Last Updated on November 19, 2019
Synovial plica syndrome is referred to the group of signs and symptoms due to inflammatory changes in plica, an otherwise insignificant remnant of the synovial membranes of the knee.
Synovial plicae are normal structures found in many knees. Normally, they are asymptomatic and are not associated with any painful conditions. However, with an inciting event like repetitive microtrauma or major injury, they can become symptomatic.
Out of four plicae, the superior, the medial, and the inferior, and the lateral, medial plica is most commonly involved in plica syndrome. Occasionally, suprapatellar plica may also be symptomatic.
Synovial Plica Anatomy
Plica is a remnant of synovial membranes. During embryonic life [fetal development], the knee is not a single chamber is divided into three separate compartments by synovial membranes. These membranes are resorbed by third or fourth month and knee becomes and the knee becomes a single chamber. Incomplete resorption of membranes may various degrees of septation. These embryonic remnants are known as synovial plicae.
Plica in Latin simply means a fold.
Types of Plicae
There are four types of synovial plicae of the knee.
- Suprapatellar
- Mediopatellar
- Lateral
- infrapatellar
Suprapatellar
It is also called plica synovialis suprapatellaris, and it divides the suprapatellar pouch from the remainder of the knee. The separation may be complete or incomplete.
The suprapatellar plica usually begins proximal to the superior pole of the patella but variations may occur in origin. From there, it courses from the anterior to femoral metaphysis or the posterior of the quadriceps tendon to the medial wall of the joint.
The incidence of suprapatellar plica has been reported to be as low as 11% to 90%
Mediopatellar or Medial Plica
The mediopatellar or medial plica lies on the medial wall of joint. It also originates in suprapatellar area and courses in the coronal plane, obliquely down to insert on the infrapatellar fat pad.
This plica is also called a shelf.
Mediopaellar plica is the most frequently cited cause of synovial plica syndrome.
Medial plica has a reported incidence of 18-60% with average cited figure 20-25%.
Sakakibara classified medial plica into four types, as follows
- Type A
- A cord-like, thin elevation of the synovial wall, under the retinaculum.
- Type B
- A narrow synovium, with a shelf-like appearance, which does not cover the anterior surface of the medial femoral condyle.
- Type C
- A larger synovium, with a shelf-like appearance, which partially covers the medial femoral condyle.
- Type D
- A type C plica that is fenestrated, creating tags
This classification has clinical significance.
Types A and B are not likely to produce symptoms, while types C and D, due to their size, may become trapped and impinged between the patellofemoral joint.
Lateral
Lateral plica is rarely present. It is a wide, thick band located along the lateral parapatellar synovium. It inserts on the lateral patellar facet.
Infrapatellar
It is the most common plica and is also called ligamentum mucosum. It is bell-shaped remnant originates in the intercondylar notch, widening through the anterior joint space, and attaches to the infrapatellar fat pad.
The plica that is the least symptomatic of all plicae.
Cause of Synovial Plica Syndrome
The etiology of synovial plica syndrome not clear. Repetitive stress, major or repetitive trauma, loose bodies, osteochondritis dissecans, meniscal tears, or other aggravating knee pathology may lead to inflammation of plicae.
Injuries to plica can occur through various mechanisms.
- A direct blow to the plica
- Blunt trauma
- Twisting injuries
- Activities that involve repetitive flexion-extension of the knee (e.g., rowing, cycling, running)
- Any mechanism resulting in intraarticular bleeding or synovitis secondary to a loose body, osteochondritis dissecans, a torn meniscus, a subluxing patella or after arthroscopy.
Pathophysiology of Plica Syndrome
Normal plica is a soft, flexible pink structure which changes orientation and dimension with knee movement. Media plica and the medial femoral condyle remain in contact during the whole range of motion with the medial plica shifting medially when the knee moved from extension to flexion.
The onset of symptoms is usually delayed until adolescence and it may be related to a decrease in tissue elasticity with age and biomechanical changes during a growth spurt.
Inflammation leads to swelling and thickening of the plica, which develops scars, becomes inelastic and develops fibrotic appearance. It may change to a band like structure and form a bowstring.
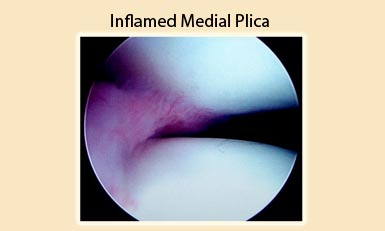
According to a theory, inflammation is caused when the plica is converted to a bowstring, causing an abrasion to the medial condyle. Impingement between the patella and the femoral condyle may occur, resulting in secondary mechanical synovitis. The patellofemoral joint mechanism is altered resulting in softening and degeneration of the articular cartilage and the development of chondromalacia.
Others say that a plica need not contact the femoral condyle to cause symptoms. Thickening of plica places excessive traction on its synovial insertion resulting in pain.
Presentation of Plica Syndrome
Synovial plica syndrome is a diagnosis of exclusion. The symptoms resemble or overlap with those of other pathology and the diagnosis may be difficult to arrive at.
Plica syndrome affects both genders equally and the main complaint is an intermittent dull ache pain located medial to the patella above the joint line and in the superomedial patellar area.
Pain increase with activity, especially with repeated knee flexion and extension as in climbing the stairs. [Sustained flexion of the knee increases pain while extension relieves it]. Popping also relieves the pain.
Knee giving way, clicking, catching, pseudo-locking, snapping, and tightness around the anteromedial or anterior knee aspect may also occur.
On examination, the knee usually appears without any swelling or effusion, though it could be present. Some atrophy of the quadriceps muscle may be present. In some cases, the patients have tender points along the medial and inferior aspect of the patella. On palpation, cord-like plica that pops and rolls under fingers may be felt, which may be tender as well.
Extension of the knee from 90° flexion, combined with internal rotation and medial gliding of the patella, may result in a characteristic popping sound and sensation that can be felt by the examiner’s fingers [usually occurs between 60° and 45°]
Holding Test
The patient holds the knee in extension while the examiner tries to flex the knee as he or she pushes the patella medially. Pain with or without clicking is considered as a positive test.
Magee Test
The knee is flexed at 30° flexion the patella is moved medially, provoking pain as the edge of the plica is pinched between the patella and the femur.
TARP [Taut Articular Band Reproduces Pain] Sign
A taut articular band that reproduces the patient’s pain upon palpation of the medial peripatellar region is virtually pathognomonic for plica syndrome. This may be referred to as a positive TARP sign.
Active Extension Test
The patient lies supine with the knee flexed at 90°. A quick extension of the tibia is performed as in kicking a football. Sudden pull of the quadriceps muscle on plica may result in pain.
The Flexion Test
The patient lies supine with the tibia extending out of the bed. The patient is asked to flex his knee quickly and examiner resits to stop that between 30° and 60° of flexion [blocking of the swing]. Plica is stretched with the eccentric contraction of the quadriceps and produces pain.
Both Active extension test and the flexion test improve the clinical accuracy of the diagnosis.
Differential Diagnoses
Common pathologies that imitate medial plica syndrome are
- Medial collateral ligament sprain
- Medial meniscal tear
- Pes anserine bursitis
- Bipartite Patella
- Knee Osteoarthritis
- Osteochondritis Dissecans
- Patellar maltracking
A pathological plica can be present in combination with other intraarticular pathologies and most common concomitant findings are meniscal tears, patellar tendinitis, Osgood-Schlatter disease, Sinding-Larsen-Johansson disease, and patellar instability.
Lab Studies
Lab investigations are generally not required for diagnosis.
Imaging
Diagnosis of synovial plica syndrome is mostly clinical but standing AP, lateral, and axial radiographs of the knee are done to rule out other pathologies. Most of the patients have normal x-rays. Underlying arthritis, osteochondritis dissecans, osteophyte, or any other bony pathology that could lead to pain or plica irritation should be ruled out.
Ultrasonography enables dynamic examination of the plica.
Magnetic resonance imaging has been found useful in the evaluation of thickness and extension of medial para-patellar plicae. CT is helpful in ruling out impingement.
Diagnostic Procedures
A definite diagnosis can be made using arthroscopy [though it is not recommended in most of the cases] but an arthroscopy can result in further irritation and scarring of the medial synovial plica so it is better approached without irritating the plica, like using the superolateral portal. Mere visualization of the patella does not indicate that plica is the cause of pain. To label a plica pathological, the following criteria must be met
- Plica must appear and impingement must be visualized
- Chondromalacia must be present in the areas of impingement
Treatment of Plica Syndrome
Most plica syndromes can be treated conservatively. Surgery should be considered when even after nonoperative treatment for 6 months, symptoms persist.
Conservative treatment includes
- NSAIDs
- Physiotherapy – Stretching, and strengthening exercises.
- Rest/activity restriction
- Intralesional steroid injection
Physical therapy should be done for 6–8 weeks after the initial examination. An intraarticular corticosteroid injection should be considered in patients who do not improve with a physical therapy program.
A patellar knee sleeve worn during sporting activities may also be a useful adjunct for many athletes.
Surgery
Once conservative treatment has failed, the surgical treatment that consists of arthroscopic plica excision should be carried.
After arthroscopic evaluation establishes that no other intraarticular abnormalities must be addressed, the plica can be resected.
If associated secondary pathological conditions are present (e.g., synovitis, medial patellar chondromalacia, or synovial pannus on the condyle), the plica must be resected, but failure can occur, as the secondary lesions may remain cause symptoms.
After the surgery, the patient is started on exercises for range of motion and strength.