Last Updated on October 28, 2023
Brachial plexopathy is an affection of brachial plexus. Plexopathy refers to a disorder affecting nerves, blood or lymph vessels in the regions of the brachial or lumbosacral plexus, the two major plexus in the body.
The symptoms of plexopathy include pain, loss of motor control, and sensory deficits.
It should be kept in the mind that the clinical presentation of cervical radiculopathies could often be confused with brachial plexopathies. A detailed clinical examination, nerve conduction studies, and electromyography can help to differentiate.
Anatomy of Brachial Plexus
Brachial plexus is a complex interconnected network of nerves in the neck formed by contributions from C5 to T1 which divide reconnect and form peripheral nerves.
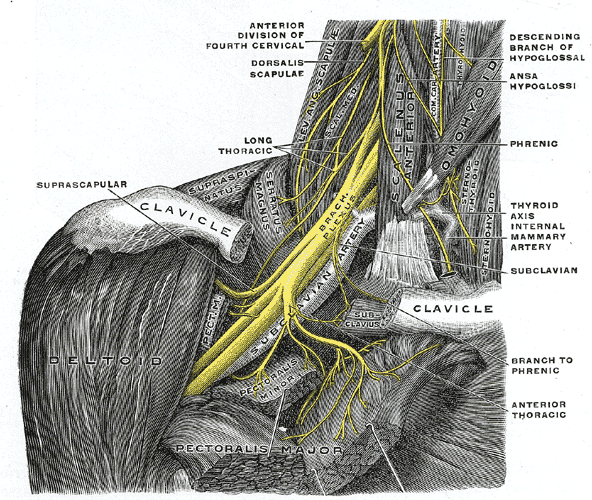
The complex arrangement is shown below.
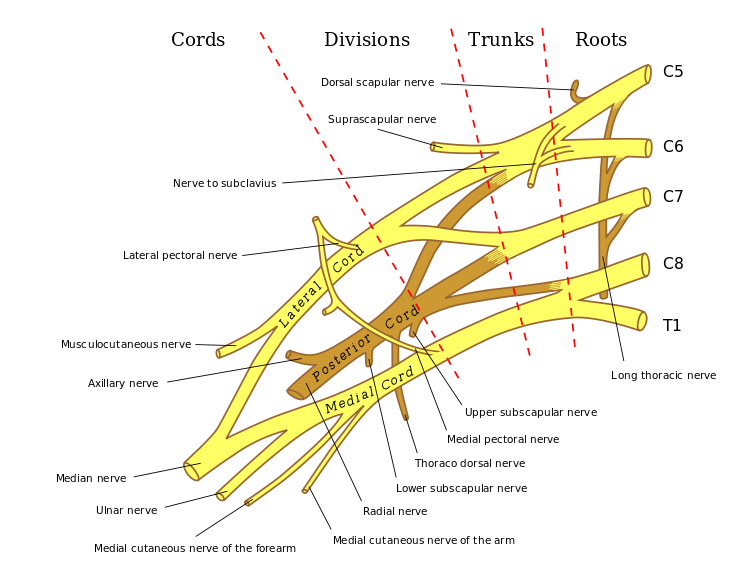
Read more on Brachial plexus anatomy
Brachial plexopathy can be caused by a variety of disorders affect the brachial plexus [neural, vascular, lymphatic]. Important causes of brachial plexopathy are discussed below
Idiopathic Brachial Neuritis or Parsonage-Turner syndrome
Idiopathic brachial neuritis is a disorder of unknown cause with asymmetric involvement of the brachial plexus. It commonly occurs between the third and seventh decade affecting men more than women.
Different events occurring days or weeks prior to the onset have been
- Upper respiratory infection
- Flu-like illness
- Immunization
- Surgery
- Emotional stress
No triggers can be found in half of the cases.
The condition is commonly seen in athletes participating in such as wrestling, weight lifting, and gymnastics.
Parsonage-Turner syndrome is thought to be an immune-mediated disorder [ suggested by demonstration of antiganglioside antibodies in serum and multifocal mononuclear infiltrates in brachial plexus biopsies.]
The typical presentation is acute sharp, stabbing or throbbing intense pain in regions of the shoulder, trapezius ridge, scapular area, upper arm, forearm, or hand. Few patients do not go through the painful stage.
The pain lasts from a few hours to weeks. A minority of the patients do not experience the initial painful stage.
After the pain goes, there develops a weakness of shoulder girdle and arm and progresses over few days.
Deltoid, supra and infraspinatus, serratus anterior, and biceps are commonly affected muscles. The muscles get wasted rapidly. Often one or more muscles in the same root distribution are spared.
The sensory deficit is not as pronounced as the motor deficit.
Sometimes, the lesions involve individual peripheral nerves such as the axillary nerve, the suprascapular nerve, and the anterior interosseous nerve.
Diaphragmatic involvement is seen in few cases. [Phrenic neuropathy may also be a part of the brachial neuritis spectrum]
Bilateral affection is seen in about thirty percent.
Electrophysiological studies help in the confirmation of diagnosis, the extent of the lesion, and prognostication. MRI findings range from normal to mild thickening of the plexus.
Most of the patients recover well.
Patients often require analgesic drugs for relief of pain. The pain can be severe in some patients, requiring a combination of agents and, at times, requiring opioid derivatives.
Corticosteroids have been used regularly in the management enough evidence is not available. IV immunoglobulin has been tried but again, a significant evidence is lacking.
Immobilization followed by physical therapy and range of motion exercises are carried. Exercises include strengthening of the rotator cuff muscles and scapular stabilization.
Nerve grafting or tendon transfers may be considered to improve shoulder abduction when recovery is not present.
Recurrence is rare.
[Read more on Parsonage-Turner Syndrome]
Idiopathic Hypertrophic Brachial Neuritis
It is an uncommon disease that progressively affects brachial plexus over months to even years.
It is characterized by slowly progressive weakness and wasting of the segments affected by the disease. Motor disability is overwhelming and sensory findings, when present, are mild.
This condition is painless from the beginning.
Nerve conduction studies and electromyography shows show demyelinating features [ not seen in idiopathic brachial neuritis].
Enlargement of the brachial plexus may be seen on MRI.
Hereditary Neuralgic Amyotrophy
It is an autosomal-dominant disorder characterized by repeated episodes of severe pain followed by paralysis and sensory disturbances in an affected limb.
The onset of is at birth or later in childhood. The recovery generally occurs after an attack but repeated attacks may leave with neurological deficit.
The episodes are triggered by infections, immunizations, surgery, delivery of a child, and stress.
The frequency of the episodes tends to decrease with age.
The individuals accumulate residual problems, such as chronic pain and impaired movement, over the time.
In some hereditary lineage, there are characteristic dysmorphic facial features like hypotelorism, epicanthal folds, long narrow face, facial asymmetry, cleft palate etc along with neck and forearm skin folds or creases and syndactyly
Cranial nerves are frequently involved in hereditary neuralgic amyotrophy.
Electrophysiological studies show normal or mildly reduced motor nerve conduction velocities distal to the affected brachial plexus. Pathological studies have found mild focal axonal degeneration in nerves examined distal to the plexus abnormality.
Neurogenic Thoracic Outlet Syndrome
Thoracic outlet syndrome is characterized by pain, paresthesias, and weakness in the upper extremity.
Cervical rib, enlarged C7 transverse processes, fibrous bands are major causes of this.
Pain, paresthesias or weakness in the upper extremity are common symptoms. Paresthesias may affect the ring and small fingers. Symptom severity tends to increase after certain activities and worsens at the end of the day or during sleep.
There is a weakness of the hand, loss of dexterity of the fingers, and atrophy of the affected muscles.
Provocative tests are used to ascertain the diagnosis. These tests are
Adson Test
- Extension of the neck with a rotation of the head toward the involved extremity, which is held in an extended position at the side.
- Maneuver constricts the interscalene triangle.
- Change in the radial pulse when the patient inhales deeply and holds his/her breath means positive
Wright test
- The patient places the arm in full abduction and external rotation
- Leads to constriction of the costoclavicular space.
- Positive if typical symptoms are elicited along with detection of a change in pulse.
Elevated Arm Stress Test (Roos test)
- The patient keeps the affected arm in full abduction and external rotation
- The patient is asked to open and close fists slowly over 3 min
- Causes constriction of the costoclavicular space.
- Positive if typical symptoms are produced and the patient is unable to sustain the maneuver for the full 3 min
X-rays and MRI are helpful in diagnosis.
Electrodiagnostic tests show the absent or reduced amplitude of sensory and motor nerve action potential in ulnar or median nerves.
Needle electromyography which shows denervation in at least one muscle supplied by each of two different nerves from the lower trunk of the brachial plexus with normal cervical paraspinal muscles.
conservative treatment includes modification of activities, postural exercises, physical therapy [Strengthening and stretching exercises] and anti-inflammatory drug therapy.
If there is no response to conservative treatment within 6 weeks, or if time loss extends longer than 2 weeks, surgical treatment may be considered.
Metastatic Brachial Plexopathy
The condition is more common in the elderly patients. Lung and breast cancers most commonly metastasize to brachial plexus reaching by direct extension or through the lymphatics from the axilla. Lymphoma, sarcoma, and melanoma are less common but associated.
The characteristic feature of metastatic plexopathy is severe pain in the shoulder girdle radiating to the inner aspect of the upper limb.
The lower trunk is preferentially involved due to the proximity of draining lymph nodes.
MRI can identify the mass adjacent to the plexus and encroachment of epidural space.
Treatment is often difficult and palliative in form of radiotherapy and chemotherapy of the underlying tumor.
Radiation-Induced Brachial Plexopathy
Radiation therapy to the chest, neck or axillary region for the underlying tumor may result in brachial plexopathy. Radiation dose > 6000 cGy are more likely to develop.
Breast carcinoma is most commonly associated followed by lung carcinoma and lymphoma.
Limb paresthesia, swelling, and motor weakness are common presenting complaints though pain is an inconsistent feature. Radiation-induced brachial plexopathy has a predilection for the upper trunk and not for the lower trunk, probably secondary to the protective effect of the clavicle and relatively shorter course of the lower trunk through the radiation port.
MRI may show thickening and diffuse enlargement of the brachial plexus without the focal mass. Nerve conduction studies may show features of demyelinating conduction blocks. EMG show spontaneous activity in the form of myokymic discharges.
Prognosis is not good. Palliative care is offered. Lymphatic bypass surgery to relieve lymphedema may rarely be needed.
Traumatic Brachial Plexopathy
Traumatic brachial plexopathy usually result from a motor vehicle accident especially in motorcycles, fall from a significant height, penetrating injuries and gunshot wounds, and iatrogenic injury [nerve block administration].
Upper plexus injuries are commonly injured if the arm is at the side [because the first rib acts as a fulcrum to direct the traction forces preferentially in line with the upper plexus]. The lower plexus lesion predominates when the arm is abducted and raised overhead violently [ because the coracoid acts as a fulcrum in a similar fashion.]
MRI can differentiate between pre-ganglionic injuries [root avulsion], pseudomeningocele and post-ganglionic lesions [ enhancing nodular thickening (neuroma) and hematoma in the vicinity of the plexus]
In an acute situation, the patient is put on symptomatic treatment. Once the general condition of the patient is stabilized, reassessment of neurological deficit is carried out.
Primary nerve reconstruction, joint fusion and tendon transfers alone or in combinations are used in the recovery of functions in many patients.
[Read more on Traumatic Brachial Plexopathy]
References
- Suarez GA, Giannini C, Bosch EP, Barohn RJ, Wodak J, Ebeling P, et al. Immune brachial plexus neuropathy: Suggestive evidence for an inflammatory-immune pathogenesis. Neurology. 1996;46:559–61.
- van Eijk JJ, van Alfen N, Tio-Gillen AP, Maas M, Herbrink P, Portier RP, et al. Screening for antecedent Campylobacter jejuni infections and anti-ganglioside antibodies in idiopathic neuralgic amyotrophy. J Peripher Nerv Syst. 2011;16:153–6.
- Martínez-Salio A, Porta-Etessam J, Berbel A, Alonso A, Gutiérrez-Rivas E, Trueba J. Amyotrophic neuralgia: Review of 37 cases. Rev Neurol. 1998;27:823–6.
- McCarty EC, Tsairis P, Warren RF. Brachial neuritis. Clin Orthop Relat Res. 1999:37–43
- Todd M, Shah GV, Mukherji SK. MR imaging of brachial plexus. Top Magn Reson Imaging. 2004;15:113–25.
- Rovak JM, Tung TH. Traumatic brachial plexus injuries. Mo Med. 2006;103:632–6.
- Rohde RS, Wolfe SW. Nerve transfers for adult traumatic brachial plexus palsy (brachial plexus nerve transfer) HSS J. 2007;3:77–82