Last Updated on July 31, 2019
Seronegative spondyloarthropathy is a group of diseases affecting axial skeleton and share common features.
Actually, the term spondyloarthropathy or spondyloarthrosis means diseases of joints of the vertebral column in contrast to the term spondylopathy which means disease of the vertebra itself.
However, the use of the term includes diseases of vertebral joints and vertebra both.
Ideally, the term should refer to any type of joint disease, including rheumatoid arthritis and osteoarthritis.
But the use of the term has become limited to a group of disorders with certain common features and termed specifically as seronegative spondyloarthropathies.
Thus spondyloarthropathy and seronegative spondyloarthropathy is used interchangeably.
What are Seronegative Spondyloarthropathies and Why These are Called So?
Spondyloarthropathies are a group of disorders is characterized by
- Arthritis [of peripheral joints or spine, usually involving also the sacroiliac joints.]
- A negative test for rheumatoid factor [that is why they are called seronegative spondyloarthropathy.]
- Association with medical problems like psoriasis, inflammatory bowel diseases [Ulcerative colitis or Crohns disease], uveitis, urogenital or gastrointenstinal infections.
- Enthesitis (inflammation at the site of insertion of tendons and ligaments to bone)
There is a strong correlation with HLA-B27 .
They have an increased incidence of HLA-B27, as well as negative rheumatoid factor and ANA.
These are called Seronegative spondyloarthropathies because they are negative for rheumatoid factor.
Spondyloarthropathy with inflammation is called axial spondyloarthritis.
Prevalence of spondyloarthropathies is reported to be around 2% with slight male preponderance. Those individuals who are positive for HLA B27 have 20 times more risk of developing spondyloarthropathy.
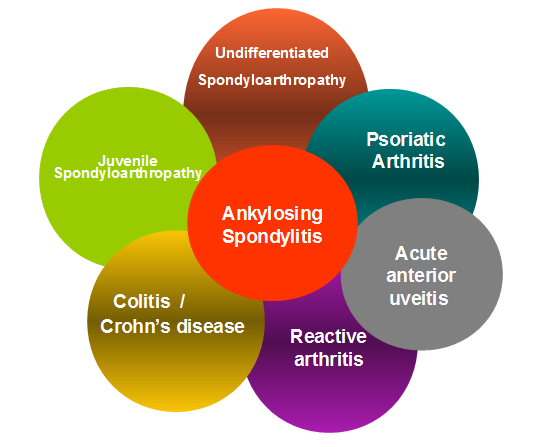
The diseases included in this group are
- Ankylosing spondylitis
- Reiter’s syndrome or reactive arthritis
- Enteropathic arthritis or arthritis associated with Irritable Bowel Disease
- Psoriatic arthritis
- Behçet’s disease
- Juvenile idiopathic arthritis
- Undifferentiated spondyloarthropathy
Ankylosing spondylitis and undifferentiated spondyloarthropathy are the most frequent subtypes of seronegative spondyloarthropathy.
Criteria for Spondylarthropathy
[The European Spondylarthropathy Study Group (ESSG)]
Presence of Inflammatory back pain, or synovitis (asymmetric, predominantly in the lower limbs) along with one or more of the following:
- Past or present psoriasis
- Past or present ulcerative colitis or Crohn’s disease
- Past or present pain alternating between the two buttocks
- Past or present enthesitis [spontaneous pain or tenderness on examination of the site of insertion of the Achilles tendon or plantar fascia]
- An episode of diarrhoea occurring within one month before onset of arthritis
- Nongonococcal urethritis or cervicitis occurring within one month before onset of arthritis
- Family history: first-degree or second-degree relative with ankylosing spondylitis, psoriasis, acute iritis, reactive arthritis or inflammatory bowel disease
- Bilateral grade 2-4 sacroiliitis or unilateral grade 3 or 4 sacroilitis.[see below for meanings of grades]
Apart from ESSG, Amor criteria is also used for diagnosis of spondyloarthropathies.
| ESSG Criteria | Amor Criteria* | |
| Inflammatory spinal pain or synovitis and one of the following: | Inflammatory back pain | 1 point |
| Alternating buttock pain | Unilateral buttock pain | 1 point |
| Enthesitis | Alternating buttock pain | 2 points |
| Sacroiliitis | Enthesitis | 2 points |
| Inflammatory bowel disease (IBD) | Peripheral arthritis | 2 points |
| Positive family history of spondyloarthropathy | Dactylitis (sausage digit) | 2 points |
| Acute anterior uveitis | 2 points | |
| HLA-B27 –positive or family history of spondyloarthropathy | 2 points | |
| Good response to NSAIDs | 2 points | |
| *Diagnosis of spondyloarthropathy with 6 or more points | ||
On plain radiographs, sacroilitis grading according to the New York criteria.
- Grade 0 – Normal
- Grade I – Some blurring of the joint margins – suspicious
- Grade II – Minimal sclerosis with some erosion
- Grade III
- Definite sclerosis on both sides of joint
- Severe erosions with the widening of joint space with or without ankylosis
- Grade IV – Complete ankylosis
Brief About Different Seronegative Spondyloarthropathies
Ankylosing Spondylitis
Ankylosing spondylitis is the most common of seronegative and primarily affects axial skeleton, usually begins in adolescence and early adulthood. The disease also affects peripheral joints as well, hip and shoulder being most common.
The prevalence of ankylosing spondylitis is 0.1-0.2% and may be higher in certain populations.
The male-to-female ratio of ankylosing spondylitis is 3:1.
The disease begins in the sacroiliac joints. Most patients have mild chronic disease or intermittent flares with periods of remission. Progression occurs from the lumbosacral region to involve other regions of the spine.
Peripheral involvement is seen in 30-50% of the patients.
Uveitis is the most common extra-articular manifestation [20-30% ]. Cardiovascular involvement <10% of patients, typically those with severe long-standing disease.
The course of the disease is characterized by remissions and exacerbations and Clinical presentation of ankylosing spondylitis varies from individual to individual.
Morning stiffness is characteristic. Peripheral Pains are due to enthesitis.
Pain is reported mainly in the hips, shoulders, and joints of the chest wall, including the acromioclavicular and sternoclavicular joints. Other peripheral joints are involved less frequently and to a milder degree.
More on Ankylosing Spondylitis
Reactive Arthritis
Earlier known as Reiter syndrome, reactive arthritis is an autoimmune disease that develops in response to genitourinary or gastrointestinal infection or a preceding Chlamydia respiratory infection.
Mechanism of development of reactive arthritis is not known but antigens are known to cross-react with self-proteins.
The frequency is estimated to be 3.5-5 cases per 100,000.
Reactive arthritis is most common in young men, with the peak onset in the third decade of life. It is rarely seen in children.
Reactive arthritis after gastroenteric infections is equal in both males and females. The disease associated with genitourinary infection is found more in males.
Enteropathic arthritis or Arthritis associated with Inflammatory Bowel Disease
It is a form of chronic, inflammatory arthritis associated with inflammatory bowel disease like ulcerative colitis and Crohn’s disease.
Peripheral limbs are more commonly involved than the spine.
The disease is characterized by abdominal pain [often bloody diarrhea] and joint pains.
Psoriatic arthritis
Psoriatic arthritis is a chronic inflammatory, seronegative arthritis that develops in patients of psoriasis. About 5% of people with psoriasis have psoriatic arthritis.
The most common type of psoriatic arthritis involves few joints.
Distal joint involvement and arthritis mutilans are characteristic features of psoriatic arthritis but less common.
The peripheral joint disease occurs in 95% of patients with psoriatic arthritis, and the spine is involved in 5%.
Psoriatic arthritis is more frequent in patients with severe psoriasis. However, the severity does not relate to the pattern of joint involvement.
[More on psoriatic arthritis]
Behcet’s disease
Behçet disease is a rare vasculitis in small, medium and large vessels resulting in multisystem affections involving gastrointestinal, eyes, skin, joints, and brain.
The disease appears to involve an autoimmune response triggered by exposure to an infectious agent.
It can lead to multiple signs and symptoms which at first appear unrelated.
Examples are mouth ulcers, inflammation of the eye, skin rashes and joint pains.
The systemic manifestations can be variable and symptoms vary from person to person. It may disappear and recur on its own.
Painful mouth sores aphthous ulcers is the most common presentation.
The sores usually heal in one to three weeks and may recur.
Sores on genital glands, scrotum, and vulva show genital involvement. The skin may have acne like ulcers or raised and tender nodules.
Uveitis in the eye can lead to a painful red eye.
The knee is the most common joint involved, often bilateral followed by the ankles, elbows or wrists.
Vasculitis causes pain at the site of involvement causing painful swellings in the region, aneurysms, and occlusion of the vessel.
Involvement of the digestive system can cause abdominal pain and bleeding. Involvement of the central nervous system can lead to disorientation or stroke and other issues
Juvenile Idiopathic Arthritis
Juvenile idiopathic arthritis was formerly known as juvenile rheumatoid arthritis.
It is the most common type of arthritis in children less than 16 years
The condition is characterized by joint pain, swelling, and stiffness. Systemic signs like fever and rash could be present.
Subtypes of juvenile idiopathic arthritis are systemic-onset, oligoarticular and polyarticular. The title also includes psoriatic arthritis, enthesitis-related arthritis, and undifferentiated arthritis
Undifferentiated Spondyloarthropathy
In this subgroup of spondyloarthropathies, features are consistent with the spondyloarthropathies but the patients do not fulfill criteria for any specific spondyloarthropathy. This condition may represent ay represent either an early phase or incomplete form of specific spondyloarthropathy. However, certain features like the age of onset – 50 years, greater female preponderance and low association with HLA-B27 positivity does suggest that undifferentiated spondyloarthropathy is a separate entity.
Management is by nonsteroidal anti-inflammatory drugs and physical therapy mainly. Sulfasalazine has been suggested to have some role in the management of undifferentiated spondyloarthropathies.
Presentation
Patients usually present between 20 to 40 years of age.
Back pain, either lumbar or dorsal, buttock pain in single or both or alternating are chief presenting complaints. Pain is worse in the night and may be associated with stiffness in the morning.
Pain in peripheral joints, especially lower limbs may also be present.
Enthesitis [pain and tenderness at tendon insertion] and dactylitis [ inflammation involving a whole finger or toe] with tendovaginitis and arthritis (sausage digit) may be present.
Associated complaints depending upon the disease profile may be nongonococcal urethritis or cervicitis, or acute diarrhea one month or less before the onset of arthritis, psoriasis, balanitis or inflammatory bowel disease, anterior uveitis may be present. There might be a family history of spondyloarthropathy.
Differential Diagnoses
- Rheumatoid arthritis
- Prolapsed intervertebral disc
- Systemic lupus erythematosus
- Gout
- Osteoarthritis
Lab Studies
ESR and CRP are often raised in relation to disease activity. Rheumatoid factor as noted is negative.
Serum uric acid, antinuclear antibodies, bacterial serology should be done to rule other causes or know any association.
Imaging
Xray of the sacroiliac joints should be done for checking sacroiliitis. Xray of the affected painful part should be done. MRI may be needed in certain cases to rule out disc herniation. HLA testing is not normally done due to high false positive rates.
Management
Seronegative spondyloarthropathies depend on the type of spondyloarthropathy. NSAIDs, Disease-modifying antirheumatic drugs [DMARDs – sulfasalazine, methotrexate], TNF – blockers like etanercept, infliximab and adalimumab are the drugs used for management. Physiotherapy and occupational therapy are also used along with.
Surgery may be indicated in severely destroyed joints
Prognosis of Spondyloarthropathies
Spondyloarthropathies are associated with spontaneous remissions or exacerbations. The disease continues for many decades. Poor prognostic factors are
- Young age at onset (less than 16 years)
- ESR>30
- Hip arthritis
- Lumbar spine movement limitation
- Poor response NSAIDs
Image credit: Enthesis.info