Last Updated on December 12, 2020
Tuberculosis of spine or TB spine or spinal TB was first described by Percivall Pott, after whom it is also referred to as Pott’s disease or Pott’s spine.
Tuberculosis of spine is the commonest form of skeletal tuberculosis. It constitutes about 50 percent of all cases of bone and joint TB.
There are few other names by which spinal tuberculosis is known and it is important to know because the terms are interchangibly used and confusion might be avoided when the term is known. These are
- Vertebral tuberculosis
- Spinal Koch’s [Tuberculsosis is also called Koch’s lesion]
- Caries spine or spinal caries
- Tuberculous spondylitis.
Tuberculosis of spine is most commonly found in the first three decades of life but can occur in any age group.
There is no gender predilection.
The lower thoracic region is the most common region to be affected by this condition. It is followed by lumbar, upper dorsal, cervical, and sacral regions in decreasing order of frequency.
Anatomy of Spine
This section will cover an overview of the spine anatomy. Detailed anatomy of the spine is discussed separately. Here is a list of articles on spine anatomy
Human spine or vertebral column is a structure made of multiple small units called vertebra and extends from just below the base of skull to a point just below the beginning of gluteal cleft.
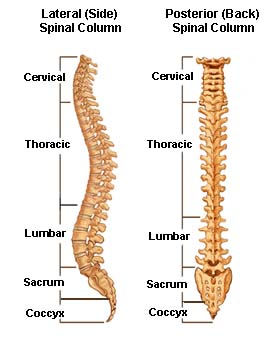 Spine is divided into five regions
Spine is divided into five regions
Cervical Spine
This part of the spine is present in the neck and consists of first seven vertebrae. The cervical spine has a normal lordotic curve [Anterior convex, posterior concave]
Thoracic Spine
Also called dorsal spine, it is below the cervical spine and spans upper trunk or thorax or area corresponding to the chest. It contains a total of 12 vertebrae which are designated as T1 to T12
Thoracic spine has a normal kyphotic curve [Anterior concave, posterior convex]
Lumbar Spine
It follows the thoracic spine and consists of 5 vertebrae, L1 to L5. Anatomical variations in which 4 or 6 vertebrae might be present in the lumbar spine are known.
Sacral Spine
The sacral spine is composed of five sacral vertebrae S1 to S5. Vertebrae in the sacral spine are fused to each other. This part of the spine follows lumbar spine and is present in the pelvic area.
Coccyx or Coccygeal Spine: This is also known as tailbone. It consists of four fused vertebrae (the coccygeal vertebrae) below the sacrum.
Vertebrae are the structural units of the spine are stacked together to form the entire vertebral column. Discs are cushion-like structures acting as shock absorbers between two vertebrae.
They also permit some movement between the vertebral bodies and the transmission of weight.
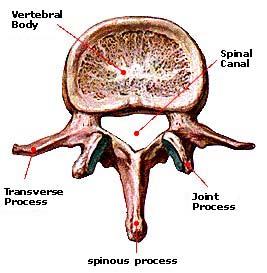
Each vertebra consists of an anterior body that is attached to a posterior ring called a posterior neural arch [pedicle and laminae together].
Pedicles, laminae and posterior surface of the body forms boundaries of the spinal canal, which is the space for the passage of the spinal canal.
This spinal canal is the space where the spinal cord passes. There is a transverse process on either side of the arch which serves as an attachment to various muscles and ligaments. Posteriorly is the posterior spinous process that also serves as an attachment to the ligaments and muscles of the spine.
The neural foramen is the opening where the nerve roots exit the spine and travel to the rest of the body. There are two neural foramina located between each pair of vertebrae, one on each side.
Various muscles and ligaments attach to the spine. They help the spine to stabilize and allow it to carry various movements.
Pathophysiology of Tuberculosis of Spine
The infection in the spine occurs from the blood mainly [hematogenous infection]. The bacteriae reach the site of infection via the bloodstream. The focus of infection usually begins in the cancellous bone of the vertebral body.
Sometimes, the infection can start in the posterior neural arch, transverse process, or subperiosteally deep to the anterior longitudinal ligament in front of the vertebral body.
[Posterior element reportedly account for about 5% of the tubercular infections of spine]
As the disease progresses, the area of infection gradually enlarges and spreads to involve two or more adjacent vertebrae by extension beneath the anterior longitudinal ligament or directly across the intervertebral disc.
Sometimes, multiple vertebrae may be infected which are separated by normal vertebrae. Such infections are called skip lesions. For example, an infection may be disseminating to distant vertebrae via the paravertebral abscess can lead to skip lesions.
As the tuberculosis of spine progresses, vertebral bodies lose their mechanical strength due to progressive destruction under the force of body weight. Extreme weakening leads to angular kyphotic deformity called kyphus.
The severity of the deformity depends upon the extent of destruction, the level of the lesion, and the number of vertebrae involved.
Kyphosis is most marked in the thoracic area because of the normal dorsal curvature. In the lumbar area, it is less because of the normal lumbar lordosis because of which the body weight is transmitted posteriorly and collapse is partial.
The collapse is minimal in the cervical spine because most of the body weight is borne through the articular processes.
Healing takes place by gradual fibrosis and calcification of the granulomatous tuberculous tissue. Eventually, the fibrous tissue is ossified, with resulting bony ankylosis of the collapsed vertebrae.
Paravertebral abscess [abscess around vertebra – literal meaning], formation occurs in almost every case. With the collapse of the vertebral body, tuberculous granulation tissue, caseous matter, and necrotic bone and bone marrow are extruded through the bony cortex and accumulate beneath the anterior longitudinal ligament.
These cold abscesses gravitate along the fascial planes and present externally at some distance from the site of the original lesion.
Some common cold abscesses sites in TB spine are
- Lumbar region – the abscess gravitates along the psoas fascial sheath and usually points into the groin just below the inguinal ligament.
- Thoracic region – the longitudinal ligaments limit the abscess, which is seen in the radiogram as a fusiform radiopaque shadow at or just below the level of the involved vertebra.
-
- Thoracic abscess may reach the anterior chest wall in the parasternal area by tracking via the intercostal vessels.
Neural Deficit in Tuberculosis of Spine
Neurological complications may arise due to compression of the cord by the abscess, caseating or granulating mass, intervertebral disc or edge of bone c. Other contributory factors may be thrombosis of the local vessels and edema of the cord.
The neural deficit in thoracic and upper lumbar regions can be paraparesis [partial weakness of the lower limbs], to begin with, and eventually, lead to paraplegia [complete paralysis of both the lower limbs]. It occurs most often in the mid-or upper-thoracic region, where the kyphosis is most acute, the spinal canal is narrow, and the spinal cord is relatively large.
Cervical tuberculosis can give rise to weakness or complete paralysis of upper as well as lower limbs [quadriparesis or quadriplegia].
The spinal cord ends at L1-L2 levels, therefore lower lumbar regions, if they cause the neural deficit, will cause root lesions only in the involved roots.
Following can contribute to the pressure on the spinal cord, leading to the neural deficit.
- Extradural Mass formed by tubercular abscess [fluid pus, granulation tissue, or caseous material.
- Extradural Granuloma and Tuberculoma
- Sequestra [dead bone] from avascular diseased vertebral bodies or intervertebral disc
- Granulation tissue on the with peridural fibrosis [cicatrization or scar formation]
- Infarction of the cord by thrombosis or arteritis.
- Cord atrophy
Paraplegia due to tuberculosis of the spine can be early-onset or late-onset.
Early-onset paraplegia occurs during the active phase of the vertebral disease usually within first 2 years of the onset.
Late-onset paraplegia occurs many more than 2 years after the disease has persisted and could be due to recrudescence of the disease or mechanical pressure on the cord.
It is also called paraplegia associated with the healed disease.
Types of Lesions in Tuberculosis of Spine
Four types of the lesion are known in tuberculosis of spine
- Paradiscal type – On either side of the disc
- Central type – Central part of the vertebral body
- Anterior type – Anterior surface of the vertebral body
- Appendiceal type (involving pedicles, laminae, spinous process or transverse processes).
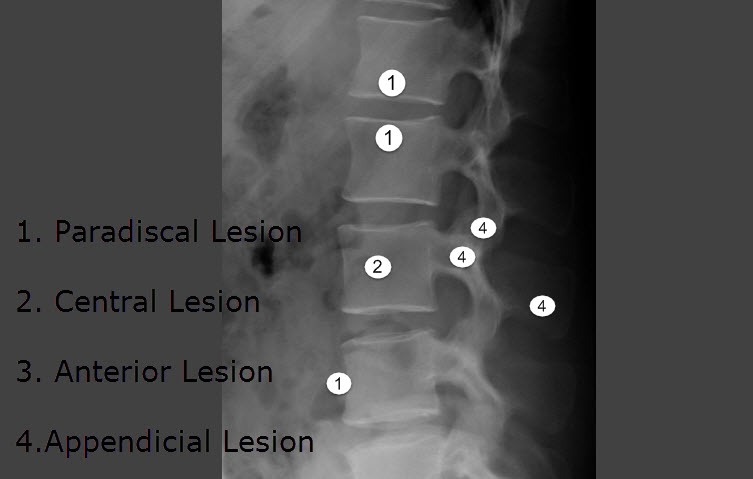
Paradiscal Lesion
In this type, the infection is on either side of the disc, involving two vertebrae. This is the most common type of presentation. The narrowing of the disc space is often the earliest radiological finding, often associated with a fuzziness of The narrowing of the disc space may either be due to either atrophy of the disc tissue or prolapsed.
Central Type of Lesion
The infection starts from the center of the vertebral body, where it reaches through Batson’s venous plexus or through the branches of the posterior vertebral artery.
Loss of disc space is minimal.
Anterior Lesion
The infection starts beneath the anterior longitudinal ligament and the periosteum.
Appendiceal Lesion
This involves isolated infection of the pedicles, transverse processes, laminae, and the spinous process does occur.
These lesions are not generally visible on routine x-rays. CT or MRI is better at detecting these lesions.
Clinical Presentation of Tuberculosis of Spine
The onset of tuberculosis of the spine is usually insidious. However, the acute presentation of tuberculosis is known.
Initial symptoms are vague, consisting of
- Generalized malaise
- Easy fatiguability
- Loss of appetite and weight
- Loss of desire to play outdoors [in children]
- afternoon or evening fever.
A backache is usually minimal and may be referred in the region supplied by the involved segment.
Muscle spasm makes the back rigid. The motion of the spine is limited in all directions. The patient may complain of an inability to flex the spine when picking an object up from the floor.
On examination, the spine is stiff and painful on movement. The stiffness of the spine is noticed by an increase of depth of spinal midline gutter as paraspinal muscle spasm makes them prominent.
There may be a localized kyphotic deformity that would be tender on palpation. A kyphus in the thoracic region may be the first noticeable sign. As the kyphosis increases, the ribs will crowd together and a barrel chest deformity may develop.
A cold abscess may be noticed in some cases. The abscesses may be palpated as fluctuant swellings in the groin, iliac fossa, retropharynx, or on the side of the neck, depending upon the level of the lesion.
In spite of the vast spectrum of the disease, the early cases may not have any clinical findings except for tenderness in the region of the complaint. Several of these symptoms and signs may be absent even in cases of the active vertebral disease.
A history of contact with a known case of tuberculosis or a recent visit to an endemic area should be asked.
When the lesion is situated in the cervical or lumbar spine, a flattening of the normal lordosis is the initial finding.
The gait of the person with Pott’s disease is peculiar, reflecting the protective rigidity of the spine. His steps are short, as he is trying to avoid any jarring of his back. In tuberculosis of the cervical spine, he holds his neck is in extension and supports his head with one hand under the chin and the other over the occiput.
Neurological Deficit in Tuberculosis of Spine
The compression of neural structures leads to signs of neurological deficit. The compression of neural structures is indicated by
- Spasticity of the limbs [uper and lower limbs in case of the cervical spine and lower limbs in case of dorsal and lumbar spines]
- Hyperactive deep tendon reflexes
- Spastic gait
- Motor weakness
- Disturbances of the bladder and anorectal function.
A neural deficit in tuberculosis of spine could be caused by the following factors
- Inflammatory
- Inflammatory edema
- Tuberculous granulation tissue
- Tuberculous abscess
- Tuberculous caseous tissue
- Mechanical
- Tubercular debris
- Sequestra from vertebral body and disc
- Constriction of the cord due to stenosis of the vertebral canal
- Localized pressure due to internal gibbus along the anterior wall of the vertebral canal
- Intrinsic
- Prolonged stretching of the cord over a severe deformity
- Atrophy of cord
- Infective thrombosis/endarteritis of spinal vessels
- Pathological dislocation of spine
- Tuberculous meningomyelitis
- Syringomyelic changes
- Spinal Tumor syndrome
- Diffuse extradural granuloma or tuberculoma
Classification of Neurological Deficit
Neurological deficit in tuberculosis of spine is classified as follows
Stage 1
- The patient walks normally and is not aware of any deficit
- Extensor plantar response
- Ankle clonus
- It May be accompanied by brisk tendon reflexes
Stage 2
- Clumsy gait
- Incoordinated jumpy gait
- Weakness, walks with support
Stage 3
- Severe weakness
- Patient bedridden and cannot walk because
- <50% sensory deficit
Stage 4
- The patient has paraplegia with flexor spasms or paraplegia in flexion.
- Paraplegia in extension with spontaneous flexor spasms
- Sphincter disturbances
- Flaccid paralysis [ occurs due to very severe cord compression]
Neural deficit in tuberculosis is of slow onset.
The earliest symptom may be twitching of muscles in the lower limbs and clumsiness while walking.
Motor functions are almost always affected before and to a greater extent than the sensory functions due to anterior site because the disease is mostly in the anterior part [motor tracts are anterior too] and probably the motor tracts are more sensitive to compression of the cord.
The paralysis as noted above may pass from spastic motor paraparesis to spastic paraplegia in extension and then on spastic paraplegia in flexion.
In severe compression of the cord, flexor spasms may occur which refers to involuntary flexions of the lower limb. This indicates a complete loss of conductivity in the pyramidal and extrapyramidal neural tracts.
Bladder and anal sphincters may be involved.
There may be a sensory deficit. The sense of position and vibration are the last to disappear.
In severe cases, all spasticity disappears and the paralysis becomes flaccid (areflexic paraplegia) with anesthesia and loss of sphincter control.
Sometimes, the insult to the cord is sudden [such as ischemia] and the patient may present with flaccid paralysis ”spinal shock” and later gradually change into spasticity.
Rarely, the disease may present like a ”spinal tumor syndrome” due to a localized tuberculoma or a diffuse granuloma or due to peridural fibrosis.
Differential Diagnosis
Mostly the diagnosis of tuberculosis can be made by clinical and radiological examination by its characteristic findings.
Doubtful cases need to be confirmed by biopsy and/or culture.
The differential diagnoses vary with age of presentation.
- Congenital defects of the spine, Calve’s disease are common differentials in young patients.
- Schmorl’s disease and Scheuermann’s disease may sometimes cause confusion in adolescent patients.
- In adults, other infections and malignancy are major differentials.
Following is a list of main differentials of the tuberculous spine.
- Infections
- Bacterial Spondylitis
- Brucella Spondylitis
- Fungal Spondylitis [rare]
- Syphilis [rare]
- Hydatid Disease [rare]
- Tumors
- Benign Tumors of spine – hemangioma, Giant-cell tumor, Aneurysmal bone cyst
- Malignant Tumors – Ewing’s sarcoma, Osteogenic sarcoma, Fibrosarcomas,Chondrosarcomas, Multiple Myeloma, Lymphomas, Metastases
- Histiocytosis-X – Eosinophilic granuloma (spine-Calve’s disease), Hand-Schuller-Christan disease, Letterer-Siwe disease
- Spinal Deformities
- Hemivertebrae
- Block Vertebrae [Fusion of two or more vertebral bodies]
- Neural arch defects
- Spinal Osteochondrosis – An ischemic lesion of the apophysis of several vertebrae
- Spondylolisthesis
Imaging
Xrays
In addition to the lesion-specific appearance of the disease [ radiolucent lesion, fuzzy vertebral margins, reduced disc space, vertebral collapse – refer to types of the lesions], the following findings may be noted.
Findings are suggestive, but not pathognomonic. Routine views are anteroposterior and lateral views of the spine. Chest radiograms are taken to rule out outer foci of systemic disease in case of a suspected person.
Paravertebral shadows
Paravertebral shadows in TB of the spine is produced by extension of tuberculous granulation tissue and the collection of an abscess in the paravertebral region.
In the cervical region, this presents as increased prevertebral space.
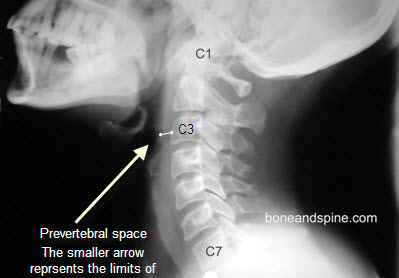
Prevertebral space is soft tissue shadow between the vertebral bodies and pharynx and trachea. On an average, the normal space between the pharynx and spine above the level of cricoid cartilage is 0.5 cm and below this, it is 1.5 cm.
An increased space suggests collection in the prevertebral space.
In the upper thoracic spine, abscess appears V-shaped shadow stripping the lung apices laterally and downwards.
It may also show as squaring of borders of superior mediastinum.
Shifting of tracheal shadow to one side may be present on AP view.
Normal tracheal shadow is concave anteriorly in lateral view of the thoracic spine. Any change in the contour should raise the suspicion of the disease from C7 to D4 vertebrae.
Below that region [D4 vertebra is watershed], a typical fusiform-shape (bird nest appearance) shadow suggests paravertebral abscess.
Abscesses below the diaphragm tend to extend along the course of psoas muscle which may be noted as the bilateral widening of the psoas shadow but is less common.
Kyphus
This occurs in typical para discal lesion due to the collapse of two vertebral bodies.
Lateral Shift and Scoliosis
A lateral curvature and deviation have been recognized as one of the rare deformities of Pott’s disease.
CT and MRI
CT and MRI provide cross-sectional imaging which describes the extent of involvement better and are good at showing the presence of an epidural component and cord compression. MRI is the investigation of choice for this, with CT with contrast being a distant second.
In addition to this, MRI also reveals the status of the spinal cord health.
These show vertebral destruction and paraspinal collections.
Lab Studies
Most of the times, especially in endemic regions, the diagnosis of tuberculosis is clinicoradiological but lab tests are called for help when a clear diagnosis cannot be reached out at.
Routine lab investigations done in Pott’s spine are complete blood count, ESR, and CRP. Liver and kidney functions should also be assessed during treatment.
CBC might show lymphocytosis but could be normal as well.
ESR and CRP are generally elevated but in some cases, the increase is not seen.
ESR is deemed to be an inflammation marker and some authors recommend serial ESR levels to assess the decrease in activity of the tubercular disease.
Tuberculin skin test is found positive in most of the patients with spine TB who are not infected with HIV
Microbiological Studies
The tissue for microbiological studies can be obtained through CT guided biopsy. This is more useful in cases with an equivocal diagnosis.
- AFB staining of the tissue
- PCR for Tuberculosis
- Culture and sensitivity.
Treatment
The treatment of spinal tuberculosis is mainly by chemotherapy. Presence of neurological deficit complicates the matters and for sake of simplicity, I have divided the treatment into two groups
Spine Tuberculosis without Neural Deficit
The prevention of neural deficit in the tuberculosis of the spine is of paramount importance, it can be largely achieved by early diagnosis and prompt treatment.
These patients are treated with antitubercular chemotherapy which consists of
- Isoniazi
- Rifampicin
- Pyrazinamide
- Ethambutol as the first line of drugs
However, depending upon the patient profile, drugs may be added or replaced.
Read more – Drug therapy for Tuberculosis
Gradual mobilization of the patient is encouraged in the absence of neural deficit with the help of suitable spinal braces. After 3 to 9 weeks of starting of the treatment, the patient is started on back extension exercises. The spinal brace is continued for about 18 months to 2 years.
Surface cold abscesses may be aspirated, deeper collections may not be required to drain.
Open drainage of the abscess is performed if aspiration fails to clear the collection.
Sinuses in a large majority of cases heal within 6 weeks to 12 weeks from the onset of the treatment
Periodic evaluation of the patient with X-rays and ESR is done to assess the activity of the disease and decreasing ESR is deemed to be a sign of reducing bacterial activity.
Tuberculosis of Spine with Neural Deficit
Patients with neural deficits require a more aggressive approach. Classical approach was to put all the patients on chemotherapy and strict bed rest.
Some authors in the recent past suggested a radical approach that advocated operating almost every tubercular lesion with [or even without] neural deficit to debride the tissue and relieve the pressure on neural structures.
While the first approach produced less than desirable results, the second one is associated with an increased surgical burden and associated mortality.
The middle path regime solves this problem to a great extent by taking the best of both approaches.
It puts the patient on chemotherapy and rest and observes for a response.
The premise of the treatment is that, as the drugs act on the bacteriae, the reduced destruction and pus production leads to lesser pressure on the neural structures which tend to recover once milieu gets better by use of medicine.
This regime advocates surgery for the patients of TB of the spine who do not get better with the initial treatment or are not candidates for conservative treatment.
Every patient with neural complications will not be cured by antitubercular drugs and rest alone, however, all patients do not need surgical decompression.
Indications for surgery in presence of neural deficit are
- Neurological complications which do not start showing signs of progressive recovery to a satisfactory level after a fair trial of conservative therapy (3 to 4 weeks).
- Patients with spinal caries in whom neurological complications develop during the conservative treatment
- Patients with neurological complications that become worse while they are undergoing therapy with antituberculous drugs and bedrest
- Patients who have a recurrence of neurological complication
- Patients with prevertebral cervical abscesses, neurological signs, and difficulty in deglutition and respiration
- Advanced cases of neurological involvement such as marked sensory and sphincter [bladder/bowel] disturbances, flaccid paralysis or severe flexor spasms.
In the cases who started showing progressive recovery between 3 to 4 weeks and progressed to complete recovery, surgical decompression was considered unnecessary.
Surgery in Tuberculosis of Spine
Surgery in tuberculosis of spine is required mostly for decompression of the neural structures or drainage of abscesses.
Surgery is also done for deformity correction in severe kyphus.
In children, posterior spinal fusion is done so as to correct the deformity with growth.
Various operative Procedures for Decompression of Neural Tissues
- Decompression and debridement with or without bone grafting
- Cervical spine and cervicodorsal junction- anterior approach
- Dorsal spine and dorsolumbar junction – anterolateral approach or transpleural approach
- Lumbar spine and lumbosacral junction – extraperitoneal approach.
- Laminectomy for posterior spinal disease, extradural granuloma or tuberculoma
- Anterior transposition of the cord through the anterolateral in severe kyphotic deformity causing paraplegia.
Recovery after surgery in tuberculosis of spine has been observed after 24 hours to 12 weeks after the decompression. Most of the patients showed the first evidence of objective recovery within 3 weeks of the decompression, however, others took a long time to recover. The time taken for near-complete recovery varied between 3 to 6 months and in few cases more than a year.
Extensor plantar response, a sign of pyramidal tract involvement, lasts for a very long time.
Patients who recover are able to return to their full activity within 6 to 12 months of the treatment. The brace is recommended for about 2 years.
Prognosis
The prognosis of the tuberculosis of spine is determined by the severity and duration of the disease.
If diagnosed and treated in very early stages, before bony destruction and deformity have occurred, the patient of tuberculosis of spine usually recovers completely without any residual problem.
After, vertebral collapse, the deformity occurs. This deformity would persist after the treatment as well when tubercular activity has finished.
If this deformity is severe, it could cause mechanical back pain in later years.
With the neural deficit in tuberculosis of spine, the prognosis is better if there is
- Partial cord involvement
- Neural complications are of short duration
- Early-onset neurological deficit
- The slow progression of neural complications
- Young patient
- Good general condition of the patient
The prognosis is relatively poor if there is
- Complete cord involvement
- Severe flexor spasms
- Flaccid paralysis
- Gross sensory loss
- Long-standing neural complication
- Late-onset neural deficit
- Rapid development of neural complications
- Patient is of older age
- Poor general condition of the patient.
Various modalities generally recover in the following order
- Vibration and joint sensation
- Temperature, touch, pain
- Voluntary motor activity
- Sphincter functions
- Wasting of muscles.
Recurrence or relapse of a tuberculous lesion [ Also called recrudescence of the Disease] poses a special problem. The commonest cause is the grumbling activity of infection caused by resistance strain of acid-fast bacilli.
Surgery may be required in these cases.
Atypical Presentation of the Tuberculosis of Spine
The classical form of tuberculosis of spine is usually easy to recognize. However, atypical forms of the disease may occur involving other parts of the vertebra or also in the form of the extraosseous involvement of the neural and perineural tissue.
These are relatively uncommon and more difficult to diagnose. These lesions are
- Posterior Complex Tuberculosis
- PIntraspinal Tuberculous Granuloma (Tuberculoma)
- Granuloma
- Extradural
- Subdural
- Single Vertebral Disease
- Multiple vertebral skip lesions
- Cold Abscess
- Pan Vertebral Disease