Last Updated on October 29, 2023
Thromboprophylaxis stands for prophylactic measures to decrease the risk of venous thromboembolism by measures that promote venous outflow from the legs and drugs that reduce thrombosis.
Venous thromboembolism which encompasses pulmonary embolism and deep vein thrombosis is a major cause of morbidity and mortality in hospitalized patients.
Thromboprophylaxis is the most effective strategy to reduce morbidity and mortality from venous thromboembolism because thromboembolism is often asymptomatic and unrecognized initially.
Risk factors for venous thromboembolism in surgical patients
The risk of venous thromboembolism is determined by patient characteristics and the clinical setting. They include
- Medical illnesses
- Obesity
- Previous history of venous thromboembolism
- Age over 60 years
- Prolonged immobilization
- Lower limb paralysis
- Hormonal therapy like oral contraceptives or hormone replacement therapy
- Stroke
- Congestive heart failure
- Recent myocardial infarction.
- Biochemical abnormalities
- Deficiencies of antithrombin, protein C or protein S
- Activated protein C
- Antiphospholipid antibody syndrome
- Myeloproliferative disorders
- Essential thrombocythemia
- Polycythemia rubra vera
- Paroxysmal nocturnal hemoglobinuria
- Major surgeries
- Orthopedic surgery of the lower limbs
- Hip arthroplasty
- Knee arthroplasty
- Surgery for hip fractures
- Cancer surgery for cancer
- Neurosurgery
- Acute spinal cord injury
- Multiple trauma
- Deep system venous disease.
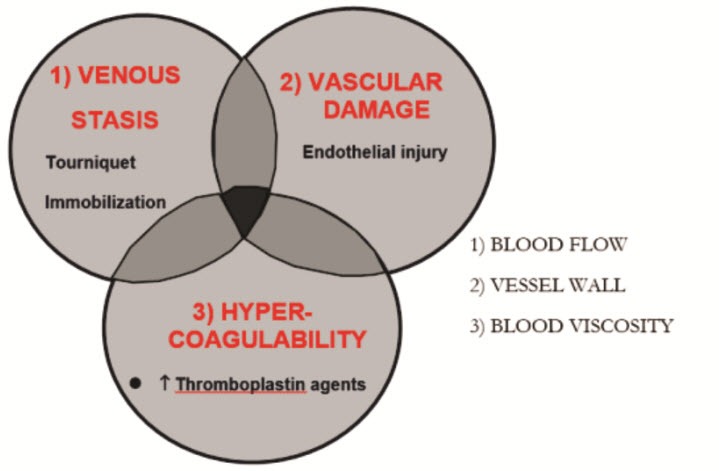
Pathophysiology of venous thrombosis
Venous thrombi usually develop at sites of slow or disturbed blood flow and begin as small deposit of platelets, fibrin, and red cells in valve-cusp pockets or in the intramuscular sinuses of the veins of the lower limb.
As the thrombus grows, it occludes the lumen of the vein, producing venous stasis, and then extends both proximally and distally as a coagulation thrombus composed of red blood cells with interspersed fibrin.
Patients are predisposed to venous thrombosis when fulfilling the elements of Virchow’s triad
- Venous stasis
- Endothelial injury
Venous stasis occurs secondary to long periods of immobilization before or during surgery and limited, or impaired postoperative ambulation.
Endothelial injury can be caused by either direct trauma to the deep tissues or indirectly by hematoma formation and thermal injury (during surgery from cautery or during cement polymerization).
Principle of Thromboprophylaxis
The prophylactic are directed at one or more of these pathogenic factors
- Anticoagulants that counteract blood coagulation
- Drugs that suppress platelet function and the interaction of platelets with the damaged vessel wall
- Mechanical devices that prevent venous stasis.
Oral Anticoagulants
Warfarin Sodium
Oral anticoagulant prophylaxis using warfarin sodium is effective for the prevention of venous thromboembolism in patients undergoing elective hip surgery and in patients who sustain a fracture of the proximal femur.
It causes a reduction in the frequency of both venous thrombosis and pulmonary embolism.
The simplest way to use this medication is to administer 10 mg orally the night before surgery [some prefer to start on the first postoperative day] followed each day by an appropriate dose to maintain an international normalizing ratio between 2 and 3. The use of warfarin sodium can be problematic, however, if there is a surgical delay. Furthermore, the risk of bleeding complications has limited the acceptance of oral anticoagulant prophylaxis.
Unfractionated Heparin or Heparin
Although it is effective in high risk general surgical patients, prophylaxis with low dose subcutaneous heparin is relatively ineffective for preventing venous thromboembolism in orthopedic patients. In patients undergoing surgery for a fractured hip, prophylaxis with low-dose heparin does not appear to reduce the frequency of large thrombi in the popliteal or femoral veins.
Low Molecular Weight Heparin
Low- molecular- weight heparins (LMWHs ) represent a newer pharmacological agent for prophylaxis and treatment of venous thromboembolism. Heparin acts via binding to antithrombin III, a natural inhibitor of the clotting cascade, and heparin-antithrombin III complexes act to inhibit factors Xa and IIa (thrombin).
LMWH can either be given preoperatively or postoperatively.
If it is started preoperatively, needle placement should occur 10 to 12 hours after the last dose of LMWH, with subsequent dosing delayed at least 2 hours after needle placement.
With the postoperative regime, the epidural catheter should be left indwelling overnight and removed the following day. The first dose of LMWH can be administered 2 hours after catheter removal.
Fondaparinux
The interaction of heparin and LMWH with antithrombin is mediated by a unique pentasaccharide sequence found on one-third or one-fifth of the chains of UFH and LMWH.
Fondaparinux is a synthetic analog of this naturally-occurring pentasaccharide sequence which also acts as an anticoagulant by binding antithrombin.
Fondaparinux exhibits excellent bioavailability after subcutaneous injection and is given once daily. But treatment with fondaparinux is costly.
To avoid bleeding complications following approaches are used
Dextran
Dextran is a glucose polymer that was introduced as a volume expander and subsequently evaluated as an antithrombotic agent.
Two types of dextran polymer have been used clinically:
- Dextran 70
- Dextran 40
The antithrombotic properties of dextran have been attributed
- Decreased blood viscosity
- Decreased platelet reactivity with the damaged vessel wall
- Decreased platelet aggregation
- Increased susceptibility to fibrinolysis of the fibrin clots.
The major side effect of dextran is volume overload, which may result in cardiac failure, particularly in elderly patients with limited cardiac reserve.
Antiplatelet drugs
Acetylsalicylic acid or Aspirin
This inhibits platelets by permanently acetylating cyclooxygenase-1, the enzyme involved in the first step in the synthesis of thromboxane A2, a potent platelet agonist. Role of aspirin prophylaxis in patients undergoing hip fracture surgery remains controversial because of the inconsistent findings trials.
Thienopyridines
This group includes ticlopidine and clopidogrel, irreversibly inhibit platelet ADP receptors. Both agents must undergo hepatic transformation to generate metabolites that inhibit these receptors. Consequently, their onset of action is delayed unless loading doses are given.
Clopidogrel is replacing ticlopidine because of safety and convenience advantages. Unlike ticlopidine, clopidogrel is not frequently associated with neutropenia, thrombocytopenia and thrombotic thrombocytopenic purpura.
Physical Methods
- Elastic stockings
- Intermittent pneumatic compression of the
- Plantar venous plexus (foot pumps) for deep vein thromboprophylaxis
Thromboprophylaxis in various clinical settings
LMWH or warfarin should be given for at least 10 days. Patients with risk factors for venous thromboembolism or those who are not mobile should receive prophylaxis with LMWH or warfarin for 30 days.
Arthroplasty
The incidence of venographically-detected deep vein thrombosis is 51% in patients in patients of elective hip arthroplasty and 61% of knee arthroplasty.
LMWH or warfarin are drugs of choice. Low dose unfractionated heparin is not recommended.
Low molecular weight heparin or LMWH is started 12–24 hours after operation and is given once or twice daily thereafter. Warfarin is started the evening after the operation, and the dose is titrated to achieve an INR of 2–3.
Because LMWH produces rapid anticoagulation, the risk of bleeding is higher.
Elastic stockings or intermittent pneumatic compression does not reduce the incidence of proximal DVT in patients who undergo elective hip arthroplasty, although both modalities lower the rate of calf DVT.
Mechanical methods can be combined with low molecular weight heparin or warfarin but are not effective alone.
Fondaparinux also is effective in patients undergoing elective hip arthroplasty but is expensive
In knee arthroplasty too, LMWH and warfarin are the prophylactic agents of choice though both are less effective than elective hip replacement prophylaxis. This primarily reflects their relative inability to reduce the rate of distal DVT in knee surgery patients.
Surgery for hip fracture
Thromboprophylaxis in patients with hip fracture is difficult. Patients are elderly and have multiple medical problems that increase their risk of bleeding.
Surgery is often delayed and prolonged immobilization further predisposes these patients to venous thromboembolism.
At present, however, LMWH or warfarin is most often used for thromboprophylaxis in patients undergoing surgery for hip fracture.
Acute spinal cord injury
Patients with acute spinal cord injury have the highest rate of DVT among all hospital admissions
Spinal cord injury patients remain at risk for thrombosis for at least 3 months, particularly if the injury is complete.
LMWH is the best form of prophylaxis. Thromboprophylaxis should be continued into the rehabilitation phase. LMWH or warfarin can be used for extended prophylaxis.
Intermittent pneumatic compression or elastic stockings may be considered if anticoagulants are contraindicated early after injury.
References
- Geerts W, Heit JA, Clagett GP, Pineo GF, Colwell CW, Anderson FA Jr, et al. Prevention of venous thromboembolism. Chest 2001;119:132S-175S.
- Stratton MA, Anderson FA, Bussey HI, Caprini J, Comerota A, Haines ST, et al. Prevention of venous thromboembolism: adherence to the 1995 American College of Chest Physicians Consensus Guidelines for Surgical Patients. Arch Intern Med 2000;160:334-40. [
- Nurmohamed MT, Rosendaal FR, Buller HR, Dekker E, Hommes DW, Vandenbroucke JP, et al. Low-molecular-weight heparin versus standard heparin in general and orthopedic surgery: a meta-analysis. Lancet 1992;340:152-6.
- Amarigiri SV, Lees TA. Elastic compression stockings for prevention of deep vein thrombosis. Cochrane Database Syst Rev 2000;(3):CD001484.
- Hull R, Raskob G, Pineo G, Rosenbloom D, Evans W, Mallory T, et al. A comparison of subcutaneous low molecular weight heparin with warfarin sodium for prophylaxis against deep vein thrombosis after hip or knee implantation. N Engl J Med 1993;329:1370-6.