Last Updated on November 17, 2023
The term lower cervical spine injury refers to the Injury of the subaxial cervical spine or that is below axis. It includes injuries to C3-C7 vertebra and adjoining structures.
Lower cervical spine injuries are common and are associated with significant mortality and morbidity.
The cervical spine can get injured during motor vehicle accidents or falls.
In trauma patients, it should be assumed that there is an injury to the cervical spine unless ruled out. Therefore, the cervical spine is protected in a patient of trauma, beginning at the accident site, during extrication, examination and shifting the patient.
Cervical spine injury has been known to occur in as many as 4.5% cases of blunt trauma.
The cervical spine is a mobile region enabling mobility in various planes and during any trauma, the head can act as a significant lever arm on the cervical spine and creating a wide range of injury patterns.
These injuries, minor or major, can affect the spinal cord and nerve roots, and depending on the level of the spinal injury cause various motor and sensory dysfunctions.
The injuries to the subaxial spine have a bimodal age distribution.
Motor-vehicle accidents, falls, and accidents resulting from recreational activities or sports are the leading causes of injuries to the lower cervical spine.
Relevant Anatomy
The cervical spine consists of seven vertebrae numbered C1-C7. C1 and C2 along with C2-C3 joint are considered upper cervical spine whereas below that is lower cervical spine.
[Read anatomy of the cervical spine in detail]
Biomechanics, and Pathophysiology
The subaxial cervical spine is seen as formed by two columns.
The anterior column consists of posterior longitudinal ligament and structures anterior to it [vertebral body and disc, anterior longitudinal ligament].
The posterior column includes
- Pedicles
- Laminae
- Facet joints
- Spinous processes
- Posterior ligament complexes
Posterior column often fails in extreme flexion or distraction and is able to resist tension. Posterior column failure may be associated with concomitant injury to the anterior column.
The zygapophyseal or facet joints are oriented at 45º to the axial plane, allowing a sliding motion. The joint capsule is weakest posteriorly.
Spinal nerves exit at the vertebral level. There are a total of eight cervical nerve roots.
The first root leaves above the atlas and last [C8] exits between the seventh cervical vertebra and the first thoracic level.
The cervical spine can get injured by various mechanisms that lead to bony or ligamentous failure.
The position of the head and neck at the time of impact and the direction of force causing injury results in the different pattern of injury seen.
Key components in cervical spine injury are force/load transmission and kinematics (motion). Mostly, cervical spine injury occurs due to both components being present in different proportions.
One can consider an axial compressive load applied to a single cervical vertebra as a fundamentally pure example of load transmission. Force can be applied in different directions like shear, torsion, tension.
Kinematics refers to cervical vertebral motion. The lower cervical spine that permits motion through intervertebral discs and facet joints and is limited by the anterior longitudinal ligament and posterior ligamentous complex. It can be in a flexion-extension plane, axial rotation and lateral flexion.
Flexion-extension motion is greatest at the C4-C5 and C5-6 segments, averaging about 20 degrees. Axial rotation ranges from 2 to 7 degrees at each of the subaxial motion segments. Lateral flexion is 10 to 11 degrees per level in C2-5 and decreases caudally.
Cervical spine injury alters both load transmission and the kinematics of the cervical spine. The cervical spinal column is extremely vulnerable to injury.
Classification of Lower Cervical Spine Injury
Allen described the following three common mechanisms for spinal injury in a descriptive classification. The various mechanisms described are
- Compression-flexion
- Distraction-flexion
- Compression-extension
Older classifications, including Allen’s, have following drawbacks
- Machinist
- Do not take into account the neural condition
- Unable to form a treatment protocol not guide the treatment
Subaxial Injury Classification (SLIC ) is based on —morphology, discoligamentous complex (DLC), and neurologic status. Each category has subpoints that are given a score. The final score is calculated by adding all the scores.
- Morphology
- No abnormality – 0
- Compression – 1
- Burst +1 – 2
- Distraction – 3
- Rotation/translation – 4
- Discoligamentous Complex
- Intact – 0
- Indeterminate – 1
- Disrupted – 2
- Neurologic status
- Intact – 0
- Root injury – 1
- Complete cord injury – 2
- Incomplete cord injury – 3
+1 is added when there is continuous cord compression along with neurologic deficit – +1
The score is used in decision-making for treatment
- < 4 Nonoperative treatment
- 4 Operative versus nonoperative
- 5or more – Operative treatment
Clinical Presentation
The cervical spine injury should be suspected in every major trauma.
For best possible in any given injury, the precautions of cervical spine begin at the field or first contact and continue till the spine is managed definitely.
The neck needs to be immobilized manually, with sandbags or cervical collar. These methods and use of spine board help to prevent secondary injury. Transfers and intubation should be accomplished under strict spine precautions. Log-roll technique and spinal precautions should be observed at all times.
Airway, breathing, and circulation should always be the highest priority.
Airway security and hemodynamic resuscitation are crucial and should take precedence. Tracheal intubation and central line placement are often performed in the emergency and due to a danger of worsening of injury by manipulation, manual cervical stabilization should be maintained throughout the intubation process.
If intubation is not possible, mask ventilation can be continued until fiberoptic or nasotracheal intubation can be safely performed in a hospital.
Cricothyroidotomy might be the safest alternative for airway control when the spine is highly unstable.
History should be taken to note the circumstances of accident and forces working. Mental status and consciousness level should be assessed.
Neurological functions, regions of pain and other injuries should be noted especially abrasions and/or laceration on the scalp, face, neck, or shoulders as clues to the mechanism of injury.
The back of the neck should be palpated for any tenderness, step-off, or hematoma.
Performa neurologic examination as soon as feasible as per ASIA.
The presence of pathologic reflexes like clonus Hoffman sign, and Babinski sign.
Often, in cases of acute cord injury, there is a spinal shock present, and a detailed assessment could only be done at a later date when spinal shock goes. The return of the spinal function is indicated by the bulbocavernous reflex. Therefore serial examination needs to be done to see if spinal shock has gone or not. It usually takes about 24 hours.
[Read more about spinal shock]
[Read more about spinal cord injury]
Depending on the spinal cord injury, different incomplete patterns of spinal injury may be seen.
[Bilateral facet dislocations have the highest incidence of spinal cord injury often resulting in incomplete/complete injury paterns]
Special attention should be paid to examine sacral roots and reflexes. Return of sacral reflexes indicates the end of the spinal shock. The bulbocavernosus reflex and anal wink are good tests of the sacral reflex arc.
A neurological examination should be regularly done to find if the lesion is improving or worsening. This helps in the guidance of the treatment.
The neurogenic shock when present should be recognized and managed.
Lab Studies
After the patient is stabilized, routine lab studies are indicated which include
- Complete blood count
- Urine analysis,
- Biochemistry tests of blood
- Serum electrolyte levels
- Liver and renal function testing
Imaging
X-rays
The standard x-ray imaging is a cross-table lateral view of the cervical spine that helps to gauge the cervical alignment. Other x-rays that could be included are odontoid view, and AP view.
A swimmer’s view may be needed to complete the evaluation.
In case, the x-rays are not able to visualize the spine properly, CT must be done to exclude the neck injury.
CT
CT scan is helpful in injuries of the cervicothoracic junction and posterior elements.
American Association of Neurological Surgeons (AANS) recommendations for CT
- Awake, asymptomatic patient without pain or neural deficit
- No radiographic evaluation required
- Awake, Symptomatic Patient
- High-quality CT
- Obtunded or unevaluable Patient
- High-quality CT or 3 3-view cervical series
MRI
MRI is able to visualize neural elements – cord and roots. Disc herniations can easily be seen on MRI.
A mismatch of injury levels on X-rays is another indication of MRI.
In case of vascular injury, as vertebral artery injury, magnetic resonance angiography may be indicated.
The artery is prone to be injured in case of sever degeneration of the spine and fractures through the foramina transversarium.
Management of Cervical Injuries
Acute Management
Management of cervical injury in the emergency requires treating the multiple injuries [often associated] and treating the concomitant neurologic injury.
Though the risk-benefit ratio has been questioned, steroids are given to prevent secondary cord damage and to minimize local edema.
For a patient presenting within 3 hours of injury, the dosage is
- 30 mg/kg loading dose of methylprednisolone given intravenously (IV) over 1 hour, followed by 5.4 mg/kg/hr for the next 23 hours.
If the patient presents after 3 hours but less than 8 hours
- the 5.4 mg/kg/hr dosage is extended for 48 hours following the same loading dose.
After 8 hours of injury starting patient on steroid does not appear to be beneficial.
Steroids are associated with poor wound healing, the risk of infection, stress ulcers and increased sugar levels. Therefore some clinicians avoid the use of steroids. Moreover, there appears insufficient to weak evidence for their effectivity.
Histamine 2 (H2) blockers such as famotidine and ranitidine) are given to prevent stress ulcers from spinal cord injury.
Prophylaxis for deep vein thrombosis is carried using low-molecular-weight heparin (LMWH), oral warfarin.
Intermittent compression devices for the lower extremities or vena cava filters may be used when required in high-risk cases
Approach to Definitive Treatment
After the patient is stabilized, the decision for the definitive treatment is based on
- Malalignment of the spine, with or without neural deficits
- Progressive neurologic deterioration associated with persistent compression.
Patients without malignment or without neural deficits [minimally displaced injuries] can be managed with nonoperative treatment.
Malalignment can be managed initially with cervical tong traction. Surgery is then done as definitive treatment. Decompression, when required, may be done.
In cases where the closed reduction is contemplated before the definitive treatment, the presence of concomitant disc herniations must be considered and if feasible confirmed with MRI. The discs with postero-inferior herniations are known to pose worsening of the neural deficit. [This is also important if the open reduction is planned.]
If MRI is not feasible, a cautious reduction while performing serial neurologic examination should be done in the awake patient.
But if the patient is intoxicated or has a head injury, MRI should be sought if patient condition allows.
A disc herniation if present should be removed anteriorly before performing the reduction.
The decision for surgery depends on the type of injury.
- For anterior column injuries
- Anterior approach
- Anterior decompression and reconstruction+grafting+ stabilization
- Posterior column injuries
- Posterior approach
- Posterior decompression/fixation/grafting
- Global injuries
- Anterior and posterior fixation approaches
Early intervention [within 24-72 hours] is recommended to facilitate early decompression and rapid return of the mobilization.
Nonoperative Treatment Options
A number of lower cervical spine fractures can be managed with nonoperative means. Nonoperative means of treatment include orthoses, skull traction, and halo vest immobilization.
The basic aim of nonoperative means is to align and immobilize the cervical spine and prevent it from further stress till the fracture union occurs.
Orthoses
Orthoses can be cervical or cervicothoracic.
Orthoses decrease motion rather than effect true immobilization.
Cervical Orthoses work through padded contact areas strategically located over subcutaneous bony prominences like occiput, spinous processes, scapular spines, acromion processes, clavicles, sternum, and mandible.
Soft cervical orthoses cause little decrease in spinal motion and are most commonly used after cervical strains or sprains.
Rigid cervical orthoses can provide varying degrees of immobilization depending on the construction material and the overall design. They are commonly used for emergent in-field cervical spine immobilization.
Skin breakdown at bony prominences can occur as a complication of cervical collars.
Cervicothoracic Orthoses devices extend to the upper thorax. These provide more effective immobilization than simple cervical collars in all planes. Sternooccipito-mandibular immobilizer –(SOMI) and Minerva brace are examples of cervicothoracic orthoses.
However, they are more difficult to apply and remove and produce high resting pressures on the chin and occiput.
Both cervical and cervicothoracic devices cause increased motion at the cervicothoracic junction.
[Read more about cervical orthoses]
Cervical Traction
Traction can be used for temporary immobilization of unstable cervical spine injuries, or to realign or reduce and maintain cervical spine fractures or dislocations. The devices used are Crutchfield’s tongs, Gardner-Wells tongs, and the halo-ring.
Halo Vest
Halo immobilization has become a less popular form of treatment for lower cervical spine injuries as the better internal fixation techniques have been developed. Despite this, halo vest immobilization remains a viable, minimally invasive method of stabilization of unstable cervical spine injuries for patients who might otherwise have contraindications to open surgical methods.
Surgical Treatment Options
With the increased choice of implants and gadgets and development of better surgical approaches & techniques, surgery is playing a greater role in the management of cervical injuries as compared to earlier times.
Anterior Surgery
The subaxial spine is reached by the interval plane between the sternocleidomastoid (lateral) and medial muscles. Following options are available with the anterior approach
- Decompression by removing offending structure
- Removal of the disc [discectomy]
- Removal of vertebra[corpectomy or vertebrectomy]
- Anterior Reduction of Dislocated Facets
- Reduction confirmed under C-arm
- Additional posterior surgery if reduction fails
- Reconstruction
- Replacement of the removed vertebra or disc.
- Autograft/ allograft/ titanium mesh cage.
- Stabilization
- Anterior locking plate
Posterior Surgery
- Midline extensile posterior approach
- Decompression
- Posterior decompression often not necessary
- Laminectomy needed to remove the offending compressive elements.
- Open reduction of dislocated facet joints can be performed using a posterior approach.
- Posterior Instrumentation
- Wire-based constructs
- Variable-angle screw-rod constructs.
- Posterior Fusion
- Cancellous bone harvested from the posterior iliac crest
Follow-up after Surgical Treatment
Rigid postoperative external immobilization is often not required after surgery. A cervical collar is generally enough.
Postoperatively, patients usually are maintained in a rigid or soft collar for comfort.
The patient should be mobilized out of bed as soon as possible to prevent pulmonary and thromboembolic complications.
Further management of the injury is
- Wound care in early postoperative period
- Early mobilization
- Physical, emotional and functional rehabilitation
- Management of bowel and bladder dysfunction
- Intermittent catheterizations
- Alternate-day suppositories
- High-fiber diet to avoid impaction.
Radiological sign of union is expected in about 2-3 months. Any deterioration in neurologic function should prompt further investigation.
Complications of Lower Cervical Spine Injury
- Spinal cord or root injury
- Pulmonary problems
-
- Pneumonia
- Atelectasis
- Pulmonary embolus
- Stress ulcers
- Pressure ulcers
- DVT
- Depression
- Autonomic dysreflexia
Cervical Injuries in Special Cases
Spondylitic Spine
These people can suffer cervical injury even after minor trauma. Therefore, those who present with neck pain or neurologic deficit after trauma should be considered to have a cervical spine injury until proven otherwise.
As degenerative changes make x-ray interpretation difficult, CT or MRI should be done in these.
Ankylosing Spondylitis and Diffuse Idiopathic Skeletal Hyperostosis
An ankylosed spine should be considered as a long bone as the mobile segments get fused.
Therefore any fracture in the cervical spine in these patients should be considered as unstable and treated accordingly.
Prognosis
The clinical outcome after lower cervical spinal injury generally is related to the level and severity of associated spinal cord injury.
If the neural functions do not return, the patient is left with disabilities depending on the level of injury.
[Read this article for knowing about different disabilities at different levels – Correlation between cord levels and vertebral levels]
Few Images of Lower Cervical Spine Injuries
Cervical Vertebrae Dislocation C5 Over C6
A young male of 34 years was brought to casualty with history of falling from a horse cart. He was quadriplegic [There was no power in any of the limbs]. On examination, he was found to be in spinal shock.
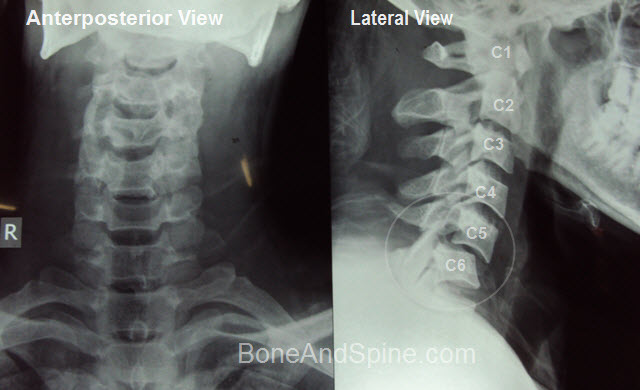
His MRI revealed a compression at the C5-C6 level along with cord edema.

C4-C5 Dislocation

MRI shows the dislocation and a disc compressing on the cord as well.

Fracture of C2 with anterolisthesis of C2 on C3
This is quite a serious injury and may cause respiratory distress.
References
- Vaccaro AR, Hulbert RJ, Patel AA, Fisher C, Dvorak M, Lehman RA Jr, et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976). 2007 Oct 1. 32 (21):2365-74.
- Toh E, Nomura T, Watanabe M, Mochida J. Surgical treatment for injuries of the middle and lower cervical spine. Int Orthop. 2006 Feb. 30(1):54-8.
- Furlan JC, Noonan V, Cadotte DW, Fehlings MG. Timing of decompressive surgery of spinal cord after traumatic spinal cord injury: an evidence-based examination of pre-clinical and clinical studies. J Neurotrauma. 2011 Aug. 28(8):1371-99.

