Last Updated on October 29, 2023
Tibial plateau fractures signify periarticular fractures of the proximal tibia frequently associated with soft tissue injuries. These fractures, being in load-bearing area affect knee alignment, stability, and motion.
Appropriate treatment of these fractures is critical to minimize disability and reducing the risk of complications like posttraumatic arthritis.
Most of these injuries are the motor vehicle–related injuries, and sports-related injuries.

Tibial plateau fractures may be either low-energy or high-energy. Low-energy fractures occur in osteoporotic bone and typically are depressed fractures. High-energy fractures are often a result of motor vehicle–related trauma, and the most common pattern of fracture in this group is a splitting fracture.
Tibial plateau fractures in younger patients are commonly the result of high-energy injuries
These fractures have bimodal distribution. The peak is seen in males in 40s (high-energy trauma) and the females in 70s (falls).
Lateral condyle is most commonly injured. Next common pattern is bicondylar fracture followed by medial condyle.
varus/valgus load with or without axial load is the main mechanism to cause these fractures.
These injuries are commonly associated with meniscal tears, cruciate ligament injuries [esp anterior], compartment syndrome and vascular injuries.
Lateral meniscal tear is more common and is associated with Schatzker II fracture pattern. Medial meniscal tear is most commonly associated with Schatzker IV fractures
Anatomy of Tibial Plateau and Knee
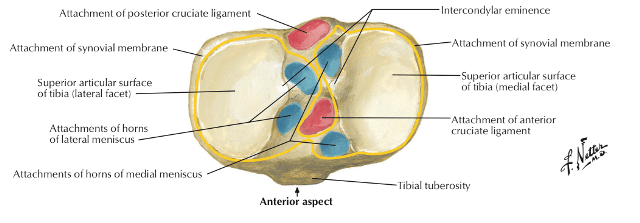
The tibial plateau top most articular portion of the tibia. It is composed of two parts
- Concave articular surfaces of tibial condyles (medial and lateral tibial plateaus)
- Oval-shaped medial
- Circlular lateral tibial condyles
- Medial tibial plateau is larger, stronger and transmits more weight
- Central non-articular intercondylar area
- A site of attachment of menisci and cruciate ligaments
The tibial plateau articulates via the medial and lateral menisci with the medial and femoral condyles to form the tibiofemoral part of the knee joint.
On plane x-ray the tibial plateau slopes posteroinferiorly 10-15 degrees [This may render anterior tibial plateau fractures occult on AP x-ray]
The lateral tibial plateau is convex in shape and is slightly proximal to the medial plateau which is concave in shape and slightly distal in comparison to the lateral tibial plateau
The knee is exposed to forces that can exceed five times the weight of the body. This complex joint has enhanced mobility at the cost of stability
The normal knee is in physiologic valgus alignment. Most of the load transmitted across the knee is medial to the eminence, and therefore, the knee has a stronger cancellous bone.
Anterior compartment musculature attaches to the anterolateral tibia and pes anserine attaches to the anteromedial tibia
Classification of Tibial Plateau Fractures [Schatzker et al]

Type I
- A wedge or split fracture of the lateral aspect of the plateau, usually as a result of valgus and axial forces
- Often the wedge fragment is not compressed (depressed), because the underlying cancellous bone is strong
- Usually seen in younger patients
Type II
- This is a lateral wedge or split fracture associated with compression
- The mechanism of injury is similar to that of a type I fracture, but the underlying bone may be osteoporotic and unable to resist depression, or the force may have been greater
Type III
- Pure compression fracture of the lateral plateau
- Axial force
- The depression is usually located laterally or centrally, but it may involve any portion of the articular surface
Type IV
- Involves the medial plateau
- Varus or axial compression forces
- the pattern may be either split alone or split with compression
- Fracture involves the larger and stronger medial plateau, the forces causing this type are generally greater than those associated with types I, II, or III
Type V
- Split elements of both the medial and the lateral condyles
- May include medial or lateral articular compression
- Usually result of a pure axial force occurring while the knee is in extension
Type VI
- Complex, bicondylar fracture in which the condylar components separate from the diaphysis
- Depression and impaction of fracture fragments
- High-energy trauma and diverse combinations of forces
Clinical Presentation
Tibial plateau fractures are often caused by high-energy trauma in young patients and due to low-energy falls in the elderly.
The soft tissue injury is often substantial, especially in high injury fractures. The patient should be specifically examined for open injury, compartment syndrome, and neurovascular examination.
The literature recommends valgus/varus stress testing but that is too painful and if required should be done under anesthesia.
There could be an associated injury to menisci and/or collateral ligaments necessitating their repair.
The medial collateral ligament is at greater risk than the lateral collateral ligament.
Imaging
X-rays
Most tibial plateau fractures are easy to identify on standard anteroposterior (AP) and lateral projections of the knee. The views should be proper for an accurate diagnosis.
Oblique projections should be added if a nondisplaced tibial plateau fracture is suspected but not seen on the standard projections.
An AP projection of the knee, angled 15° caudally (tibial plateau view), can provide a more accurate assessment of the depth of plateau surface depression.
Traction radiographs if needed may be done to understand fracture alignment, bone loss areas and for surgical planning.
Corresponding views of the uninjured knee for comparison may be done.
When the fracture is suspected and not clearly visible, the following findings may indicate a fracture.
The following subtle radiologic signs may indicate the presence of an underlying plateau fracture:
- Lipohemarthrosis – The presence of a fat/fluid level in the suprapatellar recess on the lateral views of the knee [Due to the entry of fat-laden marrow in the joint]
- Increased trabecular density beneath the lateral plateau on an AP
- Nonalignment of the femoral condyles and tibia on the AP view
CT
CT can catch a subtle fracture and provides more detailed info on complex fractures. It provides better information on the fragments, their orientation and by 3D reconstruction, helps to plan for surgery in detail.
MRI
MRI is an accurate tool for assessing meniscal, collateral and cruciate ligamentous injury, as well as for identifying occult fractures of the tibial plateau. However, its role is not clearly established.
Treatment of Tibial Plateau Fractures
Emergency Care
Undisplaced fractures require immobilization and watch for skin changes if soft tissue injury is severe.
Open fractures and fractures associated with neurovascular deficit need urgent surgery.
Closed displaced fractures are generally high energy, especially in young patients and must be cared for soft tissue swelling and compartment syndrome.
The patient is put on rest and immobilization. In severe joint swelling, aspiration of the joint can be done.
Even if the swelling is not present initially, it could develop in next 24-48 hours.
Blister formation may occur in tense swellings.
Patients who are at high risk for swelling may be put on traction than simple immobilization as soft tissue changes can be better monitored.
Blisters if present may be pierced and a sterile dressing is done.
Fasciotomy is done if compartment syndrome develops.
Sometimes, the skin changes take a longer time [2weeks or more] to heal enough to allow surgery. In such cases, a spanning external fixator to maintain alignment should be used. Articular fragments can be fixed at the same time to reconstruct the joint with screws/K-wires. Definitive fixation can be done at a later date.
Definitive Treatment
The ultimate goals of tibial plateau fracture treatment are to reestablish joint stability, alignment, and articular congruity. Preservation of motion, painless knee function and prevention of post-traumatic arthritis are other goals.
Displaced fracture, where feasible should be considered for surgery.
Fracture displacement ranging from 4-10 mm can be treated nonoperatively. But, a depressed fragment greater than 5 mm should be elevated and grafted.
Nonoperative Treatment of Tibial Fractures
Indications
- Nondisplaced stable split fractures
- Minimally displaced or depressed fractures
- Submeniscal rim fractures
- Fractures in elderly, low-demand, or osteoporotic patients
Treatment
- Initial immobilization followed bt hinged knee brace.
- Immediate passive motion allowed after hinge brace
- Partial weight bearing for 8-12 weeks, and immediate passive range of motion
- Minimally displaced split or depressed fractures
- Low energy fracture stable to varus/valgus alignment
- Nonambulatory patients or those with lower demands
Surgical Treatment of Tibial Plateau Fractures
Indications for surgery
- Open fractures
- Associated compartment syndrome
- A vascular injury
- Displaced bicondylar fractures
- Displaced medial condylar fractures
- Lateral plateau fractures with unstable joint
Surgical Options
The surgery can be done openly or arthroscopically. Open surgeries can be done in a staged manner if required.
Compromised soft tissues may cause the definitive fixation to be delayed. The external fixation may be used in the intervening period.
Various options for internal fixation are
- Arthroscopic-assisted fixation
- Conventional Plating – Non locked buttress plating
- Locked plates specially designed for these fractures
- Biologic fixation with screws or specialized plates like minimally invasive plate osteosynthesis, the least invasive stabilization system
External fixation can be
- Ilizarov fixator
- Hybrid fixator
- Tubular fixator [often temporary]
Combination of devices may also be considered.
Non-weight bearing precautions generally continue for 12 weeks. Active flexion and passive extension are encouraged for 6 weeks, after which period active knee extension is started.
Various Surgical Treatments
Temporary Bridging External Fixator
- Done when definitive fixation cannot be done immediately
- Significant soft tissue injury
- Polytrauma
- Technique
- Two 5-mm half-pins in the distal femur, two in the distal tibia
- Axial traction applied to the fixator
- Assembly locked in slight flexion
- Allows soft tissue swelling to decrease while maintaining alignment
- Decreases the rate of infection and wound healing complications
Arthroscopic-assisted Elevation and Screw fixation
- Types I, II, III, and IV fractures with ligamentous and meniscal injuries
- Minimal soft-tissue injury and allows joint lavage
- Not useful in high-energy fractures
External Fixation with Limited Open/percutaneous Fixation of Articular Segment
- Severe open fracture with marked contamination
- Internal fixation not feasible due to comminution
- technique
- Closed or limited open fracture reduction
- Stabilization of reduction with lag screws or wires
- Add external fixator or hybrid ring fixation
- Permits early knee range of motion
- Pin site problems
- Outcome similar to open reduction, internal fixation
Open Reduction and Internal Fixation
- Preferred mode of treatment wherever applicable
- Indications
- Articular stepoff > 3mm
- Condylar widening > 5mm
- Varus/valgus instability
- All medial plateau fractures
- All bicondylar fractures
- Approaches
- Lateral incision
- Midline incision
- Posteromedial incision
- Dual surgical incisions [for double plate fixation in bicondylar fractures]
- Posterior [For posterior shearing fractures]
- Technique
- Direct or indirect reduction
- Lift the compressed fragment, if present
- Bone graft or substitutes to fill the metaphyseal void caused
- Stable internal fixation with a suitable implant
- Allows an early range of motion exercises
Type-specific Treatment of Tibial Plateau Fractures
Type I
- Ascertain status of the lateral meniscus and the fracture by MRI or arthroscopy.
- Meniscus is torn
- open reduction with internal fixation with the meniscal repair.
- Meniscus intact
- Closed reduction and percutaneous cannulated cancellous screw fixation
- Open reduction is used if closed reduction not successful
Type II, III
- The depressed fragment must be elevated and supplemented with a bone graft.
- Preservation and repair of the lateral meniscus
- Minimal comminution of the lateral condyle
- Cancellous screws with washers suffice
- comminuted fracture in the soft osteoporotic bone
- Buttress plate
Type IV
- Elevate, reduce, and fix by a buttress plate
- Repair meniscus and the other soft tissues
- Fix intercondylar eminence if avulsed with cruciate ligament
- An additional posteromedial incision may be necessary in case of posterior fragment
Types V and VI
- The plateau with more severe injury is plated first.
- Minimal, biologic fixation using percutaneous implants, limited posteromedial incisions on the other side.
- External fixation preferred due to frequent wound problems with internal fixation.
Complications of Tibial Plateau Fractures
Early
- Compartment syndrome
- Vascular injuries
- Swelling and wound-healing problems
- Infections
- Deep vein thrombosis
- Nerve injuries
Late
- Knee stiffness
- Knee instability
- Angular deformities
- Late collapse
- Post-traumatic arthritis
- Higher risk with meniscectomy, axial malalignment, intra-articular infection, and joint instability
References
- Weaver MJ, Harris MB, Strom AC, Smith RM, Lhowe D, Zurakowski D, et al. Fracture pattern and fixation type related to loss of reduction in bicondylar tibial plateau fractures. Injury. 2012 Jun. 43 (6):864-9.
- · Lubowitz JH, Elson WS, Guttmann D. Part I: Arthroscopic management of tibial plateau fractures. Arthroscopy. 2004 Dec. 20(10):1063-70.
- Lubowitz JH, Elson WS, Guttmann D. Part II: arthroscopic treatment of tibial plateau fractures: intercondylar eminence avulsion fractures. Arthroscopy. 2005 Jan. 21(1):86-92. .
- Chen XZ, Liu CG, Chen Y, Wang LQ, Zhu QZ, Lin P. Arthroscopy-assisted surgery for tibial plateau fractures. Arthroscopy. 2015 Jan. 31 (1):143-53. .
- · Yoon RS, Liporace FA, Egol KA. Definitive fixation of tibial plateau fractures. Orthop Clin North Am. 2015 Jul. 46 (3):363-75, x.
- Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, et al. Complications after tibia plateau fracture surgery. Injury. 2006 Jun. 37(6):475-84.
- Mehin R, O’Brien P, Broekhuyse H, Blachut P, Guy P. Endstage arthritis following tibia plateau fractures: average 10-year follow up. Can J Surg. 2012 Feb 1. 55(1):003111-3111.