Last Updated on November 22, 2023
Ulnar tunnel syndrome is neuropathy [disease or dysfunction of nerve] of the ulnar nerve caused by compression in Guyon’s canal or the ulnar canal or ulnar tunnel.
Guyon’s canal is a longitudinal space in the wrist which allows passage of the ulnar artery and ulnar nerve into the hand. Guyon was a French Urologist who described this space in 1861.
Ulnar tunnel syndrome is also known as handlebar palsy as it is seen in cyclists.
Relevant Anatomy
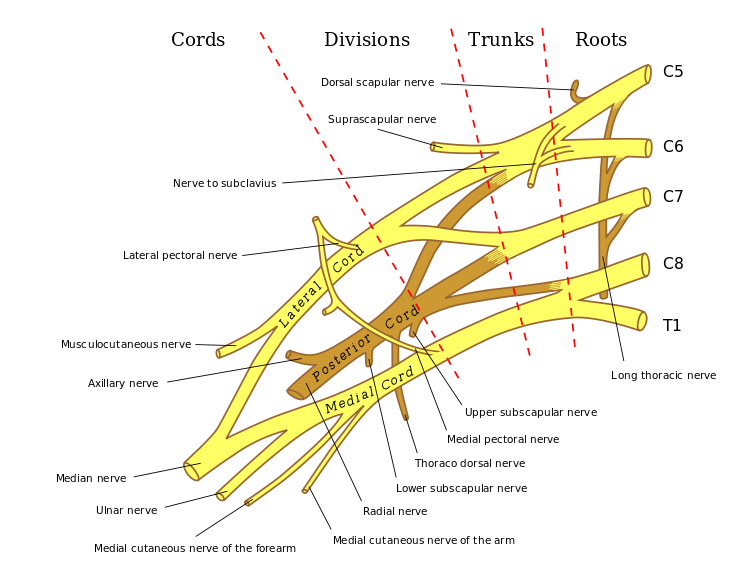
Ulnar nerve comes from from the medial cord of the brachial plexus and carries fibers from C8-T1.
It lies posteromedial to brachial artery in the anterior compartment of the upper arm and becomes medial to triceps at about 8cm from the medial epicondyle.
Passing behind the medial epicondyle, it enters the cubital tunnel. The tunnel is formed by fascia from deep forearm between two heads of flexor carpi ulnaris and aponeurosis of same muscle [Osbourne ligament]. The floor of this tunnel is formed by transverse bands of medial collateral ligament and elbow joint capsule.
Compression of the ulnar nerve at the cubital tunnel leads to cubital tunnel syndrome.
In the forearm, it runs between flexor carpi ulnaris and flexor digitorum profundus after entering the forearm between two heads of flexor carpi ulnaris.
The ulnar nerve, along with ulnar artery, pass the wrist superficial to transverse carpal ligament to enter Guyon’s canal where it divides into sensory and motor branches
Guyon canal which about 4 cm long, begins at the proximal extent of the transverse carpal ligament and ends at the aponeurotic arch of the hypothenar muscles.
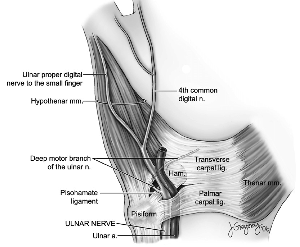
Following structures form the Guyon canal
- Volar carpal ligament forms roof
- Transverse carpal ligament proximally and hypothenar muscles distally form the floor
- Pisiform, pisohamate ligament, abductor digiti minimi muscle belly form ulnar border
- Hook of hamate forms radial border
In the canal, ulnar nerve bifurcates into the superficial sensory and deep motor branches
Muscles supplied by a motor branch in the forearm are flexor carpi ulnaris and slips of flexor digitorum to ring and little finger.
Following hand muscles are supplied
- Adductor pollicis
- Deep head of flexor pollicis brevis (FPB)
- Dorsal & palmar interossei
- 3rd & 4th lumbricals
- Abductor digiti minimi
- Opponens digiti minimi
- Flexor digiti minimi
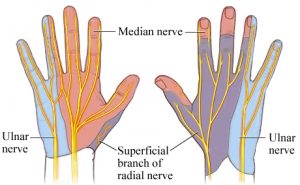
The sensory branch of ulnar nerve divides into dorsal and palmar cutaneous branches, and superficial terminal branches.
The ulnar nerve sensory supply is limited to the little finger and medial half of the fourth digit, and the corresponding part of the palm and dorsum as shown in the figure.
Palmar branch of ulnar nerve supplies anterior skin and nails whereas dorsum distribution is supplied by dorsal cutaneous branch.
Causes of Ulnar Tunnel Syndrome
Compression of the ulnar nerve at Guyon’s canal is caused by
- Ganglion cyst (80% of nontraumatic causes)
- Lipoma
- Repetitive Injury
- Ulnar artery lesion
- Thrombosis
- Aneurysm
- Trauma
- Fracture of Hook of hamate fracture
- Dislocation of pisiform
- Inflammatory arthritis
- Fibrous band
- Congenital bands
- Palmaris brevis hypertrophy
- Idiopathic
There are three zones of compression of Guyon’s canal that could lead to ulnar tunnel syndrome.
Zones of Guyon’s canal

Image Credit: Orthobullet
Zone 1
This zone extends from the proximal edge of the palmar carpal ligament to the bifurcation of the ulnar nerve. Compression in this zone would compress both sensory and motor nerves.
Ganglia and hook of hamate fractures are the main causes in this zone.
Zone 2
Zone 2 extends from the bifurcation of the ulnar nerve just distal to the fibrous arch of the hypothenar muscles.
Like zone 1, ganglia and hook of hamate fractures are the main causes. The manifestation is motor only.
Zone 3
This zone contains the superficial sensory branch of the ulnar nerve and the compression is mainly caused by ulnar artery thrombosis or aneurysm. The symptoms are sensory only.
Depending on the site of lesion and nerve fiber involvement, the compression could lead to symptoms which are motor only, sensory only or mixed.
Clinical Presentation of Ulnar Tunnel Syndrome
As noted the presentation of symptoms could be motor or sensory or mixed.
Ulnar tunnel syndrome usually produces symptoms in the hands and wrist, especially the little finger and ring finger.
The patient may complain
- Numbness or tingling sensations (paresthesia)
- Weakness of hand muscles
- Hand grip weakness
- Claw deformity of the hand
Physical signs are also based on these effects
Physical examination reveals
- Wasting of intrinsic muscles (adductor pollicis, deep head FPB, interossei, and lumbricals 4 and 5)) of as depicted by emptying of intermetacarpal spaces
- Clawing of ring and little finger caused by loss of intrinsics which flex metacarpophalangeal joints and extend interphalangeal joints
- The grasp and pinch is weak ( Due to metacarpophalangeal joint flexion and loss of thumb adduction respectively)
Following is an ulnar claw hand. Look at the flexion of little finger and ring finger. Little finger flexion is more appreciable.
Froment sign
The patient is asked to hold a piece of paper between the thumb and index finger while the examiner attempts to pull it away.
The test is considered positive if
- Flexion of the interphalangeal joint rather than adduction is used to hold the paper or
- The patient is not able to hold the paper as examiner pulls
- Indicates adductor pollicis paralysis [ulnar nerve damage]
The compensatory interphalangeal joint flexion is due to hyperflexion by flexor pollicis longus which is supplied by anterior interosseous nerve.
Jeane’s sign
If a simultaneous MCP extension occurs this is known as Jeanne’s Sign which is additional ulnar nerve damage
Wartenberg sign
The patient has abduction posturing of the little finger due to unopposed action of abductor digiti quinti.
Allen test
Allen test is used to diagnose ulnar artery thrombosis
Imaging
X-rays and CT scan are useful to evaluate hook of hamate fractures. MRI is good for evaluating compression by ganglion cysts or ulnar artery aneurysm.
useful to evaluate for a ganglion cysts
Nerve Conduction Studies are helpful in establishing diagnosis and prognosis
Differential Diagnoses
Cubital tunnel syndrome is due to compression of the nerve at the elbow region. The clawing is less in this case and forearm muscles supplied by ulnar nerve are also affected.
Treatment of Ulnar Tunnel Syndrome
Non-operative treatment is the first line of treatment in mild symptoms and consists of activity modification, drugs for pain and splinting.
Operative treatment is considered when conservative treatment fails or symptoms are very severe.
Following surgical options are used
Local Decompression
This is done to relieve the compression. All the zones should be explored and released in the surgery.
Various decompression options as needed are
-
- Release of hypothenar muscle origin
- Decompression of ganglion cysts
- Resection of the hook of hamate
- Treatment of ulnar artery thrombosis
Tendon Transfers
For correcting claw fingers, following tendons can be used
- Extensor carpi radialis longus
- Extensor carpi radialis brevis
- Palmaris longus
Tendons are passed volar to the transverse metacarpal ligament so that they could flex the proximal phalanx.
Tendons are attached to A2 pulley of the ring and small fingers
For the restoration of the pinch, the preferred procedure is Smth transfer which uses extensor carpi longus brevis or flexor digitorum superficialis of the ring finger.
To restore adduction of the small finger, transfer ulnar insertion of extensor digiti minimi to A1 pulley or radial collateral ligament of the small finger
Carpal tunnel release is done when there is associated with carpal tunnel syndrome.
