Last Updated on November 22, 2023
This article mainly focuses on the adult trigger finger, for pediatric condition go to Pediatric Trigger Thumb
Trigger finger is a common problem causing hand pain and disability. Trigger finger is due to abnormal gliding of thickened tendon at the distal aspect of palm within tendon sheath. This thickened tendon gets caught at the edge of the first annular (A1) pulley. [See anatomy below]
The cause of trigger finger is not known. It affects dominant hand more than nondominant. Thumb is the most common digit to be affected followed by the ring, long, little, and index fingers. Multiple fingers may be involved in the same person.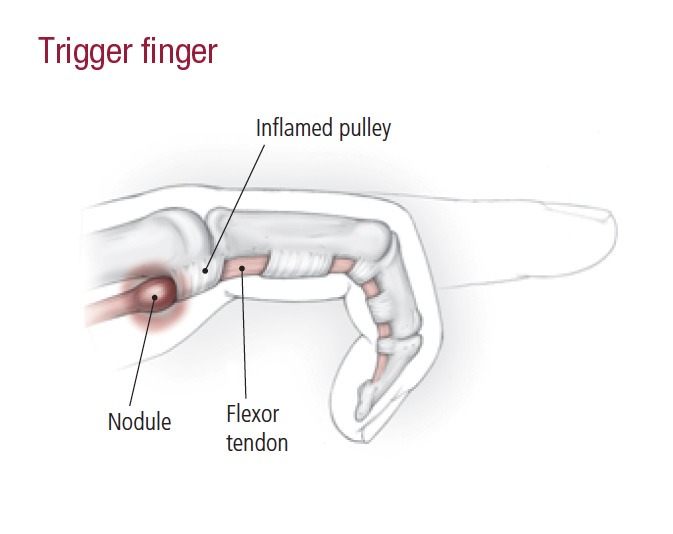
The condition has two profiles – pediatric and adult. The pediatric condition is also known as congenital trigger thumb through the presentation is sometime after infancy. Pediatric trigger finger is much less common than adults and develops almost exclusively in the thumb and thus better named as pediatric trigger thumb.
Read more on pediatric trigger thumb
Trigger finger affects men about six times more commonly than women.
The age of presentation is fifth and sixth decades of life.
Relevant Anatomy
Read Detailed anatomy of hand.
Tendons are enclosed in sheaths called tendon sheaths. Flexor tendons within their sheath run from the level of the metacarpal heads [Approximately at distal palmar crease] to the distal phalanges.
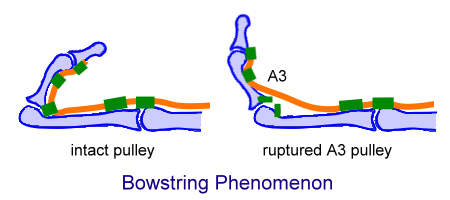
At various places, tendons are attached to the underlying bones and volar plates, by means of pulleys to prevent bowstringing. The phenomenon is explained by the images below.

The pulleys are of two types
Annular [A] – These are composed of single fibrous bands. Thus these are ring-like structures
Cruciate [C] – Cruciate pulleys consist of crossing fibrous bands.
From proximal to distal, the pulleys are named as follows [See the diagram for details]
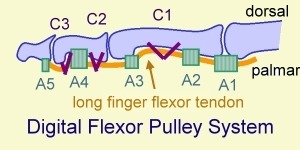
- A1 – over metacarpophalangeal joints. It is the pulley where triggering phenomenon occurs.
- A2 – over proximal end of the proximal phalanx
- C1 – over the middle of the proximal phalanx
- A3 – over the proximal interphalangeal (PIP) joint
- C2 – over the proximal end of the middle phalanx
- A4 – over the middle of the middle phalanx
- C3 – over the distal end of the middle phalanx
- A5 – over the proximal end of the distal phalanx
Thumb
The flexor pollicis longus tendon is a single tendon within the flexor sheath that inserts onto the base of the distal phalanx.
Pulley system of thumb is as follows
There are three pulleys in the thumb, two annular and one oblique.
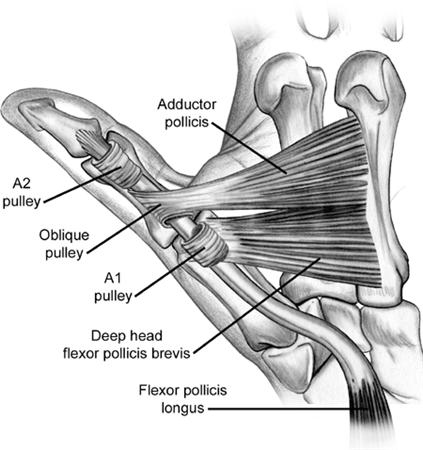
Oblique pulley
Oblique pulley originates at proximal half of proximal phalanx is about 10 mm in length, and blends with a portion of the adductor pollicis insertion.
It is most important pulley in thumb which facilitates full excursion of flexor pollicis longus and prevents bowstringing of flexor pollicis longus.
There are two annular pulleys
A1 pulley is at the level of the volar plate at the metacarpophalangeal joint and is about 6mm in length.
A2 pulley has a minimum contribution to the arc of motion of thumb.
Pathophysiology of trigger finger
The swelling in the flexor tendon cause the obstruction at the proximal pulley mechanism because of size mismatch between the swelling/nodule and space beneath the pulley.
Initially, there is a localized swelling in the tendon leading to increased friction. A nodule may develop on the tendon, causing the tendon to get stuck at the proximal edge of the A1 pulley when the patient extends the digit/
The nodule can get inflamed, further worsening the symptoms.
When more forceful attempts are made to extend the digit, the digit snaps open with significant pain at the distal palm and affected digit. When the nodule is proximal to the pulley, the extension is difficult. If the nodule is restricted distal to the A1 pulley, resulting in difficulty flexing the digit.
Causes of Trigger Finger
The cause of trigger is not clearly understood. Both, nodule formation in tendon and morphologic changes in the pulley may cause triggering but why of these causes is not exactly known.
Certain conditions such as diabetes or rheumatoid arthritis may predispose an individual to trigger finger.
Morphological changes in the pulley and/or the tendon sheath to cause triggering. Following conditions are also known to be associated
- Psoriatic arthritis
- Amyloidosis
- Hypothyroidism
- Sarcoidosis
- Pigmented villonodular synovitis
- Tuberculosis
Trigger thumb particularly is also associated with osteoarthritis of the hand. Other conditions like inflammatory arthritis, gout, or chronic infection can also be associated with trigger thumb.
Multiple digit involvement is common in conditions diabetes mellitus or rheumatoid arthritis.
Clinical presentation
The patients are usually in 5th or 6th decade of life. Locking or catching during active flexion-extension activity with triggering is the commonest complaint. The complaints may vary though like stiff finger or pain over the distal palm or radiating along the finger.
In cases who seek advice very late, flexion deformities could be the presentation.
Some patients report swelling of the affected digit at the base.
On examination, tenderness over the A1 pulley or a palpable nodule in the line of the flexor digitorum superficialis, just distal to the metacarpophalangeal joint in the palm may be felt.
With a trigger thumb, the tenderness to palpation is found at the palmar aspect of the first metacarpophalangeal joints rather than over the distal palmar crease.
Triggering phenomenon may be noted in other digits too.
The patient should be assessed for the presence of other associated conditions.
Some patient may give a history of occupational repetitive injury.
Children with trigger thumb rarely complain of pain. They are usually brought in for evaluation when aged 1-4 years with a complaint of flexed posture of interphalangeal joint of the thumb, often unilateral but sometimes bilateral.
Differential Diagnoses
The following can mimic the locking of trigger finger
- Catching of collateral ligaments of the metacarpophalangeal on metacarpal head
- Abnormal sesamoids
- Loose body in the MCP joint
- Localized swelling in the flexor digitorum profundus gets entrapped at the decussation of the flexor digitorum superficialis
- A partially lacerated flexor tendon catches against the A1 pulley or the flexor digitorum superficialis
Other conditions which form differential diagnoses are
- Infectious tenosynovitis
- Carpal Tunnel Syndrome
- Dupuytren Contracture
Lab Studies
No lab tests are needed in the diagnosis of trigger finger. Investigations may be needed for associated conditions like diabetes mellitus or rheumatoid arthritis.
CBC, glycosylated hemoglobin (HbA1c), fasting blood sugar, or rheumatoid factor could be done as required.
Imaging
Xrays are normal in trigger finger. But they are helpful in determine bony abnormalities like osteophytes, abnormal sesamoids, loose bodies etc.
Radiographs are helpful to exclude osteoarthritis, fracture malunion, foreign body, or a large sesamoid bone that is affecting interphalangeal joint motion.
Classification
The various grades are defined as follows
Grade I [Pretriggering]
There is a complaint of pain and history of catching. Catching may not be always present and may not be demonstrable on clinical examination. There is tenderness over the A1 pulley
Grade II [Active]
Catching can be demonstrated on clinical examination but the patient is able to extend the digit actively.
Grade III [passive]
IIIa – Demonstrable locking in which passive extension is required
IIIb – Inability to actively flex the finger
Grade IV [contracture]
There is a demonstrable catching, with a fixed flexion contracture of the proximal interphalangeal joint
Treatment of Trigger Finger
Following treatment options are available for trigger finger
- Medications
- Orthoses
- Corticosteroid injections
- Surgery
Injection therapy is now considered to be the first line of management. Failure of injection treatment or the presence of other pathologies such as rheumatoid arthritis may call for surgery.
The pediatric thumb is usually treated by surgical release.
Nonoperative Treatment of Trigger Finger
Most trigger digits in adults can be managed successfully with local steroid injections and splinting.
Injection Therapy for Trigger Thumb
Corticosteroid injection in the area of tendon sheath thickening is considered to be the first-line treatment of choice for trigger finger. A repeat injection may be needed.
Though splinting and local corticosteroid injection can be done in pregnancy but surgery is usually deferred until after delivery.
Following situations offer a better outcome
- Female patients
- Single finger affected
- Duration of symptoms < 4 months
- No associated conditions [rheumatoid arthritis or diabetes mellitus]
- Discrete, palpable nodule.
Patients with rheumatoid arthritis or diabetes mellitus are relatively resistant to injection treatment.
Triamcinolone is the most common drug used for injection and it is mixed with an anesthetic agent for the application.
If there is a palpable nodule, the injection is given in the nodule itself.
Otherwise, the injection can be given in the tendon sheath.
After the injection, the patient is actively encouraged to move the finger.
Ultrasonographically guided steroid injection may maximize the injection’s accuracy.
Splinting is not used routinely for these cases.
A second corticosteroid injection may be performed 3-4 weeks after the first one.
If 2-3 injections fail to provide adequate resolution, the patient might require surgery.
Corticosteroid injections are generally not helpful in these cases of pediatric trigger thumb.
Splinting
Custom-made splinting of the metacarpophalangeal joint is another option and may be chosen in who do not wish to undergo a steroid injection or as an adjunct to injection.
Surgical release
The chief indications for surgical management of trigger finger are as follows:
- Failure of non-operative treatment
- Irreducibly locked digit
- Trigger thumb in infants
The surgery involves release of A1 pulley which can be done percutaneous or through an open incision.
However, the open technique is absolutely essential for the thumb or little finger or in the presence contracture of proximal interphalangeal joint.
Complications
Potential complications of corticosteroid injection include the following:
- Infection
- Bleeding
- Weakening of the tendon
- Fat atrophy at the injection site
Potential Complications after Surgical release
- Tenderness over the incision site
- Adhesions
- Stiffness following adhesions
- Digital nerve injury
- Bowstringing due to accidental A2 cut
- Recurrence
- Infection
Prognosis
The prognosis in trigger finger is very good; most patients respond to corticosteroid injection with or without associated splinting. Some cases of TF may resolve spontaneously and then recur without obvious correlation with the treatment or exacerbating factors.
Digits with a discrete, palpable nodule had a 93% success rate with a single injection.
A failure rate of 52% has been noted in patients with the diffuse pattern.
Patients with diabetes have an overall success rate of 50% for a steroid injection.
Patients who need surgical release generally have a very good outcome with success rates of 74-94 %.
The prognosis is also very good for congenital trigger thumb that is treated with resection of the tendon nodule.
References
- Strakowski JA, Wiand JW, Johnson EW. Upper limb musculoskeletal pain syndromes. Braddom RL, ed. Physical Medicine and Rehabilitation. Philadelphia, Pa: WB Saunders; 1996. 756-82.
- Bae DS. Pediatric trigger thumb. J Hand Surg Am. 2008 Sep. 33(7):1189-91.
- Masquijo JJ, Ferreyra A, Lanfranchi L, Torres-Gomez A, Allende V. Percutaneous Trigger Thumb Release in Children: Neither Effective Nor Safe: A Cross-over Controlled Trial. J Pediatr Orthop. 2013 Dec 6.
- Schubert C, Hui-Chou HG, See AP, Deune EG. Corticosteroid injection therapy for trigger finger or thumb: a retrospective review of 577 digits. Hand (N Y). 2013 Dec. 8(4):439-44.