Last Updated on November 11, 2023
Thoracolumbar spine injuries refer to injuries of the thoracic and lumbar spine. Injuries to both these regions are considered together because the pattern of injury and their treatment is similar. Thoracolumbar spine injuries are responsible for 90% of all spinal injuries.
These injuries occur most frequently in male patients between 15 and 30 years of age.
The majority of injuries occur within the region between T11 and L1, commonly referred to as the thoracolumbar junction.
15% to 20% of thoracolumbar fractures and dislocations are associated with a neural deficit.
Most of the thoracolumbar spine injuries are caused by blunt trauma in motor vehicle accidents. Two-wheeler accidents account for most of the cases. However, there is an increase in the number of injuries due to gunshot wounds and fractures in the osteoporotic spine.
Relevant Anatomy
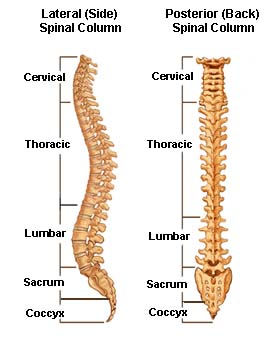
he thoracic spine is also called the dorsal spine and is constituted by the next 12 vertebrae after the cervical spine. These vertebrae are named T1 to T12 (or D1 to D12) from above downwards.
The lowest vertebra of the thoracic spine, T12, connects with L1, or the first vertebra in the lumbar spine. Between these two are ten other thoracic vertebrae connected to each other.
Lumbar spine consists of 5 vertebrae linked by joint capsules, flexible ligaments/tendons, and muscles.
Lumbar spine consists of 5 lumbar vertebrae named L1 to L5. The topmost lumbar vertebra is designated as L1 and it articulates with the D12 vertebra of the dorsal spine. The lowermost lumbar vertebra is L5 which articulates with S1.
Most of the thoracolumbar spine injuries occur in the area of the lower thoracic and upper lumbar spine.
Thoracic injuries are more devastating due to the vertebral canal being narrow and a blood supply that is precarious at best.
Fractures from T2-T10 are less common as this region of the spine is relatively stable [attached to ribs, coronal orientation of facet joints, and relatively thinner disc). Most of the fractures are of compression and burst type.
Thoracolumbar spine injuries in areas T11 to L2 are more common as the region acts like a fulcrum and is between fixed thoracic and flexible lumbar spine.
The spinal cord ends at L1-L2 and beyond that cauda equina [bunch of nerve roots are present. Hence thoracic spine fractures and L1 fractures are more commonly associated with
cord injury.
Injuries below L1 are associated with root damage but have a better prognosis than higher thoracolumbar spine injuries.
Normal Mechanics of Thoracic and Lumbar Spine
Thoracic and lumbar spine contribute to the height of the torso and roughly extend from below the neck to about the iliac crest. The thoracic spine has 12 vertebrae from T1 to T12 whereas the lumbar vertebrae are five in number.
The lumbar spine is much more flexible than the thoracic spine. The thoracic spine is rigid by virtue of the presence of the rib cage, thoracic musculature, and facet joint configuration.
The thoracolumbar junction represents a biomechanical transition zone between the rigid thoracic spine and flexible lumbar spine. It is the place where most of the thoracolumbar spine injuries occur.
Normally the thoracic spine has kyphosis whereas the lumbar spine has lordosis. The thoracolumbar junction represents the area of change in sagittal alignment between the kyphotic thoracic segment and a lordotic lumbar region.
This happens because the lumbar facet joints are more oriented sagitally.
[Read more on Thoracic spine anatomy]
[Read more on lumbar spine anatomy]
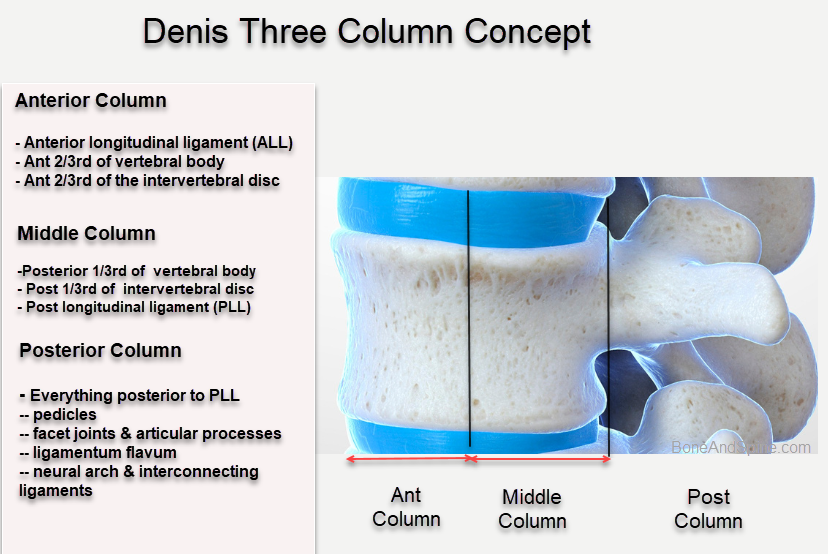
Denis developed a concept of three columns
- Anterior Column
- Anterior longitudinal ligament
- The anterior half of the vertebral body
- The anterior portion of the disc (annulus fibrosis)
- Middle Column
- Posterior longitudinal ligament
- Posterior half of the vertebral body
- Posterior aspect of the annulus fibrosus
- Posterior Column
- Neural arch
- Ligamentum flavum
- Facet capsules
- Interspinous ligaments.
According to the column concept, at least two of three columns should be injured to result in instability of the spine.
Mechanism of Injury
Forces acting on the spine result in spine fractures. Many authors in the past have attempted to classify thoracolumbar spine injuries based on the mechanism of injury. Earlier the authors divided the spine into 2 columns but after Denis, the three-column concept has been used extensively. The following mechanisms of injury are based on those concepts given by Denis.
But the mechanism of injury as provided by Denis is a good way to understand the forces and patterns of fracture resulting from that. Forces acting on the spine can be defined as follows. Most of the time the fracture pattern is the result of a combination of two or more forces.
The extent of the fracture depends largely on the energy and speed with which the force is delivered.
- Axial loading
- Flexion
- Lateral compression
- Shear
- Extension
- Flexion distraction
- Flexion rotation
The diagram below depicts the mechanism and the way forces act

via Musculoskeletal key
Axial Loading
- Causes compression
- Bursting of the vertebral body – called a burst fracture
- Causes comminuted fracture as the intervertebral disc is forced into the intervertebral body
- The ligaments remain intact- the comminuted fracture is stable
The posterior column may be involved in severe cases to some extent.
Burst fractures may show some degree of fracture fragment retropulsion into the vertebral canal. Burst fractures can occur with or without posterior ligamentous complex disruption. Unlike fracture dislocations, burst fractures do not demonstrate a translational deformity.
Flexion
Flexion causes anterior compression. a compression of more than 40-50% also causes disruption of posterior structures. These fractures with posterior disruption can lead to instability if not stabilized.
The fractures are rarely associated with neurological deficits except when multiple adjacent vertebral levels are affected. Compression fractures are isolated wedge-type fractures of the anterior and middle aspects of the vertebral body. There is no involvement of the posterior vertebral body [Unlike burst fractures]. Whereas most compression fractures are thought to be stable, more severe injuries may be associated with posterior ligamentous complex disruption.
Lateral Compression
Lateral compression of the spine can occur when the spin is forcefully bent sideways. It usually leads to stable injury unless there is a disruption of posterior structures or associated axial compression.
Shearing
The shearing force pulls one vertebra over the other. This often results in severe ligamentous injury and anterior, posterior, or lateral vertebral displacement. Anterior displacement is the most common and may also lead to severe spinal cord injury.
It results in a displacement of the whole vertebra and an unstable fracture of the articular processes or pedicles.
Holdsworth slice fracture* is an example of shearing force injury [along with rotation].
*Denis in his work has used the term slice for flexion rotation injury through the vertebra. [see below]
Flexion-Distraction injuries
Flexion distraction injury is also known as seat belt injury as the injury was found when lap type of seat belts were in use. The spine flexes with the axis of flexion is anterior to the vertebral column causing failure of the anterior and posterior columns in distraction. This causes the failure of the bone, disc, and ligamentous structures. The injury can be ligamentous or bony and ligamentous.
This injury occurs most commonly at the thoracolumbar junction. Bilateral facet dislocation can occur.
It i an unstable injury and was described by Chance. Hence, it is popularly called Chance fracture too.
These are highly unstable injuries. The unique injury feature is a translational deformity, which can occur in the sagittal and/or coronal planes.
If the center of rotation is near the posterior longitudinal ligament
- Compressive load or force acts on the anterior vertebral body- The anterior column fails in compression
- There is the corresponding distraction of posterior elements- the posterior column fails in distractions pattern of fracture would depend on the center of rotation
Flexion -Rotation
This leads to unstable fracture dislocation injury.
There is usually a complete rupture of the posterior and middle columns under tension and rotation. The anterior column may fail in varying combinations of compression and rotation.
The middle column may fail through the disc or vertebra. A slight amount of rotation between the segment above and the segment below may be seen.
Classification of Thoracolumbar Spine Injury
Over the years many classifications of thoracolumbar spine injuries have been proposed. There is no one accepted system of classification in use. The most commonly used is TLICS or thoracolumbar injury classification and severity score as not only it takes into account fracture pattern but also the cord injury severity.
Denis, based on his study, Denis divided spine injuries into four main types. This was based on the number of columns involved and the mechanism of injury.
- Compression
- Involved anterior column with an intact middle column
- Results from failure of the anterior column in compression
- Can occur by following the mechanism
- Axial loading
- Anterior flexion
- Burst Fracture
- Involves the anterior and middle columns
- The posterior column in severe cases
- caused by axial compression
- Flexion-Distraction injury or Seatbelt Type Injury
- Usually, all three columns involved
- The translation is not associated
- Unstable injuries
- Fracture-Dislocation
- All three columns involved
- Injury can occur due to a combination of shear, rotation, compression, and tension
One of the major drawbacks of Denis classification is that it is mechanistic and does not take into account the status of neural injury. Moreover, the middle column is virtual and not an anatomical structure.
AO Classification
AO based the classification of thoracolumbar spine injuries on that a stable spine can resist three major forces
- Axial compression forces- cause shortening of the column
- Axial distraction forces- cause lengthening of the column
- Torsional forces- cause rotation around the longitudinal axis
Depending on where the center of rotation of the spinal segment different patterns of injury may emerge
- Compression Injury
- Centre of rotation- At the posterior annulus
- Compression or burst fracture
- Anterior column shortening
- Distraction Injury
- Center of rotation posterior to spinous process
- Extension distraction injury
- Lengthening of the anterior column
- Rotational Injury
The injuries are further divided into three subcategories according to increasing severity.
AO classification suffers the same drawbacks of being mechanistic and not taking neural conditions into account.
Thoracolumbar Injury Classification and Severity Score or TLICs
It is based on three major categories
- Morphology of the injury as defined by imaging studies
- Compression injuries – 1
- Burst Fractures – 2
- Translational/rotational injuries -3
- Distraction injuries – 4
- Integrity of the posterior ligamentous complex ON MRI
- Intact – Zero
- Suspected-2
- Definite disruption – 3.
- Neurologic status of the patient.
- Intact – zero
- Nerve root injury- 1
- Complete cord injury -2
- Incomplete cord injury – 3
- Cauda equina syndrome- 4
The total score is calculated by adding points in all the major categories.
- < 3 – Nonoperative
- 4- Either nonoperative or operative treatment
- 5 or more- Surgery
Thus TLICS is able to predict the need for surgical treatment.
Spinal Cord Injury in Thoracolumbar Spine Injuries
Injury to the cord is of two types
- Primary Injury
- The actual injury during the process of trauma
- Contusion or laceration or transection
- The actual injury during the process of trauma
- Secondary Injury
- Due to cellular changes at the injury site
- Ongoing neural compression.
Causes leading to canal compromise/injury
- Bony retropulsion from a burst fracture
- Fracture-dislocations of vertebrae
- Hematoma formation
- Disc herniations
Factors that make the spinal cord vulnerable
- Smaller canal space
- Critical vascular supply
Due to greater vascularity, greater spinal diameter, and lesser vulnerability of cauda equina, injuries in the lumbosacral region may cause marked displacement without neurological deficit.
Incomplete Vs Complete Spinal Cord Injury
Complete spinal cord injury implies complete loss of motor and sensory function below the level of the injury
An incomplete injury means that there is some level of residual motor or sensory function below the level of injury.
ASIA scale is used to know the completeness of injury. It is as follows.
- A – Complete loss of motor and sensory function
- B – Complete loss of motor function but intact or partially intact sensory function
- C – Motor function present below the neurologic level, with greater than half of the muscles power less than 3
- D – Motor function preserved below the neurologic level, with greater than half of the muscles power more than 3
- E – Normal
It is worth mentioning that the completeness of spinal cord injury can only be ascertained after the spinal shock has gone. [A state where there is complete flaccid paralysis below injury as if the spinal cord is in shock. It generally lasts 48 hours]
Return of the bulbocavernosus reflex marks the end of spinal shock.
[Read more about spinal shock]
Complete injury of the spinal cord is evident. Incomplete spinal injury can present in any form but few are common important patterns.
[Read more about incomplete spinal cord injury patterns.]
Presentation
Often there is a history of severe injury [In severely osteoporotic or very old patients, a fracture may occur under normal physiological loads]. The patient would present with
- Pain in the injured region
- Deformity may or may to be obvious
- Neural injury signs – A mix of cord and root lesion may be present depending on the level involved
- Complete loss below L1 in conus medullaris
- Sacral part of cord – bladder bowel involvement. loss of posterior muscles
- Lower lumbar single or multiple root involvement
- Cauda equina syndrome
With the association of other injuries, spine injuries may have significant blood loss.
Anterior inspection can reveal abdominal and/or chest ecchymoses. Posteriorly, any irregularity such as ecchymoses, bogginess, crepitus, open wounds, focal sites of tenderness, malalignment, or areas of palpable step-off should be noted.
A neural examination and ASIA score should be done as per the condition of the patient.
Imaging for Thoracolumbar Spine Injuries
Xrays

Anteroposterior and lateral X-rays are usually obtained if the spine is suspected to have an injury.
The AP view best demonstrates
- Changes in coronal alignment- [indicates high energy injury]
- Changes in interpedicular distance
- Normally increases from cranial to caudal side
- Abnormal widening- lateral displacement of vertebral body fragments, typical of burst fractures.
- Space between spinous processes
- If increased – posterior ligamentous complex disruption.
Translation greater than 2.5 mm in either sagittal or coronal plane suggests gross instability.

The lateral view is more useful in characterizing and detecting injuries and following
- Sagittal plane malalignment
- Vertebral body height loss
- Break in spinous processes


Computed Tomography
CT with sagittal and coronal reconstructions is becoming an increasingly popular method of initial spine screening. Few centers skip X-rays and move to CT directly.
CT provides better visualization of the fracture than X-ray. Fractures of the pedicles, laminae, facets, and transverse processes are best detected and assessed with CT. But CT has limitations in assessing the canal space.

Magnetic Resonance Imaging
MRI provides better visualization of the spinal cord and soft tissues. MRI can help visualize disc herniations, epidural hematomas, or spinal cord edema that would not be detectable by other imaging modalities.
MRI has become an important tool in assessing the integrity of the posterior longitudinal ligament which in turn would dictate the mode of treatment that would follow.
MRI is also indicated where CT and X-rays fail to explain the findings or neural deficit.
Treatment of Thoracolumbar Spine Injuries
Non-Operative Treatment
Nonoperative treatment of thoracolumbar spine injuries consists of bed rest, brace, molded orthosis, or casts. It is estimated that only 20 to 30% of spine fractures require surgery and the rest of them can be treated nonoperatively.
Stable fracture patterns without any neural deficit can be treated non-operatively.
Fractures that can be treated nonoperatively
- Mild Compression fractures
- Isolated lamina fracture,
- Spinous process fractures
- Patient not suitable for surgery
Operative Treatment
Operative treatment offers immediate spinal stability, allowing early sitting by the patient, easy transfer of the patient, and earlier rehabilitation.
Moreover, there is a better restoration of spinal alignment and correction of translational deformities which translates into the restoration of canal dimensions.
Operative treatment includes decompression of the spinal cord/nerve roots, fixation of the injured spine, and fusion of the spine. Posterior open surgery decompression, pedicle screw fixation, and fusion is the most commonly performed surgery for thoracolumbar spine injuries.
The goals of surgical treatment are
- Protection of neural structures {by decompression}
- Prevention of deformity {by reduction and fixatio}
- Prevention of instability {By fusing vertebrae}
Which thoracolumbar fractures require surgery?
- Severe injuries involving two columns
- Flexion-distraction injuries
- Fracture-dislocations
Approach and Instrumentation
The posterior approach is used more commonly. An anterior approach is used when anterior decompression and instrumentation is required;
Pedicle screws are used most commonly as fixation implants. lately, minimally invasive surgeries have gained popularity
For using anterior instrumentation and fixation, often reconstruction of the anterior column with strut grafting, cages, or both is required.
The anterior approach offers direct decompression and preservation of motion but is associated with greater morbidity
Timing of surgery
Studies have shown that surgeries performed within 3 days of thoracolumbar spine injuries show better outcomes.
There is controversy in the literature about the timing of surgery for thoracolumbar spine injuries. There is no conclusive evidence that early surgical decompression and stabilization improves neurological recovery, or that a delay in surgery would cause compromised neurological recovery.
However, it is agreed upon that if the neurological deficit is progressive, an emergency decompression is indicated.

Otherwise, there are two schools of thought. One advocates early decompression and stabilization. The benefits highlighted are a lesser complication rate and a shorter duration of hospital stay. The other school advocates for delay in surgical procedures to allow resolution of cord edema.
Complications of Thoracolumbar Spine Injuries
Injuries to the thoracolumbar spine can lead to a variety of potential complications.
- Neural deficit
- Primary injury
- May worsen during shifting/surgery
- Ileus or decrease in bowel movements
- Nonfunctional bladder
- Deformity – Kyphosis >30 degrees
- Dural Tears
- Associated with vertical lamina and facet fractures
- May suggest nerve root entrapment
- Repair should be attempted
- Bleeding
- Infection
- Implant Failure
- Metal breakage
- Sscrew pullout,
- Subsidence may occur during the postoperative period, leading to at least a partial loss of correction.
- Pneumothorax
- Vessel injury
- erosion into the great vessels following instrumentation, injury to the iliac vessels, ureter, and sympathetic plexus have been reported
- Pseudoarthrosis or failure of fusion of vertebrae
- Can cause chronic pain and worsening deformity.

References
- Denis F. The three-column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983 Nov-Dec. 8 (8):817-31. [Link]
- Thoracolumbar trauma. Browner BD, Jupiter JB, Krettek C, Anderson PA, eds. Skeletal Trauma: Basic Science, Management, and Reconstruction. 6th ed. Philadelphia: Elsevier; 2020. Vol 1: Chap 33.
- Wood KB, Li W, Lebl DR, Ploumis A. Management of thoracolumbar spine fractures. Spine J. 2014 Jan. 14 (1):145-64. [Link]
- Karaikovi? EE, Pacheco HO. Treatment options for thoracolumbar spine fractures. Bosn J Basic Med Sci. 2005 May. 5 (2):20-6. [Link]