Last Updated on June 9, 2022
Synovial fluid analysis is often done to aid in the diagnosis of joint inflammation, pain, swelling, and/or fluid accumulation. It is withdrawn from the joint by a procedure called arthrocentesis.
Synovial fluid is a thick, stringy fluid found in the cavities of synovial joints. It reduces friction between the articular cartilage and other tissues in joints by lubricating and cushioning them during movement.
During movement, the synovial fluid held in the cartilage is squeezed out mechanically to maintain a layer of fluid on the cartilage surface. Normal synovium contains synovial lining cells that are 1-3 cells deep. Synovium lines all intracapsular structures except the contact areas of articular cartilage. 
The major difference between synovial fluid and other body fluids derived from plasma is the high content of hyaluronic acid in synovial fluid. The normal viscosity of the synovial fluid is due to the hyaluronic acid.
Functions of Synovial Fluid
Synovial fluid aids in the nutrition of articular cartilage by acting as a transport medium for nutritional substances, such as glucose, and provides lubrication of the articulating surfaces.
Secretion of Synovial Fluid
The synovial lining cells reside in a matrix rich in type I collagen and proteoglycans. There are two main types of synovial lining cells, but these can be differentiated only by electron microscopy.
- Type A cells are macrophage-like and have primarily a phagocytic function.
- Type B cells are fibroblast-like and produce hyaluronate, which accounts for the increased viscosity of synovial fluid.
Other cells found in the synovium include antigen-presenting cells called dendritic cells and mast cells.
Synovial tissue also contains fat and lymphatic vessels, fenestrated microvessels, and nerve fibers derived from the capsule and periarticular tissues.
Hyaluronic acid, synthesized by synovial lining cells (type B), is secreted into the synovial fluid, making the fluid viscous.
Composition of Synovial Fluid
Synovial fluid is made of hyaluronic acid and lubricin, proteinases, and collagenases.
The normal synovial fluid contains 3-4 mg/ml hyaluronan (hyaluronic acid), a polymer of disaccharides composed of D-glucuronic acid and D-N-acetylglucosamine joined by alternating beta-1,4 and beta-1,3 glycosidic bonds.
Synovial fluid also contains lubricin secreted by synovial cells. It is chiefly responsible for so-called boundary-layer lubrication, which reduces friction between opposing surfaces of cartilage. It may also have a role in synovial cell growth.
Vascular permeability and synovial membrane permeability are altered by inflammation, which accounts for protein content changes in the diseased synovial fluid. Immunoglobulins, immune complexes, and complement are produced by cells accumulating in the inflamed synovial membrane and periarticular lymph nodes and find their way to the synovial fluid.
Normal synovial fluid complement levels in humans are approximately 10% of the serum values. In the inflamed joint synovial fluid complement levels will vary.
Cell counts of canine synovial fluid vary from joint to joint but normally are low. Lymphocytes, monocytes, and neutrophils are also present normally, while macrophages are seen only occasionally. In pathologic fluids, chondrocytes, osteoblasts, and osteoclasts may be seen. Fragments of articular cartilage may contain chondrocytes within lacunae. The exposed subchondral bone may give osteoblasts and multinucleated osteoclasts access to the synovial fluid.
Erythrocytes are rarely seen in the normal joint fluid. Their presence usually indicates contamination of the sample by peripheral blood at the time of aspiration
Physical Characteristics of Normal Synovial Fluid
- Normal synovial fluid is clear, pale yellow, viscid, and does not clot.
- Amount – thin film covering surfaces of synovium and cartilage within joint space
- Cell count – <200/mm3 . Less than 25 percent are neutrophils
- Protein – 1.3-1.7 g/dl (20 % of normal plasma protein)
- Glucose – within 20 mg/dl of the serum glucose level
- Temperature – 32 degree Celsius (peripheral joints are cooler than core body temperature)
- String sign (a measure of viscosity) – 1-2 inches
- When a drop is taken between the thumb and finger as in pinching and then they are separated, the drop forms a string till 1-2 inches
- pH – 7.4
Examination of Synovial Fluid
Collection of fluid is done without adding an anticoagulant, except a few milliliters for a cytologic study to which is added 2 mg potassium oxalate per milliliter of fluid.
Gross Appearance
Note the color, turbidity, apparent viscosity, and tendency to clot. Blood streaks are caused by needle puncture. The viscosity may be estimated by allowing the fluid to drip from the end of a small syringe. Normally, the viscous fluid falls drop by drop. The thin, nonviscous fluid of inflammation flows freely and uninterruptedly.
As needed following studies may be conducted on the synovial fluid
Bacterial studies
Culture is done at the bedside and should include guinea pig inoculation.
Cytology
For a total cell count, saline is used as a diluent, since routine diluents contain an acid that will precipitate the mucin. Methylene blue is added to the saline to stain the nucleated cells. A standard hemacytometer is used.
The differential count is done on very thin dried smears stained with Wright’s stain. The mucinous amorphous deposit stains deeply basophilic.
In traumatic joint disease, the total cell count varies from a normal of 60 to 3000, seldom higher, and consists mainly of mononuclear cells. In inflammatory joint disease, the total count is above 3000, mainly of mononuclear cells. In inflammatory joint disease, the total count is above 3000, mainly polymorphs. One must be cautious in interpreting the fluid in mild rheumatoid arthritis, since this may resemble that of traumatic arthritis.
Sugar
The concentration of sugar in synovial fluid is the same as that in the blood. Values are normal in traumatic arthritis and reduced in rheumatoid and infectious arthritis,
Protein
In traumatic fluid, the total protein does not rise above 5.5 g/dl, and the albumin fraction determined electrophoretically is more than 60% of the total. In rheumatoid arthritis, the total protein may rise above 8 g, with a proportionately higher amount of globulin, so that the albumin concentration is lower, often below 50%.
What is Synovial Fluid?

The synovial fluid or joint fluid is present in all joints or diarthroses. The articular surfaces of the synovial joints are covered by articular cartilage and are separated from each other by a small cavity that contains the synovial fluid.
The synovial joint has a joint capsule which contains specialized secretory cells termed synoviocytes (types A and B). These produce the components of the synovial fluid and contribute to the local production of cytokines, small-molecule mediators of inflammation, and proteolytic enzymes.
Synovial fluid also provides nutrients and lubrication for the joints.
Biochemically, the synovial fluid is an ultrafiltrate of plasma.
In normal physiological conditions, the biochemical composition of the synovial fluid is similar to that of plasma.
This composition changes in various diseases and results in gross, microscopic, biochemical and cytological changes in the fluid. These changes can be analyzed and information can be deduced from the values generated in the analysis.
Typical characteristics of synovial fluid
Physical characteristics
- Appearance – clear
- Viscosity – high
- Moderately viscous – drops of it from a syringe needle will form a “string” a few inches long.
Chemical Analysis
- A small amount of glucose and protein.
- Glucose level is similar to that of the patient’s serum glucose level
Microscopic examination
- Few white blood cells (WBCs< 200/ µL) and red blood cells
- No microbes or crystals present
- Polymorphonuclear neutrophils (PMNs< 25% )
Pathologies Affecting Joints – Indications for Synovial Fluid Analysis
Diseases and conditions affecting joint(s) and the synovial fluid can be divided into four main categories:
Infections
These could be caused by bacteria, fungi, or viruses. Infection of the joint results in acute and chronic septic arthritis.
Bleeding
Bleeding disorders and/or joint injury can lead to blood in the synovial fluid
Inflammatory diseases
- Conditions that cause crystal formation and accumulation such as gout and pseudogout
- Conditions that cause joint inflammation, such as synovitis, or other immune responses. These may include autoimmune disorders such as rheumatoid arthritis and lupus.
Degenerative diseases
Osteoarthritis
Collection of Synovial Fluid
Synovial fluid is collected via arthrocentesis or joint aspiration. The collected volume depends on the size of the joint and the necessary tests. Normal joint contains few ml of joint fluid but this quantity increases in the presence of inflammation.
Depending on the test, different types of preservatives are required, as follows:
- Sterile heparinized tubes for microbiology testing
- Heparinized or EDTA tubes for cell count
- Without preservatives for most chemistry tests
- NaF for glucose testing
Powder preservatives or powdered gloves should not be used for sample collection as they can introduce particulates that could interfere with the synovial crystal analysis
Synovial Fluid Analysis – Abnormalities and Interpretation
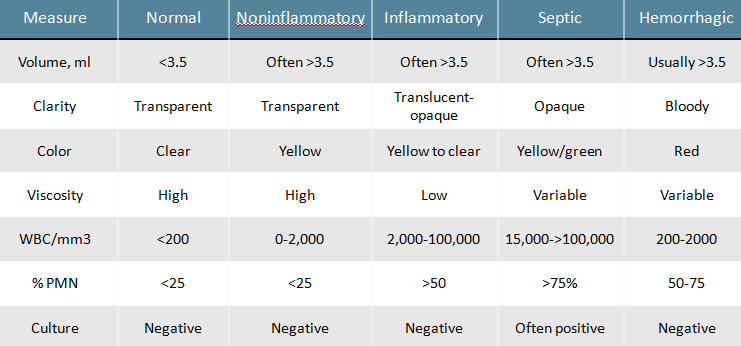
Lab evaluation of synovial fluid involves the following three steps
- Physical examination like appearance, color, viscosity etc
- Chemical analysis like glucose, total protein level, uric acid etc
- Microscopic evaluation like cell count and differential count, crystal identification etc
Additionally, microbiologic, serologic, and cytologic laboratory evaluations can be done.
Changes in the appearance of synovial fluid
Changes in the physical characteristics may provide clues to the disease present, such as:
- Decreased viscosity may be seen with inflammation. Viscosity decreases because of decreased production and polymerization of hyaluronic acid. A string 4-6 cm of synovial fluid between the tips of the fingers is normal.
- Cloudy synovial fluid may indicate the presence of microbes, white blood cells, or crystals.
- Reddish synovial fluid may indicate the presence of blood.
- Inflammatory diseases of nonimmunologic origin: Cloudy/turbid, dense yellow with crystals
- High number of crystals are present: Milky/cloudy
Changes in the biochemical composition of synovial fluid
In normal circumstances, the concentration of most of the analytes of synovial fluid is the same as that in serum.
For accurate interpretation of synovial fluid laboratory results, serum samples should be concomitantly evaluated.
Glucose is significantly decreased in inflammatory conditions. These include
- Immunologic disorders
- Lupus
- Scleroderma
- Crystal-induced arthropathies [gout and pseudogout]
- Rheumatoid arthritis
- Septic arthritis
Samples used for glucose evaluation should be collected in NaF [sodium fluoride] tubes to prevent rapid glycolysis and should be tested within 1 hour after collection. Otherwise, a falsely decreased glucose concentration is obtained.
Total protein concentration in synovial fluid is lower than in serum, usually one-third of that in serum. However, this concentration increases in inflammatory and hemorrhagic disorders.
Presence of increased uric acid indicates gout and confirmation is done by a high number of uric acid crystals in synovial fluid.
Cell counts in synovial fluid analysis
Increased WBC count [normal 200 cells/µL] indicates infections/inflammation. Gram stain and culture can be used for differential diagnosis.
- Total cell counts— the number of WBCs and RBCs in the sample Increased WBCs are seen in infection and in conditions such as gout and rheumatoid arthritis.
- Increased number of neutrophils – bacterial infections.
- > 2% eosinophils may suggest Lyme disease, parasitic arthritis, rheumatoid disease, or tubercular arthritis.
Microscopic evaluation of crystals in synovial fluid
- Monosodium urate
- In gout
- Crystals needle-shaped
- Negative/yellow birefringence in the compensated polarized light.
- Calcium pyrophosphate (CPP) crystals
- Pseudogout
- Rhombic-shaped
- Positive/blue birefringence in the compensated polarized light.
- Cholesterol crystals
- In hyperlipoproteinemia and rheumatoid arthritis
- Rhombic and have negative/yellow birefringence in the compensated polarized light.
- Corticosteroids crystals
- Seen in patients treated with intra-articular injections of corticosteroids.
- Flat, small, and have different shapes
- Can have both positive/blue and negative/yellow birefringence
- Calcium phosphate crystals [apatite]
- Degeneration and calcification of cartilage and osteoarthritis.
- Coffin-lid shaped
- No birefringence
- Calcium oxalate crystals
- In renal diseases or dialysis.
- Envelopes or pyramid shaped
- Negative/yellow birefringence
Further Lab Studies for Infection
When infection is suspected, the synovial fluid may be subjected to special investigations. These are
Gram stain
This involves staining the smear of the fluid on the slide with Gram’s stain and direct observation of bacteria or fungi under a microscope.
Normally, there should be no microbes present in synovial fluid.
Culture and Sensitivity
To determine the type of microbe and its susceptibility to different drugs.
AFB Staining and Culture
To investigate the presence of tuberculosis. Molecular tests like PCR are also methods for Mycobacteria tuberculosis detection.