Last Updated on August 28, 2021
Trigger point injections are used as a treatment modality for inactivating trigger points to provide prompt relief. Trigger points are palpable painful nodules in the taut band of muscle fibers.
Trigger points are also called myofascial trigger points as they are seen in myofascial pain syndrome, a painful muscle disorder.
[Read more on myofascial pain syndrome]
Various other modalities for the treatment of trigger points including spray and stretch, ultrasound, manipulative therapy etc.
Indications for Trigger Point Injection
Trigger points are either active or latent. Latent trigger points are not symptomatic and do not require treatment.
For injection, the trigger points should be limited in number and at an appropriate site for injection. [Conditions having widespread pain complaints, such as fibromyalgia are not suitable. Fibromyalgia can exist along with myofascial syndrome. In such cases, it is important to treat fibromyalgia first.]
Contraindications
- systemic or local infection
- Bleeding disorders
- Pregnant patient
- Ill patients
Following patients would require precautions
- Patients on anticoagulants
- Patients who are at high risk for infection
- Debilitated patients
- Diabetes mellitus
- Patients on steroids.
- Acute muscle trauma
How Does Trigger Point Injection Act?
Several mechanisms have been suggested as possible explanations for the inactivation of trigger points by injection
Following mechanisms have been thought to cause the effect
- Disruption of abnormal muscle fibers or nerve endings breaking the sensorimotor loop
- The release of intracellular potassium causing depolarization and disruption of nerve conduction due to needling
- Dilution of nerve-sensitizing substances which reduces irritability and inactivate any neural feedback mechanisms.
- Interruption feedback mechanisms between the trigger point and the central nervous system by anesthetic
- Focal necrosis may destroy the trigger point.
Procedure of Trigger Point Injection
Preprocedural Work-Up
Choosing a needle of appropriate size is important.
- For superficial muscles – 22-gauge 3.8-cm (1.5 in.) needle
- When capillary fragility with bleeding is a concern – 25-gauge needle
- Thick subcutaneous muscles – 21-gauge 5-cm (2-in.) needle or thicker
The length of the needle should be such that it does not need full-length insertion.
If the muscle is quite deep, the spinal needle may be needed.
The following sizes of needles may be used in different situations
- Scalenus, sternocleidomastoid, and interossei: 22- to 25 gauge 1.5-in. needle
- Temporomandibular joint muscles – 25 gauge 1.5-in. needle
- Cervical and suboccipital areas, upper extremities, and ankle and foot – 22-gauge 1.5-in. needle
- Extremities – 21-gauge 2.0-in. needle
- Lumbar and gluteal areas – 20- to 21-gauge 3-in. needle
- Gastrocnemius – 25-gauge 2.0-in. needle
For Withdrawal of anesthetic solution – 16-gauge 1.5-in. needle would suffice.
The patient needs to understand that he would require a period of rest after the injection and avoidance of activity.
Other equipment required include
- Needles and syringes of various sizes
- Povidone-iodine solution or alcohol
- Sterile gauze pads
- Gloves
- Lidocaine
- Isotonic saline
- Vapocoolant spray [Optional]
- Bandages
Patient Preparation
The trigger point injection may be used in prone, supine, sitting or recumbent position. Part is cleaned with povidone iodine or alcohol-based solution.
Drugs Used
One of the following may be used
- 5% procaine [least myotoxic]
- 1% lidocaine
- Bupivacaine [Long acting Anesthetics]
- Isotonic saline [when there is an allergy to anesthetic agents]
Steroids are used only for ligamentous trigger points
Needling and Injection of Trigger Point
The trigger point is located. It is felt as the most tender point in a taut muscle band. A twitch response may occur leading to muscle contraction or patient jerking or jumping [also called jump sign]
Pinch the trigger point between the thumb and index finger to prevent the trigger point from rolling away when the needle is advanced.
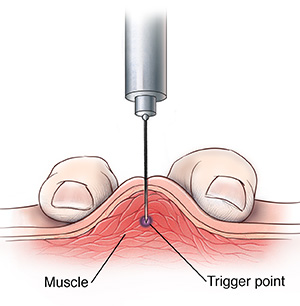
Insert the needle about 1-2 cm away from the trigger point and advance at an acute angle of 30º to the skin.
Before the needle gets to the point, warn the patient about sharp pain which may occur when the contacts the trigger point.
Aspirate before injecting.
Once inside, inject about 0.2 mL of anesthetic.
Withdraw the needle to the level of the subcutaneous tissue, and then redirect superiorly, inferiorly, laterally, and medially repeating the process of needling and injecting.
The process is repeated in each direction until the local twitch response does not occur or the muscle relaxes.
Apply pressure over the injection sites by a pressure bandage.
Stretching after trigger point injection
It is an integral part of treatment to stretch involved muscles so as to try and obtain full length.
Vapocoolant spray in a parallel direction over the muscle helps to relax remaining tense fibers.
After this apply hot pack overall injected trigger points for several minutes.
After that ask the patient to do the full active range of motion of the muscle several times. This will relieve residual stiffness and would also tell how effective the procedure has been.
This also reestablishes awareness of normal muscle function.
Postprocedural Care
Activity Modification
Ask the patient to rest the affected areas for one to two days after the injections.
As long as injection soreness is there, strenuous activities should be avoided but otherwise, the patient is encouraged to use muscle for the full range of motion.
In the long run, the patient needs to recognize and avoid the pain-provoking activities and muscle stressing movements. Learning to use muscles well and with proper alignment is key to long-lasting relief.
Exercise
After inactivation of trigger points and resolution of rest pain, a carefully graded exercise program is introduced.
Stretching exercise of the involved muscles, improved conditioning, and increased strength reduces the likelihood of developing trigger points.
Thus a graded exercise program begins with stretch exercises and the patient may progress to strengthening exercises once a tolerance to stretch occurs.
Isotonic exercises are usually better tolerated than isometric.
Conditioning exercises should be added when tolerated and done at least twice weekly. Swimming, bicycling, tennis, jogging, and jumping rope are various exercises to choose from.
Complications
Complications may include the following
- Vasovagal syncope
- Skin infection
- Pneumothorax
- Needle breakage
- Hematoma formation
References
- Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002 Feb 15. 65(4):653-60.
- Ge HY, Nie H, Madeleine P, Danneskiold-Samsøe B, Graven-Nielsen T, Arendt-Nielsen L. Contribution of the local and referred pain from active myofascial trigger points in fibromyalgia syndrome. Pain. 2009 Dec 15. 147(1-3):233-40.
- Lucas N, Macaskill P, Irwig L, Moran R, Bogduk N. Reliability of physical examination for diagnosis of myofascial trigger points: a systematic review of the literature. Clin J Pain. 2009 Jan. 25(1):80-9.