Last Updated on February 27, 2021
The ganglion impar is a sacrococcygeal ganglion, also called ganglion of Wather. It is a retroperitoneal structure located at the level of the sacrococcygeal junction.
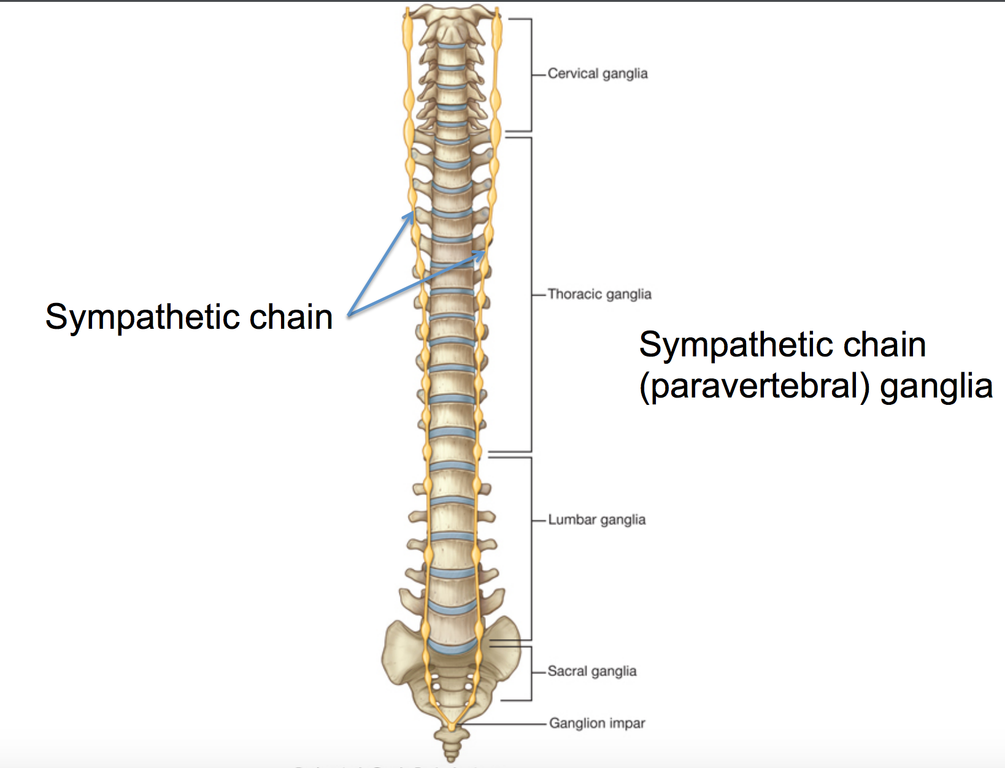
It is the final terminus of sympathetic chains formed by the fusion of both the chains.
Therefore, the ganglion impar block is used in patients with the pain in pelvic and perineal structures.
Relevant Anatomy
The ganglion impar is an irregularly shaped terminal ganglion of the sympathetic chain. It is located almost in the midline at the level of sacrococcygeal junction. It is of variable shape and can be located anywhere from the anterior surface of the sacrococcygeal junction to the lower coccygeal vertebral bodies.
The rectum is situated anterior to the ganglion. Fibers from the ganglion travel to the sacral spinal nerves along the gray rami communicantes.
This ganglion marks the end of the two sympathetic chains.
Visceral afferents from the perineum, distal part of the rectum, anus, distal end of the urethra, vulva, and distal third of vagina converge at the ganglion impar.
There is a wide range of variation in location of the ganglion.
Indications for Ganglion Impar Block
In orthopedics, ganglion impar block is used for coccydynia not amenable too other measures.
Other indications for this block are
- Intractable perineal pain
- Rectal/Anal pain (proctitis)
- Vulvar pain
- Vaginal pain [distal one-third]
- Postherpetic neuralgia
- Pain in complex regional pain syndrome
- Visceral pain
- Endometriosis
- Chronic prostatitis
Ganglion Impar Block
The classical technique was described by Plancarte and colleagues. Here, the patient is placed in lateral decubitus position with hips fully flexed.
A standard 22-gauge, 3.5-inch spinal needle is bent 1 inch from its hub to form a 30-degree angle. The needle is then introduced under local anesthesia through the anococcygeal ligament with its concavity oriented posteriorly, and under fluoroscopic guidance, it is directed along the midline at or near the sacrococcygeal junction.
A finger is placed in the rectum to avoid puncturing the structure.
A curved needle was later used instead of a bent needle. Spinal needle has also been advocated.

Technical difficulties and the procedure associated risks [needle break, rectal perforation] have made this approach unpopular.
Transcoccygeal approach is more commonly used now. This involves the placement a 20-gauge, 1.5-inch needle through the sacrococcygeal ligament under fluoroscopic guidance so that the tip of the needle is just anterior to the anterior portion of the sacrum, thus minimizing the risk of rectal perforation.
The transsacrococcygeal ligament needle-inside-needle is the most frequently used approach.
A needle-in-needle technique may avoid trauma to the disk and coccyx, in addition to decreasing needle breakage during the transcoccygeal approach
Imaging guidance markedly increased technical success rates. Fluoroscopy facilitated further development, including the transcoccygeal, transarticular, transdiscal, intracoccygeal, and paracoccygeal approaches.
Ultrasound-guided techniques provide the advantage of real-time visualization and avoidance of radiation.
There are four main anatomic approaches to consider when performing ganglion impar blocks:
Paracoccygeal approaches i.e., immediately to the right or left of the coccyx have also been described.
Ganglion Impar Block with Modified Needle-Inside-Needle Technique
- The patient is kept in a prone position
- Keep a pillow under the abdomen
- Allow flexion of the lumbosacral spine
- Allows internal rotation of lower limbs
- Prepare the skin of the area
- Use a local anesthetic to numb the skin over the insertion point using a 25-gauge needle over the sacrococcygeal disc
- Insert a 21-gauge, 1.5-inch needle through the sacrococcygeal disc under fluoroscopic guidance
- Serves as guide for the other needle
- Introduce a 25-gauge, 2-inch through the 22-gauge needle.
- Confirm the needle placement in the retroperitoneal space by contrast agent insertion [0.2-0.5]. The comma sign confirms the placement.
- For diagnostic block/prognostic block
- 1 to 3 mL of local anesthetic (lignocaine, ropivacaine or bupivacaine) is injected.
- For neurolysis
- 1- 2 mL of a neurolytic agent [ 99% alcohol, phenol]
- Given 20 to 30 minutes after the diagnostic block.
It is important that if pa atient complains pain with the neurolytic agent, the injection is stopped immediately.
Absolute bed-rest is indicated after neurolytic injection without position change. This is done to avoid the an unwanted spread of neurolytics to surrounding structures.
Risks and Complications
o Rectal perforation and tract contamination
o Infection
o Fistula
o Needle break