Last Updated on November 22, 2023
Subacromial bursitis is inflammation of the subacromial bursa, a bursa that separates the superior surface of the supraspinatus tendon from the overlying coracoacromial ligament, acromion, coracoid (the acromial arch) and from the deep surface of the deltoid muscle. The subacromial bursa helps the movement of the supraspinatus tendon of the rotator cuff in activities such as overhead work.
The subacromial bursa is also called subacromial-subdeltoid bursa and bursitis is termed as subacromial-subdeltoid bursitis or SASD bursitis.
This bursitis of the shoulder is seen in people over 30 years old and has a greater incidence in females.
Subacromial bursitis may be present concomitantly with shoulder arthritis, rotator cuff tendinitis, rotator cuff tears, and cervical radiculopathy may be present.
Relevant Anatomy
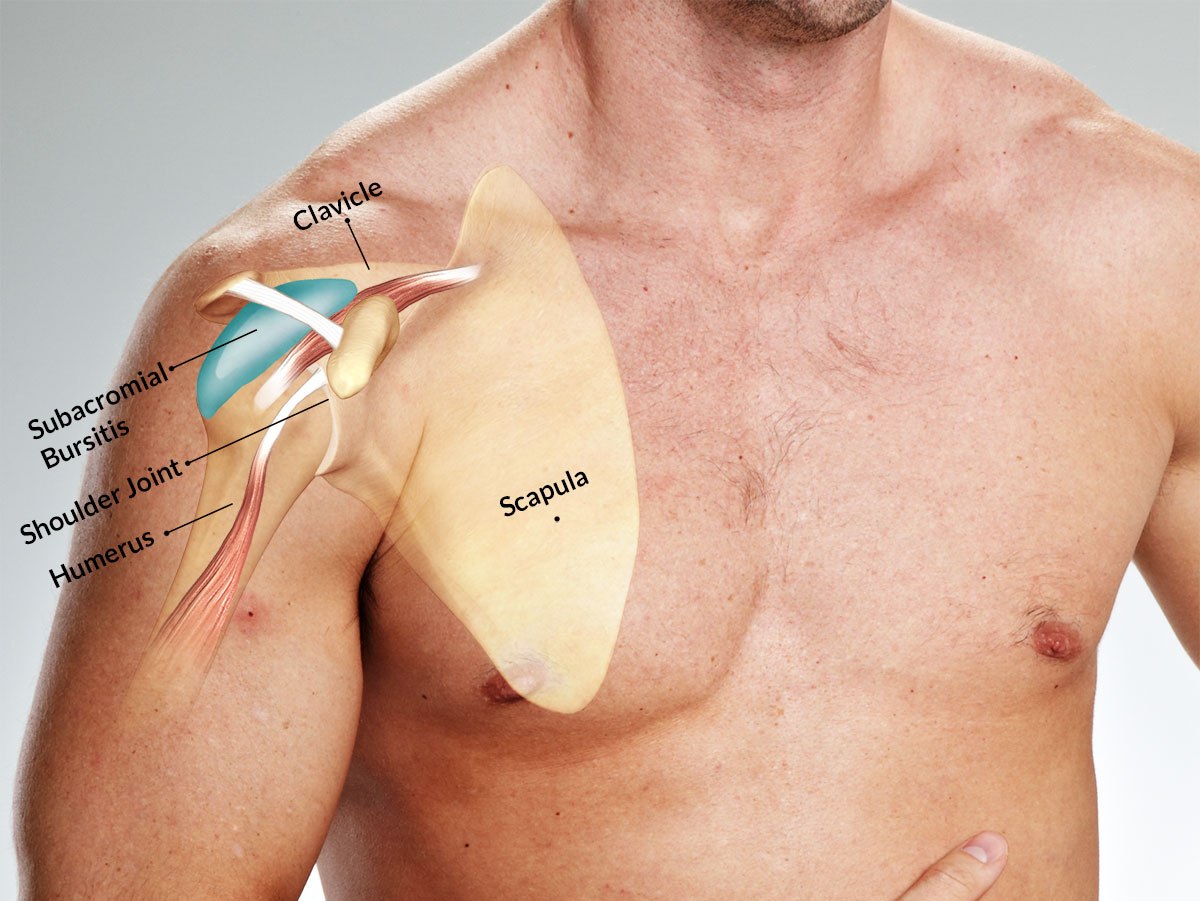
This bursa is deep to the deltoid muscle and the coracoacromial arch and extends laterally beyond the humeral attachment of the rotator cuff. Anteriorly, it overlies the intertubercular groove, medially to the acromioclavicular joint, and posteriorly over the rotator cuff.
The main function of the subacromial bursa is to decrease friction and allow smooth motion of the rotator cuff in relation to coracoacromial arch and the deltoid muscle.
Causes of Subacromial Bursitis
Subacromial bursa facilitates the motion of the rotator cuff beneath the coracoacromial arch. Any disturbance of the relationship of the subacromial structures can lead to impingement.
Known causes that cause subacromial bursitis are
- Rheumatoid arthritis
- Gout
- Pseudogout
- Infection
- Calcific loose bodies
- Acute Trauma
- Shoulder Overuse with overhead activities
- Throwing sports
- Swimming
- Professions – painting, carpentry, or plumbing
- Muscle weakness around the shoulder
- Rotator cuff degeneration
- Shoulder Pathologies
- Supraspinatus tendonitis
- Glenohumeral instability
- Acromioclavicular joint degeneration
- Rotator cuff tears
- Shoulder impingement syndrome
Presentation of Subacromial Bursitis
The presentation of subacromial bursitis is similar to shoulder impingement syndrome.
The patient complains of pain in the shoulder on anterior and lateral aspects. This may be associated with weakness and stiffness. The symptoms develop gradually.
[A weakness without pain may suggest rotator cuff tear or suprascapular nerve compression.]
Often the pain is present in the nighttime especially when the patient lies on the shoulder. There would be a history of frequent sleep interruption.
The patient may complain of an increase in pain on activities or pressure on the shoulder such as inactivity like leaning on an elbow may increase pain.
In severe cases, activities of daily living, household tasks and personal care may be affected.
On examination, the shoulder may appear normal. In case of infection, visible swelling or redness over the area may be present. The presence of fever may also suggest infection.
Tenderness is present over the anterior-superior aspects of the shoulder.
When the patient is asked to abduct the shoulder, the arc of the motion may be painful between 80 and 120 degrees. On lowering from full abduction there is often a painful catch at midrange.
Special Shoulder Tests
Speed Test
With arm extended and forearm supinated, the physician applies resistance while the patient attempts to flex the arm [shoulder joint]. A shoulder pathology like biceps tendonitis or bursitis would lead to pain.
Neer Test
The examiner performs maximum passive abduction possible in the scapular plane, with shoulder in internal rotation, while scapula is stabilized.
This causes impingement of supraspinatus tendon against the anterior inferior acromion.
It is often difficult to distinguish between pain caused by bursitis or that caused by a rotator cuff injury
Empty Can Test or Supraspinatus Test
The test can differentiate bursitis from supraspinatus tendinopathy as both might have overlapping features.
This test isolates supraspinatus muscle function. The patient is asked to abduct the shoulder to ninety degrees and internally rotated. Some authors advise elbow extension while others are not particular about this.
The arms are placed 30 degrees anteriorly (in the coronal plane) The examiner forces the arm downward while the patient resists.
Weakness or pain indicates supraspinatus involvement.
Differential Diagnoses
- Rotator cuff tear, partial or complete
- Rotator cuff tendinosis
- Subacromial impingement
- Rheumatoid arthritis
- Calcific tendonitis
- Pseudogout
Imaging
X-rays help to visualize bone spurs, acromial shape, and arthritis. Further, calcification in the subacromial space and rotator cuff may be revealed. Sometimes calcification are seen in the bursa itself.
MRI is not commonly done for bursa though it identifies bursitis quite well.
MRI can reveal fluid in the bursa and mark the affection of adjoining structures.
Ultrasound may reveal fluid distension, synovial proliferation, and/or thickening of the bursal walls.
Lab Studies
In case of suspected infection, aspiration of the fluid under imaging and its lab analysis should be done.
CBC, ESR, CRP may be done to rule out infection. In suspected rheumatoid arthritis cases RF or anti-CCP should be done.
Treatment of Subacromial Bursitis
When a patient presents with acute bursitis the aim of the treatment is to reduce the symptoms and minimize the damage. At the same time motion and strength is to be maintained.
Following modalities of the treatment are instituted
- RICE therapy [rest, immobilization, compresses and elevation]
- Drugs
- Anti-inflammatory drugs such as NSAIDs [Iboprofen, Aceclofenac, etc]
- Antibiotics in case of suspected infection
- Physical therapy modalities heat, ice, ultrasound, stretching and strengthening exercises
Initial management of subacromial bursitis involves immobilization with a sling and NSAIDs like naproxen or ibuprofen. For pain that remains disabling after 72 hours, steroid injection of the bursa may be indicated but infection should be ruled out.
In cases where these measures do not show improvement, intralesional steroid injections can be applied. These injections can be applied by palpation or by using ultrasound guidance. Intrabursal steroids may also be considered as primary treatment in patients who cannot tolerate NSAIDs.
As the pain reduces and inflammation subsides, the range of motion exercises are started.
These are followed by shoulder strengthening and stretching exercises.
Bursectomy, open or arthroscopic, is reserved for patients who fail to respond to non-operative measures.
Prognosis
Younger patients (< 20 years) and patients between 41- 60 years of age perform better than those who were in the 21- 40 years age group. Patients > 60 years of age had the poorest results.
References
- Lee JH, Lee SH, Song SH. Clinical effectiveness of botulinum toxin type B in the treatment of subacromial bursitis or shoulder impingement syndrome. Clinical journal Pain. 2011 Jul-Aug: 27,523 – 528
- Lee S, Park J, Lee D. The Effects of Cervical Stabilization Exercises on the Electromyographic Activity of Shoulder stabilizers. Journal Of Physical Therapy Science, 2013 December: 12, 1557 – 1660
- Chen, Max JL, et al. Ultrasound-guided shoulder injections in the treatment of subacromial bursitis. American journal of physical medicine & rehabilitation 85.1 (2006): 31-35.