Last Updated on October 28, 2023
Lumbosacral plexopathy is an injury to the nerves in the lumbar or sacral plexus.
Lumbosacral plexopathy can be caused by many disorders. The prevalence of lumbosacral plexopathies is unknown and is much less common than brachial plexopathies.
Risk factors vary based on cause.
Relevant Anatomy
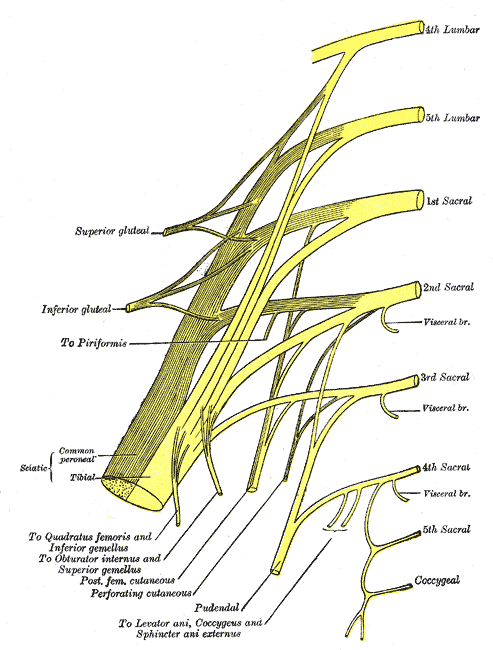
The lumbar and sacral plexuses together make lumbosacral plexus which is formed from the anterior (ventral) rami of the L1 through S4 nerve roots
The lumbar plexus is derived from the anterior rami of the L1 through L4 nerve roots. These rami pass downward and laterally along the psoas major muscle where they eventually form the plexus.
While within the psoas, they divide into anterior and posterior branches.
The posterior branches of anterior rami, L2-L4, become the femoral nerve, which exits from the lateral aspect of the psoas, traveling through the iliacus and under the inguinal ligament to the anterior thigh.
The anterior branches become the obturator nerve, that exits through the obturator foramen to the medial thigh. The lumbar plexus also gives off the lateral femoral cutaneous nerve of the thigh, iliohypogastric, ilioinguinal, and genitofemoral nerves.
The lumbar plexus and sacral plexus are united via the lumbosacral trunk, which is comprised of a part of L4 nerve root anterior rami, and all L5 anterior rami. The lumbosacral trunk passes over the sacral ala and joins the anterior rami of the S1-4 nerve roots to complete the sacral plexus.
The sacral plexus lies more inferiorly and posteriorly within the pelvic outlet. It is made up of ventral primary spinal nerve branches from L4 to S4, which form several branches including the following:
- Proximal branches to the pelvic musculature and buttock region, including nerves to the quadratus femoris, Gemelli, obturator internus, piriformis, and superior and inferior gluteal nerves.
- Posterior femoral cutaneous nerve, which has multiple sensory branches to the genitals and thigh.
- Sciatic nerve
Read detailed anatomy of Lumbosacral Plexus
Causes of Lumbosacral Plexopathy
Structural
- Retroperitoneal hemorrhage (anticoagulation, hemophilia)
- Pelvic or abdominal tumor
- Aneurysm (common or internal iliac artery)
- Endometriosis
- Trauma
Nonstructural
- Inflammatory (plexitis)
- Infarction
- Postpartum [during childbirth]
- Diabetes (diabetic amyotrophy – most common non-structural cause)
- Radiation
- Postsurgical (retractor injury)
Pattern of Injury or Plexopathy
Lumbosacral plexus lesions usually are divided clinically into
- Upper lumbar plexus [anatomical lumbar plexus]
- Lower lumbosacral plexus [anatomical sacral plexus]
Lumbar plexopathies
It predominantly affects the L2–L4 nerve fibers. Pain, if present, usually is located in the pelvis with radiation into the anterior thigh. Quadriceps, iliopsoas, and hip adductor muscles ( femoral and obturator nerves) are the affected muscles.
The knee reflex is frequently depressed or absent.
Sensory loss and paresthesias occur over the lateral, anterior, and medial thigh and may extend down the medial calf
Sensory abnormalities are
- Over the lateral thigh (lateral femoral cutaneous nerve)
- Anterior thigh (the intermediate cutaneous nerve of the thigh from femoral nerve
- Medial thigh (the femoral branch of the genitofemoral nerve, the medial cutaneous nerve of the thigh [femoral branch] and obturator nerve)
- Medial calf (saphenous nerve [femoral]).
Lower Lumbosacral Plexopathy
It predominantly affects the L4–S3 nerve fibers.
There is a complaint of a deep boring pain in the pelvis that can radiate posteriorly into the thigh with extension into the posterior and lateral calf.
The ankle reflex may be depressed or absent.
Sensory symptoms and signs may be seen over the posterior thigh and posterior-lateral calf and in the foot.
Muscles affected are
- Hip extensors (gluteus maximus)
- Hip abductors and internal rotators (gluteus medius and tensor fascia latae).
- Hamstrings
- All leg muscles supplied by the peroneal and tibial nerves.
Nerve fibers that would go to form the peroneal nerve often are preferentially affected in lumbosacral plexopathies. Therefore the patient may have foot drop and sensory disturbance over the dorsum of the foot and lateral calf. In some cases, the pattern of weakness and numbness may be difficult and electrodiagnostic studies are needed to differentiate.
Clinical Presentation
The patient typically presents with unilateral weakness, sensory loss, and pain.
The presentation may be acute or subacute depending on the cause
The Plexopathy is generally unilateral but the bilateral disease is possible (massive traumas, autoimmune diseases, or radiation-induced).
The symptoms of plexopathy would be accompanied by other symptoms of the associated conditions. For example in autoimmune disease, the skin lesions or other symptoms and signs suggestive of autoimmune disease may be present.
Systemic symptoms like weight loss, fever may be present in some conditions.
The affected limb would have signs suggestive of lower motor neuron injury.
There would be decreased muscle bulk in the distribution of the affected nerves. Muscle tone is decreased in the affected muscles, and reflexes are usually absent or greatly diminished.
[Patellar reflex is present in intact lumbar plexus whereas hamstrings reflex and Achilles reflex are affected [ supplied by the sacral plexus.]
The pattern of weakness would indicate root affected and thus guide to the part of the plexus involved.
Differential Diagnoses
- Radiculopathy
- Cauda equina syndrome [in bilateral plexopathy]
- Peroneal nerve palsy
Lab Studies
Lab studies would depend on the causation.
In general
- Blood glucose and glycosylated hemoglobin in diabetic lumbosacral plexopathy
- Erythrocyte sedimentation rate
- White blood count if an abscess is suspected
- Prothrombin time and platelets to know blood disorders
Imaging
X-rays would reveal any bony trauma.
MRI/CT can identify space occupying lesions (eg, cancer, hematoma, abscess) that may be compressing the plexus. MRI neurogram can be done evaluate if nerve root avulsion has occurred.
Neural Studies
Electrodiagnostic testing is used to localize the nerve injury and characterize the process.
Nerve Conduction Studies
Fibular and tibial motor nerve conduction studies with F waves would be absent or of low amplitude in sacral plexus involvement.
Sural, saphenous, and lateral femoral cutaneous sensory nerve conduction studies would be expected to be absent or of low amplitude, with normative distal latency unless the amplitudes are very low, in which case there may be prolonged distal latencies.too.
It must be noted that sensory nerve conduction would be normal in root avulsion too because the dorsal root ganglion cell body remains intact.
Comparison with an opposite limb or upper limb may help.
Needle electromyography
Multiple muscles innervated from L2 to S1 with multiple peripheral nerves are tested. Lumbar paraspinals should also be tested to search for radiculopathy. No motor recruitment will be seen in case the plexus is severely damaged or there is root avulsion.
Management of Lumbosacral Plexopathy
The management of plexopathy would depend on the cause. Following options are available
- Pain management
- Drugs
- Spinal cord stimulators
- Intrathecal therapies.
- Physical therapy
- Strengthening of partially affected muscles
- Correction of address muscular imbalances
- Maintain flexibility
- Improve balance and gait.
- Assistive devices and braces like AFO to correct foot drop and weakness
- Surgery in selected cases of severe nerve injury
- Preferred in root avulsions and sharp lacerations
Prognosis
The clinical course depends on the cause.
Except in root avulsion, traumatic plexopathies partial recovery normally, and many patients will have a full or nearly full recovery.
Recovery may take about 18 months after injury.
For lumbosacral plexopathy caused by compression such as (eg, retroperitoneal hematomas), outcomes can be excellent but patients may have lingering symptoms.
Similarly, for diabetic lumbosacral plexopathy, significant improvement with time occurs through some non-progressive deficits may remain.
In radiation-induced plexopathies, unfortunately, a slow but progressive loss of function is expected.
Patients of plexopathy may be left with decreased function and an abnormal gait related to muscle weakness including foot drop. There could be sensory deficits [ insensate skin].
Chronic pain may also be present.
Neoplastic plexopathy generally has a very poor prognosis when they are not resectable and resistant to radiotherapy.
Needle electromyography may be used to monitor the progress.
Common Lumbosacral Plexopathies
Retroperitoneal Hemorrhage
Retroperitoneal hemorrhage is most commonly seen in
- Complication of anticoagulation
- Hemophilia
- Aortic aneurysm rupture.
Such hemorrhages usually are located within the psoas muscle itself, where they can compress the lumbar plexus.
The presentation is of acute severe pain where the hip is flexed and slightly externally rotated.
The major neurologic deficit usually is in the femoral nerve territory, with the weakness of hip flexion and knee extension and a reduced or absent knee-jerk. However, the examination would reveal some dysfunction in the obturator or lateral femoral cutaneous nerve or both.
The treatment would depend on the cause but a decompression is almost always required.
Mass Lesions
Tumors from the bladder, cervix, uterus, ovary, prostate, colon, or rectum may compress the lumbosacral plexus leading to lumbosacral plexopathy.
Lymphoma and leukemia can directly infiltrate nerves, even in the absence of a mass lesion on imaging studies.
Aneurysms or pseudoaneurysms of the internal iliac or common iliac artery have been reported to compress the lumbosacral plexus.
In women, endometriosis can cause implantation of abnormal tissue on the plexus and cause compression. These lesions more often affect the lower lumbosacral plexus.
Endometriosis may result in intermittent symptoms but other lesions are usually slowly progressive.
Idiopathic Lumbosacral Plexitis
Idiopathic plexitis pathology is not completely known. It is thought to be inflammatory, often occurring within a few weeks of a possible inciting immunologic event, such as a cold, flu, or immunization.
There is a severe deep pain in the pelvis or in the upper leg. It characteristically persists for 1 to 2 weeks but may last many months. Because both the upper and lower plexus may be involved leading to different patterns of weakness and sensory loss.
The weakness recovers over many months to years.
Postpartum Plexopathy
Other names for this compression injury to the lumbosacral plexus during labor and delivery are maternal peroneal palsy, maternal birth palsy, neuritis puerperalis, and maternal obstetric paralysis. Although most large series place the incidence of this disorder at one in 2600 births, there are likely many milder cases that never reach medical attention.
The mechanism involves compression of the fetal head against the underlying pelvis and lumbosacral plexus. The compression primarily occurs at the lumbosacral trunk which is vulnerable as it crosses the pelvic outlet and no longer protected by the psoas muscle as they rest against the sacral ala near the sacroiliac joints.
The origin of the superior gluteal nerve lies which is close can also get compressed.
As the fibers that eventually form the peroneal division of the sciatic nerve lie posteriorly, closest to the bone, and are more vulnerable. It should be kept in mind when women present with foot drop after delivery [It can be misdiagnosed as peroneal palsy at the fibular neck.]
Weakness may be noticed immediately or within the first few days after delivery.
In addition to peroneal weakness, the examination would reveal mild weakness hamstrings; hip abduction, extension, and internal rotation indicating a higher lesion than just foot drop.
A sensory deficit is marked over the dorsum of the foot and lateral calf but may be patchy.
Diabetic Lumbosacral Plexopathy
Diabetic lumbosacral plexopathy is most common non-structural lumbosacral plexopathy. Patients develop severe aching or burning and lancinating pain in the hip and thigh, followed by weakness and wasting of the thigh muscles
It occurs in type 1 and 2 diabetes mellitus.
Often, the root and nerve levels are also involved and the disorder is called lumbosacral radiculoplexus neuropathy.
Control of sugar by adjustment of diabetes medication is important.
The management includes neuromodulator medications like gabapentin or pregabalin for neuropathic pain and selective norepinephrine reuptake inhibitors such as duloxetine.
References
- Jaeckle KA. Neurological manifestations of neoplastic and radiation-induced plexopathies.Semin Neurol.2004;24:385-393.
- Laughlin RS, Dyck JB. Electrodiagnostic testing in lumbosacral plexopathies.Phys Med Rehabil Clin N Am. 2013;24:93-105.
- Garozzo D, Zollino G, Ferraresi S. In lumbosacral plexus injuries can we identify indicators that predict spontaneous recovery or the need for surgical treatment? Results from a clinical study of 72 patients.J Brachial Plex Peripher Nerve Inj.2014;9:1.
- Kent KC, Moscucci M, Gallagher SG, DiMattia ST, Skillman JJ. Neuropathy after cardiac catheterization: incidence, clinical patterns, and long term outcome. J Vasc Surg.1994;19:1008-1013.