Last Updated on August 27, 2023
Thoracolumbar Junction Syndrome is characterized by pain that may originate at the thoracolumbar junction. Thoracolumbar junction syndrome is also called Maigne Syndrome or Dorsal Ramus Syndrome or posterior ramus syndrome. It is caused by the activation of the spinal nerve of the thoracolumbar region.
In the absence of any radiological signs, the diagnosis is made clinically.
The thoracolumbar junction (TLJ) is comprised of the T10-11, T11-12 and T12-L1 motion segments. This transitional area interposed between the thoracic and lumbar spine, is often the source of a characteristic pain syndrome characterized by a referral of the pain in the related dermatomes (T10 to L1).
Relevant Anatomy
The thoracolumbar junction is the junction between the thoracic spine and the lumbar spine usually spanning from the eleventh thoracic vertebra to the first lumbar vertebra. Here, the spinal curvature changes from kyphosis to lordosis, and the orientation of the facet joints changes from coronal to sagittal.
The change in vertebral anatomy adapting to lumbar anatomy can be noticed in last two thoracic vertebrae.
The thoracolumbar junction is important because it marks the change of region.
A thoracolumbar transitional vertebra is defined as a vertebra with partially retained features of the thoracic and lumbar segments at the thoracolumbar junction.
Maigne syndrome is due to activation or irritation of the dorsal or posterior ramus of the T 12 spinal nerve mostly.
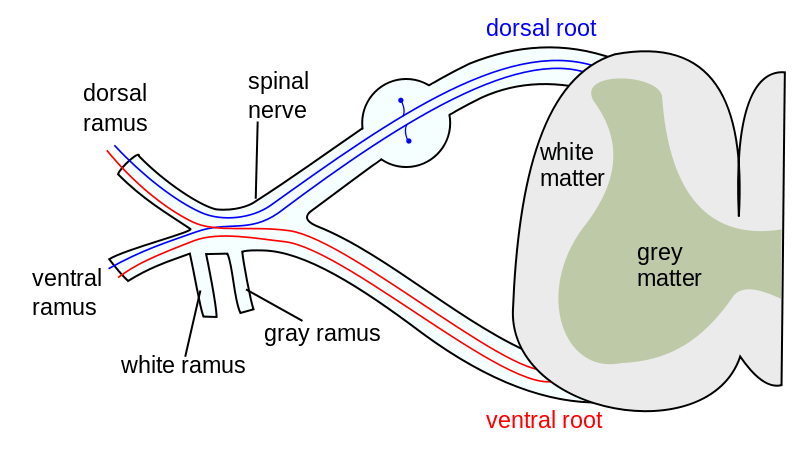
Each spinal nerve is formed by the combination of anterior and posterior roots for that particular spinal segment.
The spinal nerve emerges from the spinal column through the intervertebral foramen and divides into
- dorsal or posterior ramus – supplies the posterior part of the trunk and skin
- ventral or anterior ramus- supplies the anterior part of the trunk and skin
- rami communicants – visceral motor and sensory function
The thoracolumbar primary rami [mainly T12, L1] divides after a few millimetres into medial and lateral branches.
- The medial branch
- Runs dorsally along the angle between the transverse and zygapophyseal processes of the corresponding vertebra
- Gives off branches supplying the facet at that level.
- Lateral branch
- Directed caudally, laterally, and dorsally
- Supplies the erector spinae
- Supplies subcutaneous tissues of the lumbar and buttock area as distal as the greater trochanter.
The anterior ramus supplies the lower abdomen and groin.
Causes of Thoracolumbar Junction Syndrome
Irritation of the posterior ramus of the nerve is the major pain mechanism.
The most common cause of thoracolumbar junction syndrome is a minor intervertebral dysfunction at the thoracolumbar junction.
The nature of this dysfunction remains unknown, although the involvement of either the facets or the disc is very likely.
Thoracolumbar junction syndrome participates in the rotatory movements of the spine.
This may lead to an overuse of the motion segment which could initiate disc or facet degeneration. Disc herniation or a collapse of the vertebral body of T11, 12 or L1 may also be responsible.
A list of probable causes is given below
- Inflammation and degeneration of thoracolumbar junction (T9-L2) facet joints
- Intervertebral disc prolapse in the thoracolumbar region
- Nerve lesions
- Other degenerative processes
- Traumatic fractures
- Nerve entrapment
- Cutaneous dorsal ramus of L1 at the iliac crest
- Lateral cutaneous branch of the iliohypogastric nerve
Clinical Presentation of Thoracolumbar Syndrome
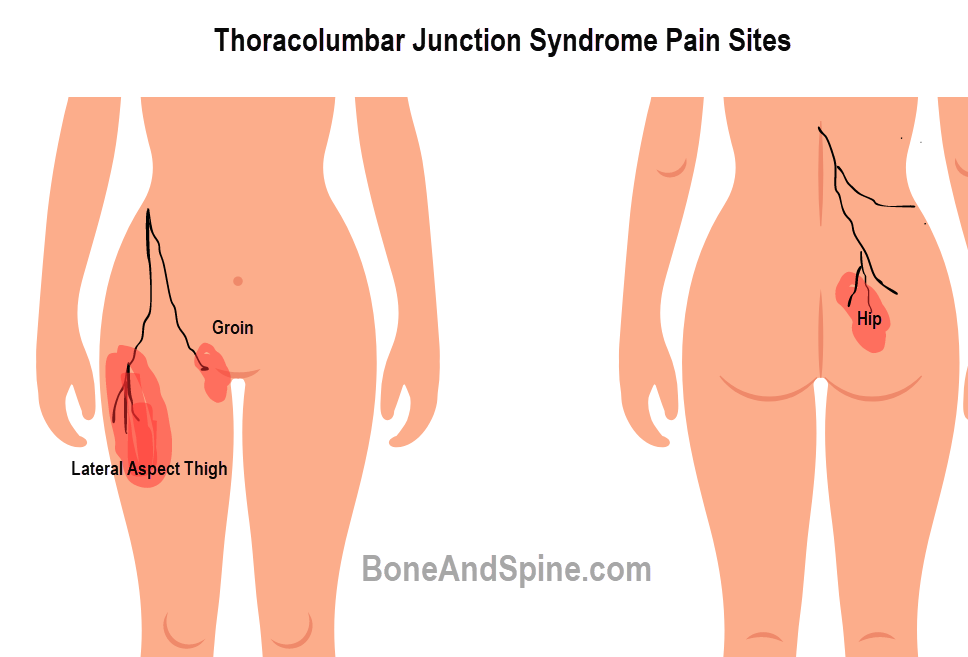
Depending on the branch involved, the pain could refer to
- Low back (cutaneous dorsal rami)
- The groin (subcostal or iliohypogastric nerve)
- Lateral aspect of the hip (lateral cutaneous rami of the subcostal or iliohypogastric nerve)
All combinations of these clinical presentations are possible.
The pain most frequently is only on one side (unilateral) of the spine and usually radiates along the pathway of the affected nerves leaving the TLJ.
Low Back Pain is certainly the most frequently encountered pain complaint. The pain is usually spread in the lateral part of the lower back without corresponding exactly to a specific dermatome.
Rarely, the pain is bilateral.
The pain is usually acute, of less than 2 or 3 months duration, often appearing after a rotatory movement of the trunk, prolonged strenuous posture, lifting, and occasionally, without any obvious precipitating factors.
Less commonly, the pain may become chronic.
The pain is frequently increased by contralateral side bending.
On examination, there is pain and tenderness in the iliac crest at a point that is consistently located seven centimetres from the midline. The pressure at this point causes a sharp excruciating pain similar to the patient’s complaint.
The opposite iliac crest is commonly unaffected.
The pinch-roll test
It can be revealed by gently grasping a fold of skin between the thumbs and forefingers, lifting it away from the trunk, and rolling the subcutaneous surfaces against one another in a pinch-and-roll fashion. On the involved side, the skin overlying the buttock and iliac crest is found to be tender when compared to the opposite side.
Examination of the thoracolumbar junction area may produce tenderness.
The affected posterior ramus ends cutaneously causing trophic changes in the skin.
Diagnosis
Diagnosis is mainly clinical. Imaging may be used to rule out any lesions of the spine or nerves.
Imaging
Radiographic is non-contributory. MRI, CT, and myelography are generally inconclusive unless a lesion is present.
Diagnostic Block
The pain is relieved by the injection of local anaesthetic into the correct facet joint. This diagnostic procedure can also be therapeutic.
Treatment of Thoracolumbar Junction Syndrome
The treatment involves the administration of anti-inflammatory drugs, spinal manipulation, and anaesthetic blocks.
The treatment has the following objectives
- Reduction of inflammation and pain
- Range of motion
- Pelvic tilt
- Hip exercises
- Muscle strengthening
- Posture training
For pain reduction following modalities may be used
- Cold therapy
- Electrical stimulation
- NSAIDs
- Intralesional corticosteroid injections
References
- Kim SR, Lee MJ, Lee SJ, Suh YS, Kim DH, Hong JH. Thoracolumbar Junction Syndrome Causing Pain around Posterior Iliac Crest: A Case Report. Korean J Fam Med. 2013 Mar;34(2):152-5. doi: 10.4082/kjfm.2013.34.2.152. [Link]
- Alptekin K, Örnek NI, Ayd?n T, Alkan M, Toprak M, A Balc? L, Öncü Alptekin J. Effectiveness of Exercise and Local Steroid Injections for the Thoracolumbar Junction Syndrome (The Maigne’s Syndrome) Treatment. Open Orthop J. 2017 May 31;11:467-477. doi: 10.2174/1874325001711010467. [Link]