Last Updated on November 22, 2023
Leg is the part of the lower limb between knee and ankle. The osseous framework of the leg is composed of two bones –tibia and fibula.
The tibia is a medial and larger of the two bones.
The bone is similar to the radius bone of the upper limb.
Structure of Tibia
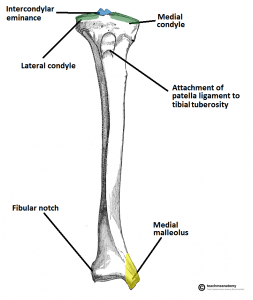

Like all bones, the tibia has an upper end, a shaft, and a lower end.
Upper end
The upper end of the tibia is markedly expanded from side to side, to form two large condyles which overhang beyond the posterior surface of the shaft. The intercondylar area is the area between two condyles. Lower down anteriorly, tibial tuberosity is present.
Medial condyle
Medial condyle is larger than the lateral condyle. Its superior surface articulates with the medial condyle of the femur. The articular surface is oval and its long axis is anteroposterior.
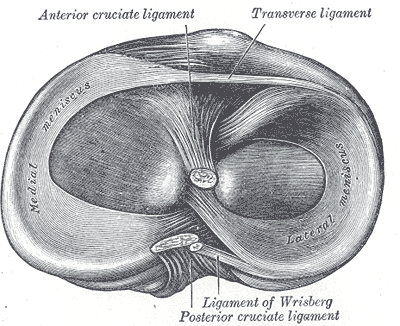
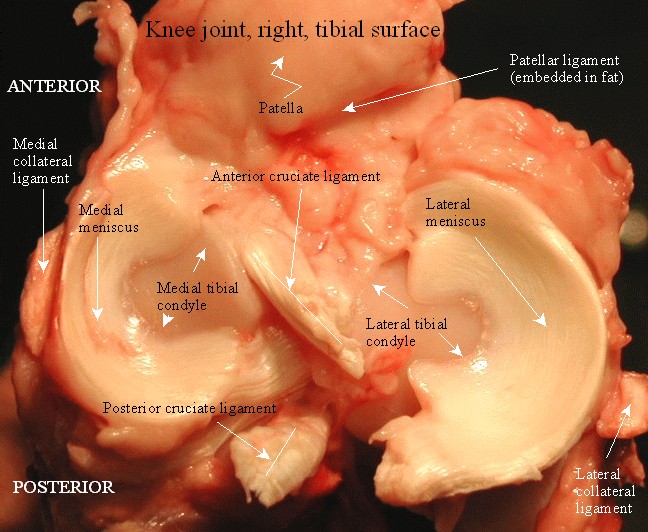
The central part of the articular surface is slightly concave and comes in contact with the femoral condyle. The flatter peripheral part separated from the femoral condyle by the medial meniscus [menisci are discussed in greater detail in knee joint anatomy]. The lateral margin of the articular surface is raised to cover the medial intercondylar tubercle.
On the posterior surface, the medial condyle has a groove. Many vascular foramina mark the anterior and medial surfaces.
Lateral Condyle
The lateral condyle overhangs more than the medial condyle and the articular surface is nearly circular [oval in medial condyle]. It articulates with lateral condyle of femur and in peripheral part is covered by lateral meniscus [similar to medial condyle]. The central part is slightly concave just like medial condyle and comes in contact with femoral condyle.
The articular surface has a raised medial margin which covers the lateral intercondylar tubercle.
The posteroinferior aspect of the lateral condyle bears a flat, circular fibular facet and is directed downwards, backwards and laterally. This facet articulates with the fibula. A groove marks the posterior surface of the condyle superomedial to fibular facet.
The anterior aspect of the condyle bears a flattened impression.
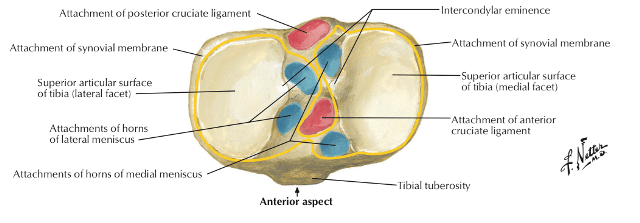
Intercondylar area
The intercondylar area is the roughened area on the superior surface, between the articular surfaces of the two condyles. The area is narrowest in its middle part. This part is elevated to form the intercondylar eminence which is flanked by the medial and lateral intercondylar tubercles.
Tibial Tuberosity
Tibial tuberosity is a prominence located on the anterior aspect of the upper end of the tibia and forms the anterior limit of the intercondylar area.
Lower down, tibial tuberosity is continuous with the anterior border of the shaft. It has an upper smooth area and a lower rough area. The epiphyseal line for the upper end of the tibia passes through the junction of these two parts.
Shaft of Tibia
The tibial shaft is prismoid in shape and has three borders (anterior, medial and interosseus), and three surfaces (lateral, medial and posterior).
Borders
The anterior border is sharp and S-shaped [ convex medially in the upper part and convex laterally in the lower part.] that extends from the tibial tuberosity to the anterior border of the medial malleolus. The anterior border is subcutaneous and forms the shin.
The medial border It extends from the medial condyle, above, to the posterior border of the medial malleolus and is rounded.
The lateral border is also called interosseous border and extends from the lateral condyle [ a little below and in front of the fibular facet] to the anterior border of the fibular notch.
Surfaces
The lateral surface lies between the anterior and interosseus borders. In its upper three fourths it is concave and is directed laterally, and in its lower one fourth it is directed forwards.
The medial surface lies between the anterior and interosseus borders. It is subcutaneous in mostly [ upper three fourths]
Between the medial and interosseus borders is the posterior surface of the tibia. It is widest in its upper part. A rough ridge called the soleal line crosses it here extending from the fibular facet, running downwards and medially, and terminating by joining the medial border at the junction of its upper and middle thirds. [see image]
Above the soleal line, the posterior surface is in the form of a triangular area whereas the area below the soleal line is elongated and divided into medial and lateral parts by a vertical ridge which harbors a downward directed nutrient foramen.
The nutrient foramen transmits the nutrient artery which is a branch of the posterior tibial artery.
Lower End
The lower end of the tibia is also expanded but lesser than the upper end. It has a downward projection on the medial side called medial malleolus.
It has five surfaces –
The anterior surface of the lower end has an upper smooth part and a lower rough and grooved part.


The medial surface is subcutaneous and is continuous with the medial surface of the medial malleolus. The medial malleolus is a short but strong process which projects downwards from the medial surface of the lower end of the tibia. It forms a subcutaneous prominence on the medial side of the ankle and serves as an important anatomical landmark.
The lateral aspect of the lower end presents a triangular fibular notch to which the lower end of the fibula is attached. The upper part of the notch is rough. The lower part is smooth and may be covered with hyaline cartilage.
The inferior surface of the lower end is articular. It articulates with the superior trochlear surface of the talus and thus takes part in forming the ankle joint. Medially the articular surface extends on to the medial malleolus.
The posterior surface is traversed by a shallow groove directed obliquely downward and medialward, serving for the passage of the tendon of the flexor hallucis longus.
Attachments on the Tibia


Upper-End Tibia
Medial condyle
- The upper border – capsular ligament of the knee joint and deeper fibers of the tibial collateral ligament
- Groove on the posterior surface – Semimembranous
- Anterior surface – the medial patellar retinaculum
Lateral Condyle
- The iliotibial tract – flattened impression on the anterior surface.
- The capsular ligament of the superior tibiofibular ligament – margins of the fibular facet.
- The origins of fibers of the extensor digitorum longus and of the peroneus longus (near the fibular facet.)
- The groove on the posterior surface of the lateral condyle is occupied by the tendon of the popliteus (with an intervening bursa)
Intercondylar Area
From before backwards [See the image above]
- The anterior horn of the medial meniscus, just in front of the medial articular surface.
- The anterior cruciate ligament on a smooth area just behind the previous attachment.
- The anterior horn of the lateral meniscus, to the front of the intercondylar eminence, and lateral to the anterior cruciate ligament.
- The posterior horn of the lateral meniscus, to the posterior slope of the intercondylar eminence.
- The posterior horn of the medial meniscus, to the depression behind the base of the medial intercondylar tubercle.
- The posterior cruciate ligament, to the posteriormost smooth area.
Tibial Tuberosity
- The ligmentum patellae or patellar ligament- upper smooth part of the tibial tuberosity.
- Infrapatellar bursa separates the lower rough area of the tuberosity from the skin.
Shaft
- Upper two thirds (or less) of the lateral surface – tibialis anterior origin
- The upper part of the medial surface
- Insertions of the Sartorius, the gracilis and the semitendinosus (from before backwards)
- Posterior to this along with the medial border – tibial collateral ligament.
- Soleal line –
- The soleus muscle [ The tendinous arch for the origin of the soleus is attached to a tubercle at the upper end of the soleal line.]
- Fascia covering the soleus
- Fascia covering the popliteus
- Transverse fascial septum.
- The popliteus is inserted on the posterior surface, into the triangular area above the soleal line.
- The medial area (of the posterior surface) below the soleal line gives origin to the flexor digitorum longus while the lateral area gives origin to the tibialis posterior.
- The anterior border of the tibia
- Deep fascia of the leg and
- Superior extensor retinaculum [in lower part]
- The interosseus border- interosseus membrane.
- Fibular notch gives – interosseus tibiofibular ligament.
- Margins of the articular surface – The capsular ligament of the ankle joint
- Lower border of the medial malleolus – deltoid ligament of the ankle
Important Anatomical Relations of the Tibia
- The lower part of the anterior surface of the shaft and the anterior aspect of the lower end are crossed (from medial to lateral side) by the tibialis anterior, the extensor hallucis longus, the anterior tibial artery, the deep peroneal nerve, the extensor digitorum longus, and the peroneus tertius.
- The lowermost part of the posterior surface of the shaft and the posterior aspect of the lower end are related (from medial to lateral side) to the tibialis posterior, the flexor digitorum longus, the posterior tibial artery, the tibial nerve, and the flexor hallucis longus. The groove for the tibialis posterior tendon continues downwards on the posterior surface of the medial malleolus.
- The lower one-third of the medial surface of the shaft is crossed by the great saphenous vein.
Blood supply of Tibia
The nutrient artery originates from the posterior tibial artery which enters the bone though nutrient foramina on its posterior surface. It is the largest nutrient artery in the body.
Ossification of Tibia
The tibia ossifies from one primary and two secondary centers.
- Primary center appears in the shaft during the 7th week of intrauterine life.
- Secondary center for the upper end appears just before birth and fuses with the shaft at 16-18 years.
- Secondary center for the lower end
- Appears during the first year
- Forms the medial malleolus by the 7th year
- Fuses with the shaft by 15-17 years.
Sometimes, separate secondary centers may appear for the tibial tuberosity and the medial malleolus.
Applied Anatomy
The bone is commonly fractured in trauma especially at the junction of the upper two thirds and the lower one-third of the shafts the shaft is most slender here
Side determination
- The upper end is much larger than the lower end.
- The medial malleolus is on the medial side.
- S-shaped sharp border lies anteriorly.