Last Updated on October 28, 2023
Scapular dyskinesis is a term that denotes loss of control of normal scapular motion, physiology or mechanics. It is also called sometimes as scapular dyskinesia but dyskinesis is said to be a better term as dyskinesia is applied to abnormal active movements mediated by neurological factors e.g. tardive dyskinesia.
Dyskinesis is a finding in the examination of the shoulder and could be attributed to many causes
Normal scapula function is essential for optimal shoulder function, especially in the overhead throwing athlete. The scapula is responsible for control and positioning of the humerus in relation to the glenoid so that power transfer occurs efficiently from the core to the distal upper extremity. Abnormalities of scapula function present clinically as asymmetry in scapular motion when compared to the opposite side.
Thus scapular dyskinesis is a collective term that depicts the dysfunctional movement of the scapula that may cause a possible impairment of overall shoulder function.
Overhead athletes have a higher prevalence of scapular dyskinesis of about 61% as compared with non-overhead athletes.
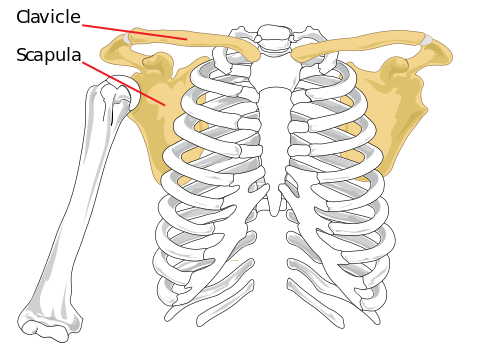
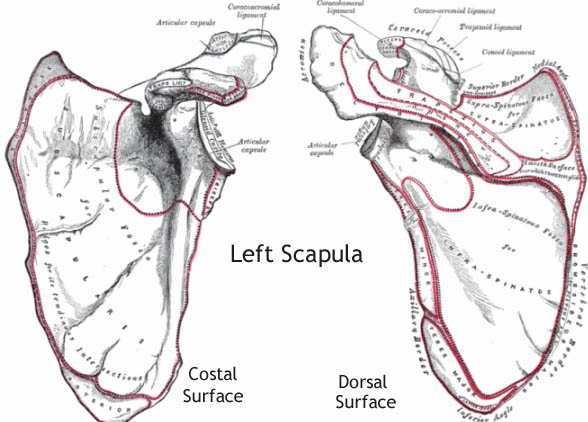
Relevant Anatomy and Biomechanics
[read scapula anatomy]
The acromioclavicular joint connects scapula to clavicle which via sternoclavicular joint connects to the axial skeleton. Muscular attachments stabilize the scapula over posterior aspect while allowing the requisite motion. Due to very few bony attachments s, the scapula is dependent on mostly muscle activation for mobility and stability.
1 7 different muscles attach to or originate from the scapula
- trapezius
- serratus anterior
- deltoid
- latisimus dorsi
- levator scapulae
- rhomboid major
- rhomboid minor
- omohyoid – inferior belly
- pectoralis minor
- teres major
- teres minor
- triceps brachii
- biceps brachii
- coracobrachialis
- infraspinatus
- subscapularis
- supraspinatus
Scapula is responsible for transfer of core strength via the glenohumeral joint to the arm and hand by optimal coupling of the muscle activations and bony motion
Normal Movements of Scapula
Normal movement of the scapula comprises components of three motions
- Upward/downward rotation around a horizontal axis perpendicular to the plane of the scapula
- upward rotation with arm elevation
- downward rotation with arm returning to side from raised position
- Internal/external rotation around a vertical axis through the plane of the scapula
- Anterior/posterior tilt around a horizontal axis in the plane of the scapula.
The clavicle acts as a strut for the shoulder complex, connecting the scapula to the axial skeleton.
This enables two translatory motions
- Upward/downward translation on the thoracic wall [shrugging action]
- Retraction/protraction around the rounded thorax.
Retraction involves coupling of scapular external rotation, posterior tilt, upward rotation and medial translation
Protraction is the coupling of internal rotation, angular tilt, downward rotation and lateral translation is called protraction.
Shrug is coupling of upward translation, anterior tilt and internal rotation.
The scapula in addition to the upward rotation tilts posteriorly and rotate externally to clear the acromion from the moving arm in elevation and abduction.
Internal and external rotation in a synchronous manner maintains the glenoid as a congruent socket.
Scapula also acts as a link in the proximal to the distal sequencing of velocity, energy, and forces of shoulder function termed the kinetic chain.
Important Muscles in Scapular Movement
- Trapezius and the serratus anterior are the greatest contributors to scapular stability and mobility.
- Lower trapezius – overhead arm stability position and in the descent of the arm from a position of maximum elevation.
- Rhomboids
- Assist the trapezius in stabilization
- Control of medial and lateral scapular translation.
- Latissimus dorsi and pectoralis minor – Affect scapular motion in their role as prime movers of the arm.
- Act mainly as force couples.
Scapulohumeral Rhythm
The ratio of glenohumeral motion to scapulothoracic motion is 2:1. Glenohumeral joint does 120° and Scapulothoracic does 60°.
[Read more on scapulohumeral rhythm]
Causes of Scapular Dyskinesis
- Bony Factors
- Fracture Clavicle
- Joint Pathologies
- Acromioclavicular arthritis
- Glenohumeral joint degeneration
- Spinal accessory nerve palsy
- Stiffness
- Pectoralis minor
- Biceps short head
- Soft tissue posterior shoulder inflexibility
- Ligamentous stiffness
- Muscular causes
- Serratus anterior weakness
- Abnormal trapezius force couple
- Decreased rotator cuff strength
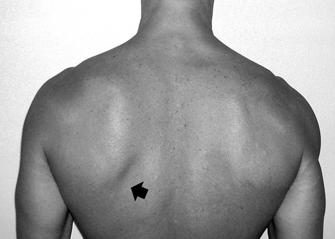
SICK Scapula Syndrome
It is a severe form of scapular dyskinesia. SICK scapula Syndrome refers to
- Scapular malpositioning
- Inferior medial border prominence
- Coracoid pain and malposition
- Kinesis abnormalities of the scapula
It’s an overuse syndrome.
The onset is insidious.
The symptoms are
- Anterior shoulder pain (most common)
- Posterior superior scapular pain
- Superior shoulder pain
- Proximal lateral arm pain
- nany combination of above. Posterosuperior scapular pain may radiate into the ipsilateral paraspinous cervical region or patient may complain of radicular/TOS type symptoms. The onset is almost always insidious.
The scapula is protracted and is in anteriorly tilted position secondary to tight pec minor or short head of the biceps at the insertion to the coracoid process.
The pain at the posterior side is the insertional pain over the scapula and is due to chronic over tension by the abducted and protracted scapula.
Coracoid tenderness is an important sign and occurs secondary to constant traction from tightness at the tendon’s insertion.
This syndrome is characterized by a drooping of the shoulder and is often seen in overhead athletes. It is thought to contribute to the development of shoulder injuries.
Classification of scapular dysfunction [Kibler]
Type I or Inferior dysfunction
The prominence of the inferior angle as a result of anterior tilting of the scapula in the sagittal plane.
- Best seen in the hands-on-hips position or during eccentric lowering from overhead elevation.
- Most commonly found in patients with rotator cuff dysfunction.
Type 2 or Medial dysfunction
- Prominence of the entire medial scapular border due to internal rotation of the scapula in the transverse plane.
- Evident in same positions as type I
- Most often occurs in patients with glenohumeral joint instability.
Type 3 or Superior dysfunction
- Excessive and early elevation of the scapula during elevation.
- Referred to as compensatory shoulder hiking or shrug
- Seen in patients with rotator cuff dysfunction and deltoid-rotator cuff force couple imbalances.
All images in classification are from the article by R Postacchini, an open-access article here.
Diagnosis of Scapular Dyskinesis
The scapula is examined routinely as a component of the shoulder examination.
Note for the presence of winging of the inferior or medial borders of the scapula is present. In addition note for scapular prominence during forward flexion, shrugging or arm lowering from a position of full flexion.
Scapular Assistance Test
It evaluates scapular contributions to impingement and rotator cuff strength by simulating the force-couple activity of the serratus anterior and lower trapezius muscles.
- Baseline active range of motion and pain is evaluated.
- Manually stabilize the scapula
- Rotate along the inferior border of the scapula as the arm moves
- If symptoms are diminished or eliminated, then scapular stabilizing muscle dysfunction is responsible and rehabilitation should aim at that The SRT
Scapular Retraction Test
can be used for evaluation in cases of labral symptoms and rotator cuff strength.
- Baseline active range of motion and pain is evaluated.
- Stabilizing the scapula in a retracted position on the thorax. [a posterior tilt and external rotation motion to the scapula]
- This confers a stable base of origin for the rotator cuff and often will improve tested rotator cuff strength.
- Reduced pain during movement indicates rotator cuff involvement
Lateral Scapular Slide Test
It enables quantitative assessment of scapular stabilizer strength.
The test evaluates three different positions of the scapula on injured and non-injured in relation to a fixed reference point on the spine.
First position – Arms by the side
The inferomedial angle of the scapula is palpated and marked on both the injured and non-injured sides. The measurements from a fixed reference point are recorded.
Second position – Hands on the hips [The fingers anterior and the thumb posterior, 10° of shoulder extension.]
The position of the inferomedial border of the scapula is marked, and the reference point on the spine is maintained. The distances are calculated on both sides.
[Scapular Load test is another separate test done in the same position where a manual load is applied in the anterior, posterior, inferior or superior direction to the arm when the arms are similar to the second position.
Third position – Arms at or below 90° of forward elevation [Maximal internal rotation at the glenohumeral joint.]
The threshold of abnormality is 1.5 cm and significant asymmetry is most commonly measured in the third position.
Isometric Scapular Pinch test
The patient is asked to actively squeeze or retract the scapulae together as hard as possible in standing position.
Normal individual- Squeezes or 15 to 20 sec without any burning pain or noticeable weakness.
Burning pain is considered positive.
Patient may relax contraction due to pain.
Wall pushup test
The patient performs wall pushups for 15 to 20 times. Weakness of scapular muscles (mainly serratus anterior) or winging usually shows up with 5 to 10 pushups. Perform the test on the floor for stronger people.
Investigations
Workups should be directed toward confirming an underlying diagnosis and would vary from case to case.
- Nerve conduction studies – To confirm injuries to injury to the long thoracic nerve, dorsal scapular nerve or spinal accessory nerve.
- Electromyography – To identify injury and the potential for recovery in periscapular muscles.
- X-rays – to rule out bony injury
- MRI – To delineate muscle injury
- MR arthrograms – Labral pathology.
Treatment of scapular dyskinesis
The mainstay of treatment for the scapular dyskinesis is physical therapy to relieve the symptoms and to re-establish muscle strength and activation patterns.
Rehabilitation for scapular dyskinesis should start proximally and end distally. It consists of
- Core stability exercises.
- Muscle strengthening exercises can be initiated.
- Re-education of muscles