Last Updated on November 22, 2023
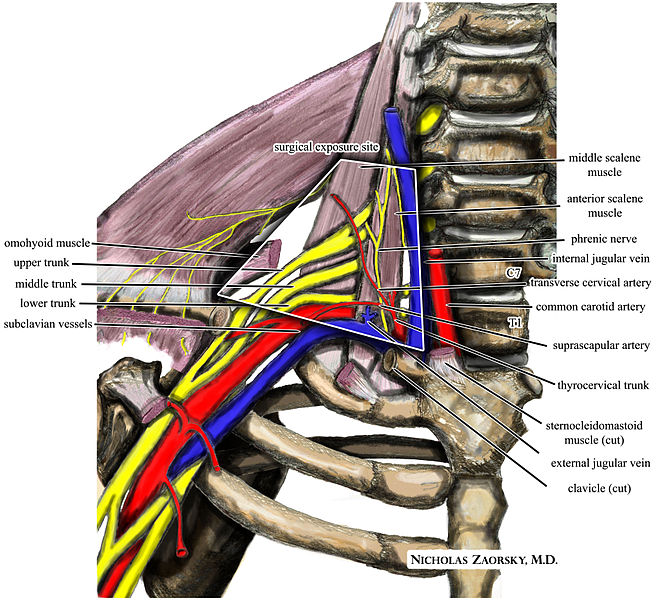
Thoracic outlet syndrome is a group of disorders involving compression of neurovascular bundle passing between the anterior scalene and middle scalene muscles as they pass between the chest and upper extremity. The structures that could be affected are the brachial plexus, the subclavian artery, and, rarely, the subclavian vein.
Note: Subclavian vein, normally, does not pass between scalene muscles.
Potential site for compression are
- Interscalene space [Space between the anterior scalene and middle scalene muscles]
- Costoclavicular space [between first rib and clavicle]
- Space below pecotralis minor
Causes of Thoracic Outlet Syndrome
Thoracic outlet syndrome may result from
- Dynamic compression such as abnormal compression from the clavicle and shoulder girdle on arm movement.
- Static compression caused by abnormalities such as the cervical rib
- Enlargement or spasm of the surrounding muscles
- Pancoast tumor (cancer in the apex of the lung) in the progressive stages of the disease.
- Physical trauma – accidents, repetitive strain injury, sports-related activities
- Pregnancy- Joints loosen during pregnancy, leading to bad posture. Any preexisting narrow thoracic outlet may become symptomatic.
- Congenital abnormalities – cervical rib, prolonged C7 transverse process, and muscular anomalies in the scalenus anterior or scalenus medius muscle, fibrous connective tissue anomalies.
Cervical rib syndrome, scalenus anterior syndrome, costoclavicular syndrome, hyperabduction syndrome are types of thoracic outlet syndrome named by the condition that causes it.
Scalenus Anterior Syndrome
The compression on brachial plexus and/or subclavian artery caused by muscle growth.
Cervical Rib Syndrome
The compression on brachial plexus and/or subclavian artery is caused by bone growth termed as the cervical rib
Costoclavicular syndrome
There is a narrowing between the clavicle and the first rib.
Risk Factors of Thoracic Outlet Syndrome
- Bony overgrowth in the clavicle or first rib. Some people are born with an extra incomplete and very small rib above their first rib, which protrudes out into the superior thoracic outlet space is called a “cervical rib” because of its attachment to C-7 (the 7th cervical vertebra). It causes compression and symptoms and signs of thoracic outlet syndrome.
- Congenital abnormalities
- Scalene muscle hypertrophy from athletic activities
- Congenital postural deficiencies such as scoliosis and drooping shoulders
- Rapid weight loss associated with vigorous physical activity
- Repetitive activity at work
- Professionals with frequent overhead arm activities [ swimmers, volleyball players, dancers, badminton players, baseball pitchers, and weightlifters, rock climbers, electricians who work long hours with their hands above their heads, and some musicians] are also considered to be at increased risk.
Signs and symptoms Thoracic Outlet Syndrome
Symptoms of Thoracic outlet syndrome symptoms vary depending on which structures are compressed.
Neurological Thoracic Outlet Syndrome
This type is caused by Caused by compression of the lower portion of the brachial plexus by a band of tissue that joins the transverse process at C7 to the first rib. It is the most common form and accounts for 94% cases. It affects women more than men.
- Wasting in the fleshy base of the thumb (Gilliatt-Sumner hand)
- Numbness or tingling in arm or fingers
- Pain or aches in your neck, shoulder or hand
- Weakness of the grip
Vascular Thoracic Outlet Syndrome
It can be divided further into arterial or venous.
Arterial Thoracic Outlet Syndrome
It is caused by the compression of the subclavian artery and accounts for only about 1% of all cases of thoracic outlet syndrome. It is the most serious form of the syndrome and affects men and women equally.
Symptoms include
- Spasm of vessels of hand leading to pallor in one or more of fingers
- Thrombosis or embolism of the arteries leading to weak or no pulse in the affected arm, cold fingers, hands or arms
- Weakness of arm or neck
- Aneurysm
- Muscle atrophy, and gangrene
Sometimes affected subclavian artery can lead to the affection of vertebral artery leading to cerebrovascular arterial producing transient blindness, and embolic cerebral infarction.
Venous Thoracic Outlet Syndrome
It results from the compression of the subclavian vein and accounts for about 4% of all cases and affects young men mostly.
It is characterized by arm claudication, edema, cyanosis, venous dilatation, arm pain, and swelling, possibly due to blood clots
Paget-Schroetter Syndrome or effort-induced thrombosis can be the first sign of subclavian vein compression due to thoracic outlet syndrome.
Special Tests For Thoracic Outlet Syndrome
It must be noted that none these tests is able to reliably diagnose or rule out thoracic outlet syndrome.
Adson’s test
It tests thoracic outlet syndrome at the scalene triangle. The patient is examined standing and the radial pulse is palpated while moving the upper extremity in abduction, extension, and external rotation. The patient then is asked to rotate her head toward the involved side while taking a deep breath and holding it. A positive exam will result in a diminished or absent radial pulse.
Costoclavicular Test
Also called military brace test, in costoclavicular maneuver, the patient’s shoulders are drawn inferiorly and posteriorly. If the patient has a reproduction of arm pain or numbness, consider thoracic outlet syndrome. Radial artery palpation can also diminish in addition to this.
Elevated arm stress test[EAST]
Patient raises arms over the head, then opens and closes fists for approximately 3 minutes. If this reproduces symptoms, it is likely that he has thoracic outlet syndrome.
Stick em up Hand Raise or Hands-Up Test
For up to 3–5 minutes, both hands are held at right angles over the head bent at the elbows, with or without opening and closing of the fingers and a positive test occurs when the affected hand quickly becomes paler than the unaffected because of compromised blood supply.
Compression Test
Exerting pressure between the clavicle and medial humeral head causes radiation of pain and/or numbness into the affected arm.
Imaging in Thoracic Outlet Syndrome
X-rays
Mostly xrays are normal. A cervical rib if present may be noted in x-rays
Doppler Ultrasound
This tests the arterial flow through the radial arteries, with and without having the patient perform various arm maneuvers providing strong evidence of impingement of the subclavian artery at the thoracic outlet. The test, however, would not diagnose neurogenic TOS, by far the most common subtype of TOS.
Treatment of Thoracic Outlet Syndrome
Most of the thoracic outlet patients respond to conservative measures like improved personal habits, medications, rest, physical therapy, and massage, and stretching. A minority of patients with signs and symptoms of thoracic outlet syndrome need surgery.
Personal Habits
Excessive weight may contribute to symptoms in those with underlying anatomic predisposition and normal weight needs to be maintained or achieved. Posture improvement better sleeping habits like avoiding sleeping on the stomach, shoulder strengthening exercises.
Physical Therapy
Stretching and physical therapy help to relieve compression in the thoracic outlet, reduce blood vessel and nerve impingement, and realign the bones, muscles, ligaments, and/or tendons that are causing the problem.
Physical therapy can include a passive or active range of motion exercises of neck and shoulder girdle. Active breathing exercises and ergonomic desk setup and motion practices help to maintain good posture.
Medications
Nonsteroidal anti-inflammatory medications ease the pain and reduce swelling. Botox injections injected into the tight or spastic may eliminate pain or reduce it enough for the victim to undergo physical therapy and, hopefully, be able to properly stretch and reduce compression in the affected area.
Surgery
Surgical approaches aim at the removal of the offending structure that leads to compression. Like in cases where the first rib is compressing a vein, artery, or the nerve bundle, the first rib and scalene muscles, and any compressive fibrous tissue can be removed.
A cervical rib that causes the compression can be removed similarly.