Last Updated on October 28, 2023
Spinal accessory nerve palsy often occurs due to lesions in the neck, most often due to iatrogenic reasons. The nerve is especially vulnerable in the posterior triangle of the neck owing to its long and superficial course in the posterior cervical neck.
Iatrogenic spinal accessory nerve injury most commonly occurs following diagnostic lymph node biopsies of the posterior triangle of the neck.
Spinal accessory nerve palsy results in shoulder dysfunction that affects the overall quality of life. Early identification and timely intervention consequently results in better therapeutic outcomes.
Relevant Anatomy
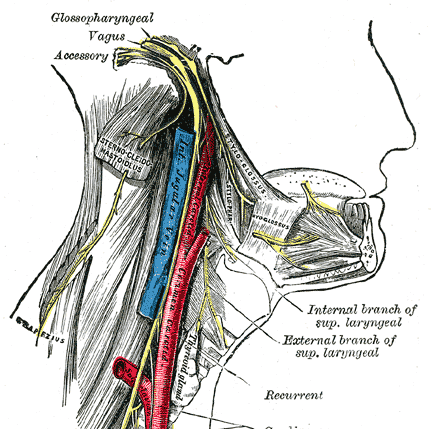
Spinal accessory nerve is XI cranial nerve that consists of two components – spinal and cranial.
Spinal component arises from upper 4-7 spinal segments and travels up to meet the cranial component from medulla to form a bundle that enters the skull through the foramen magnum. It travels towards jugular foramen to exit along with the vagus nerve.
The cranial component joins the vagus nerve and the spinal component travels down to enter sternocleidomastoid muscle and supplies it. It continues further downward journey in the posterior cervical triangle to reach trapezius where it also receives cervical connections. It often gives an independent branch to upper trapezius and rest of the muscle is supplied by the plexus formed between cervical connections and spinal accessory nerve.
Causes of Spinal Accessory Nerve Palsy
Most of the cases are due to injury, iatrogenic injury being the most common.
Iatrogenic
- Lymph node biopsy in the posterior triangle of the neck ( common cause)
- Radical neck dissection in malignant tumors
- Neck surgery
- Benign Tumor Surgery
- Parotidectomy
- Carotid vessel surgery
- Internal jugular vein manipulation
- Facelift surgery
Traumatic
- Penetrating injury
- Blunt injury
- Direct blow
- A knot in sling leading to pressure injury
- Unsuccessful hanging [noose pressure]
- Severe dislocations of the acromioclavicular joint
- Whiplash injury
Neurologic
- Poliomyelitis
- Motor neuron disease
- Brachial neuritis
- Syringomyelia
- Collet-Sicard syndrome [inolves the lower cranial nerves (IX, X, XI, and XII)
- Vernet syndrome [tumor near jugular foramen – involves the lower cranial nerves IX, X, and XI nerves]
- Brachial plexitis
Idiopathic
- Few cases of spontaneous spinal accessory nerve palsy have been reported
Pathophysiology of Nerve Injury
The nerve injured or transected during surgery could be the main branch or a small branch that innervates the upper trapezius muscle.
Traction, skeletonization [stripping of tissue], and devascularization of the nerve during neck dissection can injure the nerve.
These insults lead to segmental demyelination and loss of nerve function.
Most of the presenting symptoms and signs are attributable to denervation of the upper trapezius muscle.
Current evidence suggests that there is a variable contribution of both cervical and spinal accessory nerve motor innervation to the trapezius.
Therefore, sometimes the unpredictable motor and sensory deficits that arise from transection of the nerves to this muscle.
The nerve injury in the neck causes trapezius muscle paralysis.
However, if the nerve is injured before entering sternocleidomastoid muscle, there would be a weakness of sternocleidomastoid muscle as well.
The pain in trapezius paralysis is multifactorial. Frequent straining of supporting muscles (rhomboids and levator scapulae) and traction on the brachial plexus are generally responsible.
Clinical Presentation of Spinal Accessory Nerve Injury [Trapezius Paralysis]
Most of the symptoms as noted are produced by paralysis of the trapezius.
Shoulder pain is the most common complaint. The pain could radiate to the neck, upper back and to the ipsilateral arm. Pain is worsened when the shoulder is not supported.
Pain may worsen when the weight of the involved shoulder is not supported, placing strain upon the shoulder joint.
The patient would also complain of decreased power when performing overhead activities or where shoulder bears weight.
On examination, the shoulder may droop and scapular winging may be present.
There would be a loss of sustained abduction. In old cases, the range of motion decreases due to adhesive capsulitis.
Sternoclavicular joint hypertrophy or subluxation may occur. This happens because of abnormal stress on the medial clavicular head after the loss of the trapezius muscle support.
Differential Diagnoses
- Long thoracic nerve palsy
- Myofascial pain syndromes.
- Whiplash injury
Diagnostic Work-up
High-resolution ultrasonography
It allows visualization of the normal spinal accessory nerve as well as changes after accessory nerve injury but actual transection is not readily visualized.
Electrodiagnostic tests
Nerve conduction studies reveal prolonged latencies in nerve injury. Electromyography would reveal signs of denervation or reinnervation [depends on the time since injury].
Electrodiagnostic tests can be used in the monitor recovery of function, plan a physical therapy and for intraoperative identification and preservation.
Contributing nerve supply from the cervical plexus to the trapezius muscle may result in results in some retained motor function after injury and making the diagnosis difficult.
Treatment of Spinal Accessory Nerve Injury
Conservative Treatment
The patient can be managed conservatively when serial clinical examination shows an improvement in the shoulder function or electromyography indicates electrical regeneration.
It can also be considered when symptoms are mild and tolerable with minimal scapulohumeral dysfunction.
Medical treatment includes-
- NSAIDs
- Transcutaneous nerve stimulation
- Regional nerve-blocks with local anesthetics
These measures provide short-term relief from shoulder pain and improve function. But frequent injections may be required.
Rehabilitation includes orthosis and physical therapy.
Rehabilitation aims at improving range of motion and maintaining proper shoulder alignment by reducing the mechanical tension on the scapula and shoulder girdle.
This is done by orthosis that elevates and medializes the scapula and thus in effect reducing the functional deficit of the trapezius muscle. An orthosis also makes other muscles perform better.
Physical therapy consists of a range of motion and strengthening exercises.
These include elevation, external rotation, and internal rotation exercises.
Physical therapy is vital to the long-term preservation of shoulder function and reduction of pain.
Surgical Treatment
The indications for spinal accessory nerve repair are as follows
- Iatrogenic intraoperative transection of the nerve [Immediate treatment]
- Delayed diagnosis with substantial shoulder symptoms
- Known spinal accessory nerve palsy with no improvement conservative management as evidenced by serial clinical examinations or EMG
- Severe paralysis
The surgical options are as follows:
- Neurolysis
- Nerve repair with or without graft [up to 20 months after injury]
- Eden-Lange muscle transfer [after 20 months]
Neurolysis
This procedure involves freeing the nerve of any fibrosis or other compressive structure
- When there is no anatomical break in continuity of the nerve
- Conduction of electrical impulses is present.
- Intraoperative nerve conduction studies aid in the identification of functional nerve fascicles.
Nerve repair
If the nerve is continuity and there is no electrical transmission on stimulation, resection of the scar or neuroma is done followed by a primary end-to-end anastomosis.
Nerve grafts are used if primary repair causes unacceptable tension.
The nerve graft could be autologous taken from nerves like greater auricular or sural nerves etc.
Vascularized grafts may also be used.
Alternatively, synthetic nerve guides or conduits may be used.
Allografts with temporary recipient immunosuppression have also been reported to be effective.
For gaps >3cm, cable grafts are recommended.
Longer grafts are associated with worse outcomes.
Eden-Lange procedure
Eden Lange procedure is a muscle transfer procedure indicated for
- >20 months after injury
- Failed nerve repair
- Irreparable nerve injury
- Primary trapezius pathology
The procedure stabilizes the scapula is by transferring the levator scapulae and rhomboid muscles to more lateral scapular targets.
After transfer, contraction of muscles stabilizes the scapula, particularly during abduction and anterior flexion of the shoulder.
References
- Chandawarkar RY, Cervino AL, Pennington GA. Management of iatrogenic injury to the spinal accessory nerve. Plast Reconstr Surg. 2003 Feb. 111(2):611-7; discussion 618-9.
- Ozdemir O, Kurne A, Temucin C, et al. Spontaneous unilateral accessory nerve palsy: a case report and review of the literature. Clin Rheumatol. 2007 Sep. 26(9):1581-3.
- Maldonado AA, Spinner RJ. Lateral pectoral nerve transfer for spinal accessory nerve injury. J Neurosurg Spine. 2017 Jan. 26 (1):112-5.
- Donner TR, Kline DG. Extracranial spinal accessory nerve injury. Neurosurgery. 1993 Jun. 32(6):907-10; discussion 911.
- Park SH, Esquenazi Y, Kline DG, Kim DH. Surgical outcomes of 156 spinal accessory nerve injuries caused by lymph node biopsy procedures. J Neurosurg Spine. 2015 Oct. 23 (4):518-25.