Last Updated on October 28, 2023
Periosteal chondroma is a benign cartilage tumor that develops on the surface of bone under the periosteum. It is also called as juxtacortical chondroma. Chondroma consists of mature hyaline cartilage.
Periosteal chondromas are rare lesions and account for less than 1% of all chondromas. The majority of cases are diagnosed during the second and third decades of life but the condition is known to affect various age groups. Males are known to be more affected than females.
Unlike osteochondromas, periosteal chondroma is known to grow into adulthood as well. Osteochondroma stops growing after skeletal growth stops.
Long tubular bones of the extremities are typically affected by juxtacortical chondroma. The proximal humerus is most commonly affected, almost contributing for 50% of the cases. It may also involve the bones of the hands and feet.
Periosteal chondromas occur in the second to fourth decades of life.
Pathology of Periosteal chondroma
Microscopic features are typical of a chondroma with a hyaline cartilage matrix. On average, juxtacortical chondromas can show mild nuclear atypia or binucleated chondrocytes. Scalloping and erosion of the outer cortex are seen microscopically.
Some periosteal chondromas may bulge for a short distance into of intervening lamellar bone.
Typically, a fibrous capsule overlies the tumor. Occasional foci of necrosis and myxoid degeneration are present but not as extensive as in malignant lesions.
Mutations in isocitrate dehydrogenase 1 and 2 (IDH1 and IDH2) genes have been described in periosteal chondromas. These are known to occur in enchondromas, and periosteal and central chondrosarcoma, suggesting similar modes of tumor formation.
Mutations of the enzyme results in accumulation of gamma-2-hydroxyglutarate which is an oncometabolite.
Clinical Presentation
This surface lesion most often presents as a palpable mass.
Slowly progressive painful mass is the most common cause of presentation. The pain is due to enlargement of the lesion or from impingement on adjacent soft-tissue structures.
Physical examination reveals a firm and immobile mass which is painful to touch.
Presence of periosteal chondromas near tendon insertion sites may disturb their function causing pain and local discomfort on activity. In deep-seated surfaces, these could be initial symptoms.
Periosteal chondromas are always not symptomatic though. These are sometimes discovered incidentally on radiographs.
Imaging
X-rays
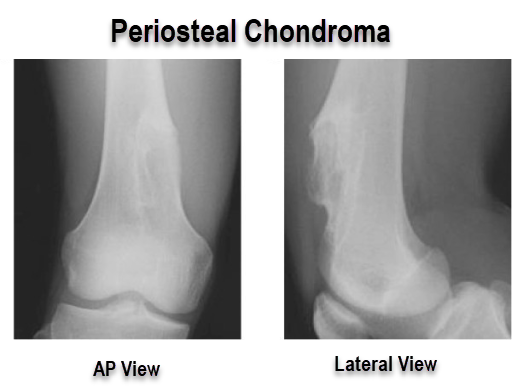
X-rays reveal a well-circumscribed surface lesion of bone, usually of size 1-5 cms, with variable punctate calcifications on radiographs. The cartilaginous nature of juxtacortical chondroma is easy to recognize on plain radiographs.
The cortex beneath the lesion is usually eroded but it is not completely disrupted. Complete cortex disruption is not there. the lesion is clearly demarcated from the medullary cavity by a continuous rim of cortical bone.
There would a varying degree of subcortical sclerosis beneath the lesion.
The elevated periosteum is seen as solid buttresses of mature subperiosteal bone. It can sometimes slightly overhang the edges of the central excavation especially in cases of the smaller periosteal chondromas
CT/MRI
Computed tomography, magnetic resonance imaging, or both modalities also may be needed to evaluate the extent of involvement and the relationship between the lesion and adjacent structures.
On magnetic resonance imaging (MRI), the lesion is best seen on T2-weighted images as a well-defined lobular mass. No evidence of tumor extension into the adjacent medullary canal is present.
It shows the presence of the elevated periosteum overlying the lesion is best documented on magnetic resonance images.
The lesion is clearly separated from the medullary cavity by a rim of sclerotic cortical bone.
Differential Diagnosis
- Juxtacortical chondrosarcoma
- Periosteal osteosarcoma
Treatment
Asymptomatic stable lesions can be monitored. Though the risk of malignant transformation is very small, asymptomatic periosteal chondromas should be followed regularly with clinical examination and x-rays.
A lesion that enlarges over a period or is symptomatic should be treated.
Complete local excision of juxtacortical chondroma is a curative procedure. Because periosteal chondromas may demonstrate radiologic overlap with juxtacortical chondrosarcoma, excision of the lesion is the preferred mode of the treatment.
The excision should include a rim of the underlying cortex as well.
In selected skeletal sites such as the ribs and fibula, segmental resection is the preferable mode of treatment.
Curettage is not done because of the associated risk of recurrence.