Last Updated on November 19, 2019
Wrist arthrocentesis is the procedure of aspirating fluid from wrist joint and is used for diagnosis and therapy of various pathologies of the wrist.
The wrist joint is anatomically complex and can be approached from any side but the dorsal approach is the preferred site for wrist arthrocentesis.
Relevant Anatomy of Wrist Joint
Indications of Wrist Arthrocentesis
Diagnostic
- Acute monoarticular [that affects a single joint] arthritis
- Suspected infection (eg, septic arthritis)
- Inflammatory joint effusion
- Gout
- Pseudogout
- Rheumatologic disorders
- Reactive arthropathies
Therapeutic
- To relieve a large painful effusion.
- Instillation of medications
- Repeated arthrocentesis for septic arthritis in carefully selected patients as a means of decreasing bacterial load
Contraindications
- Cellulitis in the overlying skin
- Overlying skin lesions (eg, dermatitis or psoriasis)
- Known bacteremia
- Bleeding disorders
- Patient on anticoagulation medication
Procedure of Wrist Arthrocentesis
- The patient should be in a comfortable supine position and the wrist should be palmar flexed. Placing a rolled towel or sandbag under the wrist would help.
- Identify and mark the landmarks and prepare the part with povidone-iodine solution or alcohol solution
- For local anesthesia, infiltrate the skin and subcutaneous tissues with 1% or 2% lidocaine. Topical ethyl chloride may be used.
- Insertion of the needle
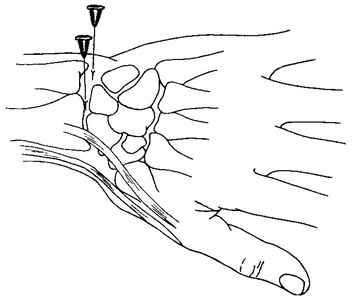
- Dorsally just distal to the radius and just ulnar to the anatomic snuff-box – Avoid extensor carpi radialis brevis and extensor pollicis longus tendons. Direct the needle perpendicular to the skin. If the bone is hit, pull the needle back and redirect it slightly toward the thumb.
- Radial entry – The hand and wrist are relaxed in a slightly flexed position. The joint space can be located by palpating the edge of the distal radius just medial to the thumb extensor tendon.
Ulnar deviation widens the joint space.
- Another approach is from the ulnar side. Keeping the wrist in the same relaxed position, the joint space can be identified by palpating just distal to the distal ulna. The 22-gauge needle is directed in a volar and radial direction.
- Bedside ultrasonography may be useful as an adjunct for joint aspiration by helping to localize the optimal site for needle placement.
- A pop or give way is felt as the needle enters the joint.
- The fluid could be withdrawn now. The ease of withdrawal is determined by the needle size, the viscosity, amount of fluid and the presence of any fibrin clots.
- If the fluid cannot be withdrawn, rotating the needle, withdrawing it slightly, or even reinjecting a little of the fluid often helps unclog the needle and allows additional fluid to be withdrawn. The bore of the needle used may be varied depending on the viscosity of the fluid to be withdrawn.
- After the procedure is done and the sample is taken the needle is withdrawn. In therapeutic cases where injections are to be given, the only syringe is removed keeping the needle secure in the place and the desired medication injected.
- At the end of the injection procedure, the needle should be swiftly withdrawn, and light pressure should be put on the needle site in the skin.
Complications of Wrist Arthrocentesis
Infection is a small but significant risk. The sterile technique minimizes the risk. In cases where risk is gauged higher, the patient may be put on prophylactic antibiotics.
The estimated risk of septic arthritis following aspiration or corticosteroid injection is estimated to be between 1 in 2000.
Tendon rupture and nerve injuries are even rare and often result from misplaced needles.