Last Updated on November 22, 2023
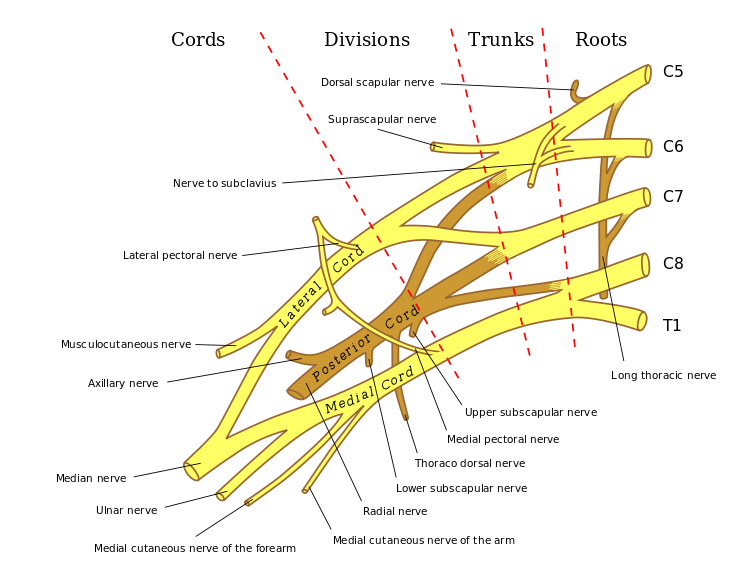
Ulnar neuropathy refers to compression of the ulnar nerve, a continuation of the medial cord of the brachial plexus and a mixed nerve that supplies muscles of the forearm, and skin over medial part of hand and digits.
Ulnar neuropathy is the second most common entrapment neuropathy of the upper limb.
There are various sites where ulnar nerve entrapment can occur. The most common is near the elbow, which is called cubital tunnel syndrome.
The second most likely site is the Guyon canal at wrist. This involvement is termed as ulnar tunnel syndrome.
However, entrapment can occur anywhere along its course for one reason or other.
Most of the cases of ulnar compression neuropathy occur in patients older than 35 years. Cubital tunnel syndrome is 3-8 times more common in men
Anatomy of Ulnar Nerve
[Read detailed anatomy of ulnar nerve]
Ulnar nerve comes from from the medial cord of the brachial plexus and carries fibers from C8-T1.
It lies posteromedial to brachial artery in the anterior compartment of the upper arm and becomes medial to triceps at about 8cm from the medial epicondyle.
Passing behind the medial epicondyle, it enters the cubital tunnel. The tunnel is formed by fascia from deep forearm between two heads of flexor carpi ulnaris and aponeurosis of same muscle [Osborne ligament]. The floor of this tunnel is formed by transverse bands of medial collateral ligament and elbow joint capsule.
Compression of the ulnar nerve at the cubital tunnel leads to cubital tunnel syndrome.
In the forearm, it runs between flexor carpi ulnaris and flexor digitorum profundus after entering the forearm between two heads of flexor carpi ulnaris.
The ulnar nerve, along with ulnar artery, pass the wrist superficial to transverse carpal ligament to enter Guyon’s canal where it divides into sensory and motor branches
Guyon canal which about 4 cm long, begins at the proximal extent of the transverse carpal ligament and ends at the aponeurotic arch of the hypothenar muscles.
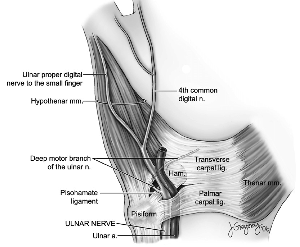
Following structures form the Guyon canal
- Volar carpal ligament forms roof
- Transverse carpal ligament proximally and hypothenar muscles distally form the floor
- Pisiform, pisohamate ligament, abductor digiti minimi muscle belly form ulnar border
- Hook of hamate forms radial border
In the canal, ulnar nerve bifurcates into the superficial sensory and deep motor branches. There are three zones of Guyon canal from proximal to distal
- Zone 1- Extends from the proximal edge of the palmar carpal ligament to the bifurcation of the ulnar nerve. Compression affects both sensory and motor nerves.
- Zone 2 – Extends from the bifurcation of the ulnar nerve just distal to the fibrous arch of the hypothenar muscles. Motor nerve affected only
- Zone 3- Contains the superficial sensory branch of the ulnar nerve.
Muscles supplied by a motor branch in the forearm are flexor carpi ulnaris and slips of flexor digitorum to ring and little finger.
Following hand muscles are supplied
- Adductor pollicis
- Deep head of flexor pollicis brevis (FPB)
- Dorsal & palmar interossei
- 3rd & 4th lumbricals
- Abductor digiti minimi
- Opponens digiti minimi
- Flexor digiti minimi
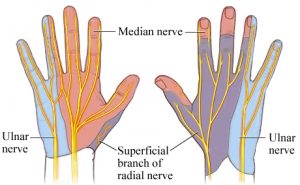
The sensory branch of ulnar nerve divides into dorsal and palmar cutaneous branches, and superficial terminal branches.
The ulnar nerve sensory supply is limited to the little finger and medial half of the fourth digit, and the corresponding part of the palm and dorsum as shown in the figure.
The palmar branch of ulnar nerve supplies anterior skin and nails whereas dorsum distribution is supplied by dorsal cutaneous branch.
Sites of Ulnar Nerve Entrapment

Image Credit: Semantic Scholar
Although the nerve could be injured or entrapped at any point along its course, it is most commonly compressed around the elbow and in the wrist.
Following are the five most encountered sites around the elbow are discussed.
- Intermuscular septum
- Due to the arcade of Struthers
- A thin fibrous band from the medial head of the triceps to the medial intermuscular septum
- 6-10 cm proximal to the medial epicondyle
- Where ulnar nerve pierces the medial intermuscular septum.
- Due to the arcade of Struthers
- Medial epicondylar region
- In valgus deformity of the bone
- Causes extra traction on the nerve
- Tardy ulnar nerve palsy
- Epicondylar groove
- Slightly distal to the medial epicondyle
- A fibro-osseous tunnel holding the ulnar nerve and accompanying vessels
- Cubital tunnel
- The passage between the two heads of the flexor carpi ulnaris
- Two heads connected by Osborne ligament
- This ligament is a continuation of the fibroaponeurotic covering of the epicondylar groove.
- The tunnel flattens during flexion due to ligament stretching causing pressure
- Exit from Flexor Carpi Ulnaris
- perforates a fascial layer between the flexor digitorum superficialis and the flexor digitorum profundus to exit the flexor carpi ulnaris
- Can get compressed
At the wrist, the ulnar can get entrapped in Guyon canal and depending on zone of compression, as discussed in anatomy, the symptoms could be motor or sensory or mixed.
Pathophysiology of Ulnar Nerve Entrapment
During flexion of the elbow following things happen
- The ulnar nerve undergoes longitudinal excursion
- 9-10 mm of proximal to the medial epicondyle
- 3-6 mm distal to medial epicondyle
- Flexion stresses the medial collateral ligaments and the overlying retinaculum causing a reduction in the volume of the canal
- The ulnar nerve elongates by 5-8 mm with elbow flexion
Overall, the traction of the nerve during the flexion movement is thought to be responsible for the increased intraneural pressure and nerve injury.
Subluxation of the ulnar nerve, when it occurs, could also lead to increased compression.
Just to mention here that intraneural and extraneural pressures are lowest at 45 degrees of flexion. It is also the position of rest and immobilization for ulnar nerve entrapment around the elbow.
Wrist extension and shoulder abduction are further known to increase the intraneural pressure.
Depending on the severity of compression the nerve could have neurapraxia, axonotemesis or neurotemesis
[Read more about types of nerve injuries]
Causes of Ulnar Neuropathy
Ulnar neuropathy can be caused by many non-compressive causes such as diabetes or viral infection.
In this article, however, we are restricting ourselves to compressive causes.
Compression can be caused by space-occupying lesions like tumors or constricting bands.
Following causes can lead to compression of the nerve
- Constricting fascial bands
- Subluxation of the ulnar nerve over the medial epicondyle
- Cubitus valgus
- Bony spurs
- Synovial hypertrophy
- Tumors
- Ganglia [wrist]
- Repetitive injury as in occupational exposure
- Compression during general anesthesia
- Blunt trauma
- Deformities (eg, rheumatoid arthritis)
- Hemophilia hematomas
Clinical Presentation
Ulnar neuropathy has a varied presentation. The symptoms could range from mild transient paresthesias in the ring and small fingers to clawing of these digits and severe intrinsic muscle atrophy.
Any trauma pertaining to the course of the ulnar nerve should be noted.
There may be a complaint of numbness, tingling, or burning in the fourth and fifth digit, which is the area of distribution of the ulnar nerve.
The pain is rarely a complaint. In elbow lesions, the pain may in the elbow but not in the hand.
Weakness may also be a presenting complaint. This is due to weakness of muscles supplied by ulnar nerve [see list above, in the anatomy].
Patients of ulnar neuropathy may find difficult to open jars or turning doorknobs. They may complain of fatigue or weakness of hand muscles with repetitive work.
A very peculiar complaint is little finger gets caught on the edge of the pants pocket when she tries to place the hand into the pocket. The process requires adduction of the fingers which is deficient due to ulnar nerve involvement. The little finger is most expressive because the action of extensor quinti minimi keeps the finger abducted [as it attaches on the ulnar side] and extends.
The weakness of pinch or grip indicates the weakness of thumb adductor and first dorsal interosseous which is adducts of the index finger.
On examination, there is the clawed posture of hand which is marked by the extension of the fourth and fifth digit at metacarpophalangeal joint.

Ulnar claw hand is term referred to the condition of the hand that results due to ulnar neuropathy. Lumbricals which extend interphalangeal joints and flexion of metacarpophalngeal joints. Their weakness causes hyperextension of metacarpophalangeal joint and flexion at the interphalangeal joints of 4th and 5th digit.
The posture is also called the benediction sign or the benediction hand because it appears similar to a priest hand blessing.
A complete examination of the extremity and neck is done especially emphasis at following points
- Examination of upper limb and palpation along course of the nerve
- Complete motor and sensory examination of the hand
- Special tests for ulnar nerve function evaluation
Cervical involvement should be ruled out based on clinical findings.
Special Test for Ulnar Neuropathy
Elbow flexion test
It is considered a diagnostic test for cubital tunnel syndrome. In this patient is asked to
- Flex the elbow past 90 degrees
- Supinate the forearm
- Extend the wrist
A discomfort or parasthesia within 60 seconds means a positive test.
Shoulder internal rotation test
- The shoulder is kept at 90° of shoulder abduction, maximal internal rotation, and 10° of flexion
- The elbow flexed 90°
- The wrist in the neutral position
- Fingers are extended
The test is specific to cubital tunnel syndrome and considered positive if any symptom appears within 10 seconds.
Froment sign
The patient is asked to hold a piece of paper between the thumb and index finger while the examiner attempts to pull it away.
The test is considered positive if
- Flexion of the interphalangeal joint rather than adduction is used to hold the paper or
- The patient is not able to hold the paper as examiner pulls
- Indicates adductor pollicis paralysis [ulnar nerve damage]
The compensatory interphalangeal joint flexion is due to hyperflexion by flexor pollicis longus.
Thus, in addition to the weakness, the examiner sees flexion of the tip of the thumb.
Jeane’s sign
If a simultaneous MCP extension occurs this is known as Jeanne’s Sign which is additional ulnar nerve damage
Wartenberg sign
The patient has abduction posturing of the little finger due to unopposed action of abductor digiti quinti.
Allen test
Allen test is used to diagnose ulnar artery thrombosis
If a Martin-Gruber anastomosis in the forearm or a Riche-Cannieu anastomosis in the palm is present, the examiner may be deceived by the apparent functioning of ulnar-innervated muscles.
Tinel Sign
The examiner taps over the ulnar groove and further with a reflex hammer. Presence of definite paresthesias in the ulnar portion of the hand, especially in the last two digits.
The test may not be very sensitive and false positive in some individuals.
Localizing the Lesion Based on Examination
Localization of the lesion of ulnar neuropathy is reached at by available findings from history and examination, and then confirmed and sometimes established by investigations.
The history itself might provide some cues if present. Any pain, swelling, surgery in a region would suggest the site of compression.
The motor and sensory examination provide enough signs to differentiate if the lesion is around the elbow or below though sometimes, it is still difficult to deduce.
We begin with motor examination first.
As we discussed before, the following hand muscles are supplied
- Adductor pollicis
- Deep head of flexor pollicis brevis (FPB)
- Dorsal & palmar interossei
- 3rd & 4th lumbricals
- Abductor digiti minimi
- Opponens digiti minimi
- Flexor digiti minimi
These muscles are tested for their strength and function.
Flexor carpi ulnaris and flexor digitorum profundus are supplied in the forearm. Therefore the involvement of these muscles occurs only in cases where the entrapment of the ulnar nerve is higher to the point where branches to these muscles come out. These muscles would not be involved in compression that occurs in the wrist.
Often the branch to the flexor carpi ulnaris splits off from the main trunk before the branch to profundus muscle. Therefore sparing of flexor carpi ulnaris may occur more often.
Thus, if both the intrinsic hand muscles and forearm muscles supplied by the ulnar nerve are involved, then the lesion is in the elbow region.
If these muscles are spared, most likely, the lesion is in the wrist but it could be in elbow region after the branches to the forearm muscles have come out.
Another issue is the structural organization of the ulnar nerve fibers as separate fascicles. It could be that compression affects some fascicles only producing an atypical picture.
In addition to this differentiation, it must be established that the ulnar neuropathy is not due to lesions of brachial plexus or cervical spine. This can be assessed by examination of other muscles supplied by C8-T1 fibers. Examination of medial-cord [of brachial plexus] muscles can reveal if the lesion is higher.
[To know medial cord and brachial plexus distribution, read brachial plexus anatomy]
Abductor pollicis brevis is also supplied by C8-T1 fibers by median nerve and its examination would reveal if the lesion is in the ulnar nerve or affects brachial plexus/ cervical spinal cord.
Ulnar neuropathy at or distal to the wrist is characterized by weakness of the interosseous and hypothenar muscles but no weakness in forearm muscles.
Sensory involvement would provide a cue to the zone of compression.
Following scenarios are possible
- Hypothenar and interosseous muscle weakness without sensory loss
- Compression of the deep motor branch
- Sometimes hypothenar muscles are spared if compression is after the hypothenar branch is given off
- The weakness of the interosseous and hypothenar muscles, with sensory involvement in the fifth digit
- Compression of both the deep motor branch and the superficial terminal sensory branch
- Classical Guyon canal compression pattern
- Pure sensory loss
- Compression distal to the canal of Guyon
- There is entrapment of superficial terminal sensory branch
- Other sensory branches are spared as they are given before entering Guyon’s canal
- Dorsal ulnar cutaneous sensory nerve,
- Palmar cutaneous sensory nerve
Sensory examination
Though the ulnar nerve has a defined area of sensory supply, the exact findings would depend on which nerve branch is affected and individual variations of supply.
For example, the area of the palmar cutaneous sensory nerve can be a bit farther proximally than is usual.
Presence of sensory loss beyond the defined area, say for example, above the wrist crease should raise doubts of C8-T1 involvement at a higher level.
As they both do not enter, the Guyon canal, palmar and dorsal cutaneous sensory branches are often spared in GUoyn canal compression but terminal sensory branch may get involved.
Therefore, a compression at the canal of Guyon might be detectable on examination only in the tips of the fingers [ the superficial terminal branch]
Differential Diagnosis
- Non compressive Neuropathy
- Alcohol
- Viral infection
- Diabetes
- Amyotrophic Lateral Sclerosis
- Brachial Plexus Injuries
- Cervical Disc Disease
- Cervical Spondylosis
- Thoracic Outlet Syndrome
- Traumatic Peripheral Nerve Lesions
Lab Studies
lab studies are not useful in compressive lesions. but they are helpful in ruling out medical causes and infections.
- Complete blood cell count
- Fasting blood glucose
- Hemoglobin A1C
- Renal function tests
- Angiotensin-converting enzyme
- Antinuclear antibody
- Lyme serology
- Thyroid function tests
- Vitamins B-12, B-1, B-6 and Folate levels
- Tissue transglutaminase antibody/Gliadin antibody – Gluten sensitivity
- HIV serology
- Hepatitis serology
Imaging
X-rays
- X-rays of the cervical spine to rule out cervical disease
- X-ray chest – Pancoast tumor or tuberculosis
- X-ray of the elbow
- Look for abnormal anatomy such as
- Valgus deformity
- Bone spurs
- Shallow olecranon groove
- Osteochondromas
- Any sign of fracture or dislocation
- Lesions that destroy bone- tumors, infections, or abnormal calcifications.
- Look for abnormal anatomy such as
- X-ray of the wrist
- Fractures of the hook of the hamate
- Dislocations
- Soft-tissue mass/calcification
X-rays may help to rule our double lesions or the entrapment of the ulnar nerve may occur at more than one level.
Ultrasonography
Examination by ultrasound helps to identify sites of compression and can tell about the cause as well like tumor or cyst.
It can highlight structural alterations like change in the diameter of the nerve at the site of compression and swelling of the nerve just before the compression.
It can identify nerve transection in peripheral nerve injuries.
Magnetic Resonance Imaging
MRI has a limited role in nerve entrapments.
Electromyography and Nerve Conduction Studies
These are classicial nerve studies which are used to confirm
- The area of compression
- Extent of compression
- Can detect double lesions [double-crush]
Motor and sensory conduction velocities are more useful in acute entrapments.
In chronic neuropathies, both conduction velocities and electromyography are done because electromyography can show axonal degeneration.
Electromyography is also used when determining the efficacy of conservative treatment.
Treatment of Ulnar Neuropathy
Non-operative Treatment
Non-operative methods are most likely to be successful when the symptoms are only pareasthesiae and these are transient. Often these are caused by malposition of the elbow or blunt trauma.
Moreover, in cases of non-compressive causes, treatment of underlying cause helps to recover ulnar neuropathy.
The measures taken generally are
- Drugs
- NSAIDs
- Tricyclic antidepressants and related drugs
- Anticonvulsant drugs
- Opioid drugs
- Oral vitamin supplements
- Physical therapy
- Occupational therapy
- Nerve gliding, sliding, or tensioning exercises
- Elbow’s flexors-extensors exercises
- Limitation of activity
- Restrict the range of joint motion
- Decrease the repetitive activity
- Splinting
- Cushions to avoid the effects of pressure
- Elbow pad or splint for prevention of excess flexion
- In the night for 3 months
- Add day splinting for another 3 weeks if the symptoms do not improve
- Continue splints for 6 weeks after resolution of symptoms
- A pillow or folded towel or commercial soft elbow splint the antecubital fossa to extend the elbow
In case of a fracture of the hook of the hamate with ulnar nerve palsy, the limb is immobilized for 4-6 weeks. Surgery is indicated if symptoms progress during this time.
Operative Treatment
More specifically, indications for surgery for ulnar nerve entrapment include the following:
- A long-standing lesion with muscle wasting or clawing
- No resolution in symptoms in 6-12 weeks of conservative treatment
- Progressive palsy or paralysis
The various operative procedures are
- In situ decompression
- Decompression with anterior transposition in the elbow
- Medial epicondylectomy
- Decompression of the Guyon canal
Surgery is also the treatment in traumatic injuries, resection of masses or cysts, and sectioning of fibrous bands.
Surgical Procedures
Decompression in Situ
This means a localized decompression of the nerve. At the elbow, this has the advantage of preserving vascular supply when compared to transposition. But it carries a higher recurrence rate.
It is indicated in mild compression of the ulnar nerve.
THid procedure should not be used when there is pre-existing scarring or chronic subluxation of the ulnar nerve.
Decompression With Anterior Transposition
It is the operation of choice for most of the cases. Anterior transposition moves the nerve to healthy bed from an unsuitable one and causes effective lengthening that does not undergo tension with elbow flexion.
It is more technically demanding and carries the risk of complications like devascularization of the nerve. It is done in presence of altered anatomy like valgus, nerve subluxation, presence of structural lesions like osteophytes, ganglion, etc.
Medial Epicondylectomy
This is also done to release the pressure on the ulnar nerve at the elbow. Removal of the epicondyle removes a compressive area.
However, it allows for greater migration of the ulnar nerve with elbow flexion. There is a potential for elbow instability.
The procedure is indicated in nonunion of an epicondyle fracture with ulnar nerve symptoms and ulnar nerve subluxation
However, the decompression (neurolysis) alone showed greater effectiveness in relieving pain at the elbow.
Decompression of Guyon Canal
This is done to relieve the compression. All the zones should be explored and released in the surgery.
Various decompression options as needed are
- Release of hypothenar muscle origin
- Decompression of ganglion cysts
- Resection of the hook of hamate
- Treatment of ulnar artery thrombosis
Complications of Surgical Intervention
- Failure to decompress the nerve adequately
- Injury to the nerve
- Neuroma
- Infection
- Thrombophlebitis
Prognosis
A favorable outcome is noted in more than 90 percent of cases. The sensory outcome is better than the motor.
Following factors are associated with the poor prognosis
- Age more than 50 years
- Coexisting peripheral polyneuropathy due to diabetes or other causes
- Muscle atrophy
- Absent ulnar sensation
With appropriate decompression, the patient should be a return to normal function.
In chronic palsy with pain, muscle weakness, or atrophy, the surgical outcome is less certain.
Tardy Ulnar Nerve Palsy
Tardy ulnar nerve palsy is ulnar neuropathy that occurs long after the injury of medial condyle. It could occur in supracondylar fracture of the humerus, malunited lateral condyle injury with cubitus valgus or injury to medial condyle/epicondyle.
Tardy means slow. This neuropathy develops over the years and therefore is called tardy.
References
- Elhassan B, Steinmann SP. Entrapment neuropathy of the ulnar nerve. J Am Acad Orthop Surg. 2007 Nov. 15(11):672-81.
- Khoo D, Carmichael SW, Spinner RJ. Ulnar nerve anatomy and compression. Orthop Clin North Am. 1996 Apr. 27(2):317-38.
- Bradshaw DY, Shefner JM. Ulnar neuropathy at the elbow. Neurol Clin. 1999 Aug. 17(3):447-61, v-vi.
- McPherson SA, Meals RA. Cubital tunnel syndrome. Orthop Clin North Am. 1992 Jan. 23(1):111-23.
- Dy CJ, Mackinnon SE. Ulnar neuropathy: evaluation and management. Curr Rev Musculoskelet Med. 2016 Jun. 9 (2):178-84.
- Boyer M. Simple decompression did not differ from simple decompression plus anterior transposition of the nerve for
- Karthik K, Nanda R, Storey S, Stothard J. Severe ulnar nerve entrapment at the elbow: functional outcome after minimally invasive in situ decompression. J Hand Surg Eur Vol. 2012 Feb. 37(2):115-22.
- Broudy AS, Leffert RD, Smith RJ. Technical problems with ulnar nerve transposition at the elbow: findings and results of reoperation. J Hand Surg Am. 1978 Jan. 3(1):85-9.