Last Updated on December 1, 2023
Burst fractures are defined as vertebral fractures with the failure of the anterior and middle columns. The fractures are unstable as there is involvement of two columns, anterior and middle, out of three columns of the spine.
Burst fractures represent about 10% to 20% of thoracolumbar injuries. The term was given by Holdsworth and the 3-column theory by Denis explains the mechanism and definition. As per Denis, the burst fracture is compression of the anterior and middle vertebral columns leading to retropulsion of a fragment of the posterior vertebral body fragment into the spinal canal.
Burst fractures are caused by axial loading with flexion and can be considered as high-energy compression fractures that result in disruption of the posterior vertebral body cortex with retropulsion into the spinal canal.
L1 is the most common vertebra involved with the majority of the burst fractures occurring at T9-L5.
The majority of these fractures are single-level fractures. Most of these are seen with high-energy injuries like motor vehicle accidents and falls from height.
Holdsworth described burst fractures in 1963.
Relevant Anatomy
There are 12 thoracic and 5 lumbar vertebrae. The first ten vertebrae are relatively fixed due to being attached to the ribs and sternum. T10 to L2 is considered as the thoracolumbar junction which is a kind of transition region from rigid thoracic to flexible lumbar spine. But this feature predisposes this region as to injury risk as it acts as a stress riser.
Denis Classification of Vertebral Column
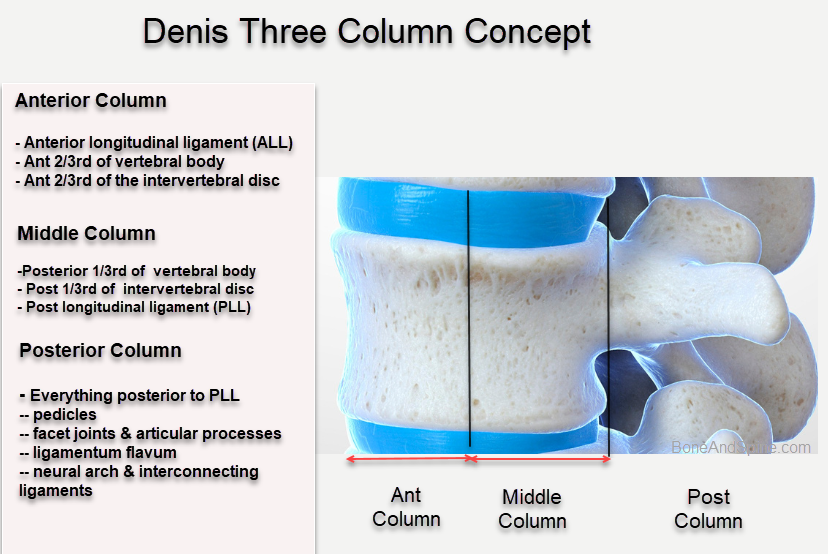
- Anterior column: Anterior longitudinal ligament, anterior 2/3 of vertebral body and anterior 2/3rd of vertebral disc (annulus)
- Middle column: Posterior longitudinal ligament, posterior 1/3 of the vertebral body and posterior 1/3rd of the vertebral disc (annulus)
- Posterior column: Pedicles, lamina, facet joints and articular processes,ligamentum flavum, spinous process and posterior ligament complex
The posterior ligamentous complex is very important in predicting the stability of spinal fractures. The complex is formed by supraspinous and interspinous ligaments, ligamentum flavum and facet capsule.
Injury to the posterior ligamentous complex indicates the injury to the posterior column and renders the injury unstable.
Pathophysiology of Burst Fractures
The term burst fracture implies that the margins of the vertebral body spread out in all directions.
Burst fractures are caused by falls from height or motor vehicle accidents.
The mechanism of burst fracture is axial load exerted on the vertebral column. The fracture anatomy is changed by associated flexion and rotation of the vertebrae at the site. [See classification below]
Injury to just the anterior column results in a compression fracture. In a burst fracture, there is an injury to the middle column along with the anterior column. This is a much more severe injury than a compression fracture as it increases the risk of spinal cord injury.
A high-energy compression force drives the intervertebral disc into the vertebral body below. The anterior cortex fails in compression, and either one or both the endplates can get fractured. The middle column also fractures and a portion of the body gets retropulsed backward into the canal. The posterior elements may be injured as well.
There is often canal compromise often caused by retropulsion of bone. The maximum canal occlusion and neural compression occur at the moment of impact.
Injury to the middle column results in instability of the spine.
Injury to the middle column is signified by
- the widening of interpedicular distance on AP radiograph
- and loss of height of the posterior cortex of the vertebral body.
Injury to the posterior ligamentous complex further adds to instability.
Associated Injuries
- Spinal cord injury: Injury to the cord occurs frequently with burst fractures as retropulsion of fragments may lead to cord compression. Maximum trauma to the cord occurs at the time of the impact.
- Concomitant Spine Injuries: Injuries may also occur at other spinal levels
- Visceral Injuries: Injuries to abdominal viscera and chest may occur. There may be an injury to the bowel, lung, liver, spleen, and urinary tract among others.
- Long Bone Fractures: Concomitant fractures of other bones may occur depending on the severity of the injury
Classification of Burst Fracture
Burst fractures may be subdivided by fracture pattern as follows [Denis classification]. This classification has a limited role in treatment guidance and is just mechanism-based. It also does not include a neural deficit in classification severity
- Type A
- Occurs due to axial loading
- Fractures of both upper and lower-end plates
- Retropulsion into the canal.
- Type B (Most common type}
- Axial loading and flexion
- Only the superior end plate is fractured.
- Type C
- Axial load and rotation
- Rare
- Disruption of only the lower-end
- Type D
- Axial loading and rotation
- May be viewed as fracture dislocation
- Rotation of one body relative to the other occurs
- Type E
- Burst fracture in lateral flexion.
TLICS classification is more preferred now as it helps in treatment guidance.
Presentation of Burst Fracture
Burst fractures are high-energy injuries. Therefore most of the patients are seen in emergency set up with injuries to the back and concomitant injuries involving other parts of the body. Some o the [patients could be critical and injury protocols of ABC- airway, breathing, circulation must be followed. The spine would be examined only after other critical injuries have been responded to and the patient is stabilized.
A conscious patient is able to guide to the region of injury whereas in an unconscious patient, imaging needs to be relied upon for the location of the injury.
Apart from a skin condition, tenderness, and deformity, a neurological examination is carried out. In the initial hours, there may be spinal shock and accurate neurological examination may be possible only after this has gone which is usually not more than 24 hours but rarely could take longer.
Neurologic exams should include testing of the muscle strength, sensation, and reflexes of the lower extremities, as well as, testing of bowel and bladder sphincter control.
Depending on the level of spinal cord injury (spinal cord ends at T12-L1), various possible neurological deficits can result from burst fractures of the thoracolumbar spine.

Imaging
Radiographs
Xrays are a basic investigation and it is recommended to view the entire spine as concomitant spine fractures may be present. Anteroposterior and lateral views are standard views. X-rays might reveal
- Loss of vertebral height on lateral view:
- The anterior part is commonly more compressed than the posterior
- The fracture line involves the posterior cortex of the vertebra
- Posterior element fracture in severe injuries
- Retropulsion of bone [Only significant displacement and chunk visible on x-ray]
- Widening of pedicles – increase in interpedicular distance
- Indicates injury to the middle column
CT scan
CT defines the fracture better. It is done in cases where the x-ray films are inadequate. Sometimes, x-rays may be skipped to favor CT images as these have higher sensitivity. CT can better assess the extent of retropulsion of the fragment.
However, CT has a role in visualizing soft-tissue injuries.
MRI
MRI is very useful in assessing soft-tissue injuries including ligaments, discs, spinal cord, and nerve roots.
A myelogram CT may be done when an MRI is indicated but cannot be done.
It is useful to evaluate spinal cord or thecal sac compression and provides insight into the amount of injury to the cord.
It also highlights cord edema or hemorrhage and injury to posterior ligament complex.
Treatment of Burst Fractures
Principles of Treatment
Surgery is often the primary line of treatment. Nonoperative treatment has a limited role when a neurological deficit and instability are present. In other cases, the nonoperative treatment may be considered as indicated.
The goals of surgical treatment are
- Neural decompression- By reduction of fracture if needed and relieving compression by removal of offending structure (for example – bont fragment or disc)
- Stabilization in as anatomical position as possible – by implant fixation
- Fusion- Neurological Decompression
Anterior decompression by the anterior approach is considered better than the posterior. However. treating the surgeon’s experience, familiarity, and confidence in the procedure always counts.
When there is instability in all three columns, both anterior and posterior surgery is required. It can be done in one sitting or as a staged procedure.
Therefore integrity of posterior ligamentous complete is of paramount importance in burst fractures as that would guide the treatment. All fractures with disrupted posterior ligamentous complexes are deemed as unstable. These are high risk fractures for neurological deterioration and deformity progression (kyphosis) without surgery.
Once disruption is confirmed, stabilization and fusion should be considered especially for patients who do not have neurological deficit. The insult is posterior ligamentous complex is indicated by **
- Widening of the interspinous distance
- Increase in joint space of facets (facet diastasis)
- Kyphosis > 30 degrees
- More than 50% loss of vertebral height
**Milder degrees of injuries to the posterior ligamentous complex may not be determined and there are studies suggesting that patients may be managed without surgery too despite these red flags.
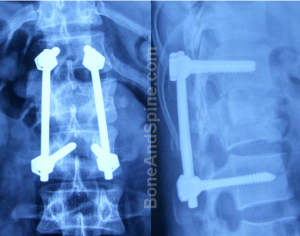
Stabilization is done using implants like
- Screws and rods
- Plate-screw systems
Fusion is done with bone graft. It can be autograft or heterograft. Bone graft substitutes have been used successfully too.
Read more about bone grafts and their uses.
Nonoperative
Indications of Non-operative Treatment
- Mechanically stable patients without neural deficit
- Kyphosis<30 degrees
- Vertebral height loss < 50%
- Neurologically intact and mechanically stable patients
- TLICS score is 3 or less
- Spinal canal compromise is less than 50 percent.
In these patients, treatment with a brace may lead to an excellent result. Bracing can be used to immobilize stable burst fractures. It can be in the form of thoracolumbosacral orthoses. The usual period of immobilization is for 3 months. After the brace is applied, the patient is radiographed to check stability, loss of height or increase in kyphosis [All these indicate underlying posterior ligamentous insufficiency].
If everything is satisfactory, the patient is mobilized with physical therapy.
Frequent x-rays for follow up are done. Occasionally, a fracture that was thought to be stable and treated in a brace may begin to angulate while in the brace. This may necessitate a later decision to perform surgery.
Recent studies have suggested no clear advantage of orthosis but if it provides the patient relief, it should be given.
The retropulsed fragments resorb over time and usually do not cause neurologic deterioration.
Operative Treatment
Surgical decompression & spinal stabilization is indicated in the neurologic deficits with radiographic evidence of cord/thecal sac compression.
The treatment is advised to both complete and incomplete spinal cord injuries.
As per TLICS score, it should be 5 or higher for operative treatment.
The spine is approached wither through an anterior and posterior approach.
Early surgery should be done in unstable burst fractures. Instability is suggested by
- Neural injury
- Spine angulation is more than 20 degrees
- Subluxation or dislocation of the spine
- More than half of spinal canal is compromised
Complications
Thoracolumbar burst fractures being high-energy fractures can result in a variety of injuries (in addition to spinal injury) and their after effects. we are here restricting to complications of spine injury only
- Persistent pain
- Progressive kyphosis
- Occurs often with loss of posterior ligamentous integrity
- Syringomyelia
- Surgical treatment complications
- Dural tears
- Infection
- Root injury/entrapment
- Pseudoarthrosis or failure to fuse
References
- Hsu JM, Joseph T, Ellis AM. Thoracolumbar fracture in blunt trauma patients: guidelines for diagnosis and imaging. Injury. 2003;34:426–433. [Link]
- Alpantaki K, Bano A, Pasku D, Mavrogenis AF, Papagelopoulos PJ, Sapkas GS, et al : Thoracolumbar burst fractures: a systematic review of management. Orthopedics 33 : 422-429, 2010
- Pneumaticos S.G, Triantafyllopoulos G.K, Giannoudis PV. Advances made in the treatment of thoracolumbar fractures: current trends and future directions. Injury. 2013;44:703–712. [Link]
