions.
Imaging of parathyroid glands is not needed. Imaging of the parathyroid glands is not indicated unless primary hyperparathyroidism is suggested.
Treatment of Secondary Hyperparathyroidism
Secondary hyperparathyroidism is mainly treated by medical therapy. The idea is to supplement vitamin D and calcium deficiency.
50,000-IU of oral vitamin D are given for 8 weeks and the second course can be followed if needed, for the same duration.
In renal patients following measures are helpful
- Dietary phosphate restriction if the parathyroid hormone is high in spite of vitamin D supplementation
- Phosphate binders if dietary restriction also does not help to lower phosphate
- Calcium carbonate
- Calcium acetate
- Sevelamer hydrochloride
- Lanthanum carbonate.
- Calcium supplementation
- Calcimimetics- cinacalcet
Surgery in Secondary Hyperparathyroidism
Indications for surgery include bone pain or fracture, pruritus, calciphylaxis (see Related Disorders), and extraskeletal nonvascular calcifications with elevated parathyroid hormone levels despite appropriate medical therapy.
Parathyroidectomy can be considered in patients with severe hyperparathyroidism (persistent serum levels of intact parathyroid hormone greater than 800 pg/mL [88.0pmol/L]), associated with hypercalcemia and/or hyperphosphatemia that is refractory to medical therapy.
The procedure of choice is either total parathyroidectomy with autotransplantation or 3.5-gland parathyroidectomy. In either case, a thymectomy must be included
Briefly, parathyroid tissue is cut into approximately 16-20 pieces, each of which measures 1 X 1 mm. These are inserted in pockets in the forearm musculature, and each piece is marked with a polypropylene suture on the fascia. Parathyroid tissue must also be cryopreserved [preserved by freezing] in case the primary autotransplant fails.
If total parathyroidectomy and autotransplantation are performed, the patient requires a period of maintenance with calcium and calcitriol supplementation.
Most people with hyperparathyroidism secondary to chronic kidney disease will improve after renal transplantation, but many will continue to have a degree of residual hyperparathyroidism (tertiary hyperparathyroidism) post-transplant with the associated risk of bone loss, etc.
Prognosis
Medical therapy is effective in most patients. Some patients may require parathyroidectomy. Patients who require removal of parathyroids have approximately a 10% risk of recurrent or persistent disease owing to missed gland or hyperplasia of the autograft.
Some patients have persistent hypoparathyroidism after the operation. Cryopreserved tissue may be used for transplantation in such cases and that may reverse hypoparathyroidism.
If hypoparathyroidism is permanent, lifelong calcium and calcitriol supplementation are necessary.
Untreated secondary hyperparathyroidism may progress to tertiary hyperparathyroidism. In such cases, correction of the cause does not stop excess parathyroid secretion due to irreversible parathyroid gland hypertrophy. Tertiary hyperparathyroidism is associated with hypercalcemia rather than hypocalcemia.