Last Updated on October 29, 2023
Congenital pseudarthrosis of tibia is an uncommon disease with clinical presentations ranging from simple anterolateral tibial angulation to complete non-union with extensive bone defects. It is a rare disease, with an estimated frequency of 1/150,000 births. Pseudarthrosis means false joint. A relationship with type 1 neurofibromatosis or von Recklinghausen’s disease is known but exact pathophysiology has still not been clearly defined.
The disease becomes evident within a child’s first year of life though late presentations are known.

Image curtsy: Radiopaedia
Pathophysiology of Congenital pseudarthrosis of the Tibia
The affected tibia has abnormal fibrovascular tissue grows, replacing the bony cortex. It is called fibrous hamartoma and it promotes osteoclastic bone resorption. This leads to insufficient mechanical strength and poor osteogenetic potential at the site.
Reactive changes occur at medullary aspect leading to deposition of excess trabecular bone which is visible as medullary sclerosis on x-ray.
The cuff of fibrous tissue or fibrous hamartoma is in continuity with abnormal periosteal thickening. Fibrous hamartoma has low osteogenic [bone forming] and high osteoclastic [bone resorbing] activity.
The soft tissue at the pseudarthrotic site is composed of fibrous tissue, fibrocartilage, and hyaline cartilage with evidence of enchondral ossification. Spaces and clefts are lined by a synovial-like tissue. Within the bone ends, marrow spaces are devoid of hematopoiesis.
This tissue causes compression, osteolysis, and persistence of pseudarthrosis. Resorption lacuna with giant osteoclasts are present at the pseudarthrosis-bone junction [Intracortical cysts] are found more in younger children.
Fibrous hamartoma and of the pathological periosteum also contribute to the prevention of union by mechanical interposition. The periosteum could create a fibrous band causing an increase in local pressure around the bone resulting in reduced vascularization. The vascularization defect could also be secondary to thickening of the vessel walls in the area of pseudarthrosis.
The ultrastructural findings in the abnormal periosteum are similar to skin neurofibromas of neurofibromatosis patients. This indicates a pathogenetic association of both diseases.
The composition of the pseudarthrotic tissue seems to be identical whether or not it is associated with NF1. The physiopathology of congenital pseudarthrosis of tibia could, therefore, be identical, irrespective of the association with neurofibromatosis 1.
40–80% with congenital pseudarthrosis of the tibia are neurofibromatosis 1 carriers.
Clinical Presentation
Bowing may be discovered during a clinical examination at birth or in the first weeks of life.
The bow in tibia is anterolateral. Severe cases present a discontinuity between the two segments. The clinical presentation varies considerably, from simple bowing to pathological fracture and pseudarthrosis.
The severity of shortening in the leg also varies.
Normally the disease is unilateral, located at the junction of the middle and distal thirds of the tibial segment. There is no predominance for sex. There is no predilection of side too.
The fibula is also affected in more than half of the cases.
Differential Diagnosis
Isolated congenital pseudarthrosis of tibia needs to differentiated from bone anomalies associated in neurofibromatosis 1. The latter is a multisystemic neurocutaneous disease with an autosomal dominant pattern and an estimated frequency of 1/4000 births.
Other differential diagnoses are
- Fracture non-union
- Failed bone graft
- Ehlers-Danlos syndrome
- Osteogenesis imperfecta
- Fibrous dysplasia
- Ochronosis
Imaging
X-ray
Depending upon the severity of the condition, x-rays show simple convex anterolateral bowing to true tibial discontinuity with resorption of the two ends of the fracture.
In cystic form the cortices are continuous and thickened in the concave side of the bow, medullary canal is narrow and an image of a cyst can be seen at the apex of the curvature. The deformity gradually worsens until a transverse fracture occurs. In cystic forms, bowing appears at between 6 weeks and 1 year.
In dysplasic forms, the bowing is visible at birth and sometimes pseudarthrosis may already be present.
The tibia is narrow with an hourglass appearance and the medullary cavity is partially or completely obstructed.
The fibula is frequently affected in these types.
When pseudarthrosis has developed, the ends of the bone may be thin, atrophic or on the other hand, wide and hypertrophic.
This false joint is often in the distal third of the shaft but can occur at any level. The fibula can be frequently affected
MRI
MRI provides a more detailed analysis of both bone and especially soft tissue lesions. It is helpful for the preoperative planning in that the borders for resection can be defined precisely.
Computed tomography scan
Computed Tomography scan usually confirm radiographic findings, showing osteolytic lesions containing solid tissue. The lesion can be delineated by a sclerotic rim.
Total bone scintigraphy
At the level of the pseudarthrosis – a slight uptake at the beginning of the dynamic venous phase and a high uptake during the terminal phase.
Classification of Congenital Pseudarthrosis of Tibia
Various classification systems based on radiographic finding have been developed.
Andersen’s classification
Cystic, Dysplastic and Sclerotic
Crawford Classification
It is the most frequently used classification today. It is descriptive and identifies the different stages of progression.
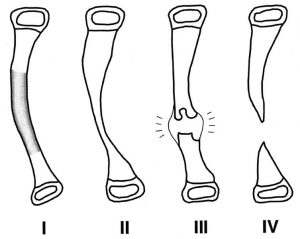
Image credit: JBJS
Type I
Anterior bowing with an increase in cortical density and a narrow medulla
Type II
Anterior bowing with narrow, sclerotic medulla,
Type III
Anterior bowing associated with a cyst or signs of a prefracture.
Type IV
Anterior bowing and a clear fracture with pseudarthrosis often associating the tibia and fibula;
Boyd Classification
It has six types and provides prognostic value
Type I
Anterior bowing associated with other congenital malformations
Type II
- Anterior bowing with an hourglass appearance to the tibia
- Fracture usually occurs before the age of 2.
- The ends of the bone are thin, rounded and sclerotic with obliteration of the intramedullary canal.
- Often associated with NF1
- Poor prognosis with frequent recurrence
Type III
- Pseudarthrosis developing from an intraosseous cyst
- Anterior bowing can precede or follow the development of the fracture
- High rate of union and rare recurrence
Type IV
- Sclerotic bone with no pathological bowing.
- Medullary canal is partially or completely obliterated.
- Fatigue fracture may occur and progress to pseudarthrosis.
- Good prognosis with treatment before fatigue fracture
- The prognosis is good if treated before the fatigue fracture occurs,
Type V
- Dyplasic appearance to the fibula
- Pseudarthrosis can be located on either of the two bones of the tibial segment.
- The prognosis is good if the lesion is located only on the fibula, an extension to the tibia has a prognosis similar to type II,
Type VI
- Associated with an intraosseous fibroma or a schwannoma.
- Prognosis depends on how aggressive is the intraosseous lesion.
Treatment of Congenital Pseudarthrosis of Tibia
Treatment of congenital pseudarthrosis of the tibia is surgical. In its natural progression, the deformity and shortening worsen.
As the child is not operated before he reaches a certain age, wearing a protective brace before the child has begun walking delays the fracture in bowing and limits the deformity if pseudarthrosis is already present.
The aims of surgical treatment are
- Union at the pseudarthrosis site
- Restoration of alignment
Surgery for CPT should preferably be postponed until the age of 5 years and should not be performed on patients under the age of 3 years. This is because of the difficulty of stabilizing small bone fragments in younger children.
Associated pseudarthrosis or hypoplasia of the fibula is seen in two-thirds of the cases. Yet the need for fibular surgery remains controversial.
Surgical Treatment Options
Intramedullary nailing and Bone Grafting
It involves resection of areas of pseudarthrosis, intramedullary fixation, and grafting. The use of a telescopic nail or pins helps protect the reconstructed area during growth and avoids having to change the internal fixation. A rate of union of more than 80% has been reported.
Ankle pain and stiffness, Pes cavus and/or valgus and residual leg length discrepancies are reported complications.
Vascularized bone transfers
This involves wide resection of the dystrophic tibia and augmentation with a vascularized graft. Vascularized graft means the graft has its own blood supply and is not dependent on host site circulation for survival, thus enhancing the results. The contralateral fibula is mostly used for the purpose of graft though fibula of the same side has also been used with success.
The graft is fixed by screwing or pinning with and without external fixation.
The rate of primary union of vascularized transfers is more than 70%. The success rate increases with the patient’s age.
In 30% of cases, secondary bone grafting is necessary to obtain bone union.
Valgus ankle deformity on the donor side, re-fracture in the graft itself, recurrent nonunion at one end of the graft site and residual limb-length discrepancy are the known issues.
If the procedure is combined with intramedullary nailing, it prevents re-fracture rate significantly.
External fixation
Circular external fixation or Ilizarov ensures stability, allows correction of axial deformities, and allows lengthening procedure to be done if required.
Thus it can correct deformities of leg and ankle and limb length discrepancy simultaneously. It especially good in cases with small bone fragments.
But it is cumbersome, complex and associated with a high risk of infection.
The rate of union varies from between 50 and 90%
Graft Adjuvants and Orthobiologics
These methods, when used along with conventional procedures, stimulate the bone healing process. The efficiency of novel biological treatments still has to be demonstrated.
Bone Morphogenetic Proteins
Two recombinant human osteogenic proteins have been described.
BMP-2 acts earlier on the proliferation and differentiation of mesenchymal cells into chondroblasts while BMP-7 acts on osteoblast differentiation.
Induced membrane and spongy autologous graft
In the first stage, a cement spacer in fills the defect to be reconstructed associated with stable internal fixation. In the second surgery, the spongy autologous graft is put after removing the cement spacer.
Periosteal grafts
This technique involves complete resection of the diseased periosteum around the area of pseudarthrosis, which is replaced with a periosteal graft harvested from the iliac wing which covers the resected area after placement of a bone graft and intramedullary tibular and fibular internal fixation.
Autologous and bone marrow grafts
Under research, the capacity of bone marrow cells to differentiate into osteoblastic cell lines could be enough to justify its use in the treatment of CPT.
Bone Stimulators
- Ultrasound
- LIPUS
- Electrostimulation
Amputation
When extensive surgical procedures have not achieved a functional extremity, the pseudarthrosis is resistant. This kind frequently encounters persistent nonunion, dysfunctional angular deformity, shortening, atrophy, and stiffness.
Such cases are appropriately treated by amputation. While waiting for surgery, tibial alignment should be maintained with an orthosis to allow child walk, run, and socialize.
Evaluation of Results of Treatment
Johnston has suggested a method of rating the results of treatment
Stage 1
Clear union with full normal function during full weight-bearing;
Stage 2
- Incomplete union with useful function but a protective brace is needed;
- X-rays show a transverse cortical or longitudinal defect and/or frontal or sagittal deformity of more than 15° which may or may not be associated with shortening of more than 3 cm
Stage 3
Persistent pseudarthrosis or a recurrent fracture.
Complications
Valgus ankle
- Occurs in 45% of cases
- Due to proximal migration of the lateral malleolus
- Causes tibiotarsal joint instability
- Stresses lateral tibial epiphysis and causes asymmetric growth.
- Epiphysiodesis of the medial malleolus corrective
Ankle Stiffness
- Due to rigid immobilization
- Cause pain or foot deformities
Leg Length Discrepancy
- Shortening of the affected leg may occur
- < 5 cm – controlateral epiphysiodesis otherwise Ilizarov lengthening
Recurrent fractures
- Fracture may occur after union.
- Brace may be protective.
- Revision surgery may be necessary.
Prognosis
The association with neurofibromatosis was long considered to be a negative predictive factor but repeated studies have not found so.
Lower location [towards metaphyses], severe deformities with bone atrophy, extensive sclerotic lesions with a small diameter bone and significant shortening and associated fibular involvement have a poor prognosis.
Overall, the percentage of bone union varies between 31% and 100%. Healing rates were found to be higher when the pathological periosteum and fibromatous tissue were removed.
References
- Hefti F, Bollini G, Dungl P, Fixsen J, Grill F, Ippolito E, et al. Congenital pseudarthrosis of the tibia: History, etiology, classification, and epidemiologic data. J Pediatr Orthop B. 2000;9:11–5.
- Gutmann DH, Aylsworth A, Carey JC, Korf B, Marks J, Pyeritz RE, et al. The diagnostic evaluation and multidisciplinary management of neurofibromatosis 1 and neurofibromatosis 2. JAMA. 1997;278:51–7.
- Grill F, Bollini G, Dungl P, Fixsen J, Hefti F, Ippolito E, et al. Treatment approaches for congenital pseudarthrosis of tibia: Results of the EPOS multicenter study. J Pediatr Orthop B. 2000;9:75–89.
- Ohnishi I, Sato W, Matsuyama J, Yajima H, Haga N, Kamegaya M, et al. Treatment of congenital pseudarthrosis of the tibia: A multicenter study in Japan. J Pediatr Orthop. 2005;25:219–24.
- Toh S, Harata S, Tsubo K, Inoue S, Narita S. Combining free vascularized fibula graft and the Ilizarov external fixator: Recent approaches to congenital pseudarthrosis of the tibia. J Reconstr Microsurg. 2001;17:497–509.
- Kim HW, Weinstein SL. Intramedullary fixation and bone grafting for congenital pseudarthrosis of the tibia. Clin Orthop Relat Res. 2002;405:250–7.
- Dobbs MB, Rich MM, Gordon JE, Szymanski DA, Schoenecker PL. Use of an intramedullary rod for treatment of congenital pseudarthrosis of the tibia. A long term followup study. J Bone Joint Surg Am. 2004;86-A:1186–97
- Fabeck L, Ghafil D, Gerroudj M, Baillon R, Delince P. Bone morphogenetic protein 7 in the treatment of congenital pseudarthrosis of the tibia. J Bone Joint Surg Br. 2006;88:116–8.
- Guidera KJ, Raney EM, Ganey T, Albani W, Pugh L, Ogden JA. Ilizarov treatment of congenital pseudarthroses of the tibia. J Pediatr Orthop. 1997;17:668–74.
- Okada K, Miyakoshi N, Takahashi S, Ishigaki S, Nishida J, Itoi E. Congenital pseudoarthrosis of the tibia treated with low-intensity pulsed ultrasound stimulation (LIPUS) Ultrasound Med Biol. 2003;29:1061–4.