Last Updated on November 22, 2023
Achilles tendinosis is a condition due to repeated microtrauma which may cause stiffness, edema, weakness, and pain in the Achilles tendon.
Achilles tendinosis affects sports persons [runners, gymnasts, cyclists, and volleyball players] and recreational athletes. It affects inactive people too. It is said to be a failed healing response to wear and tear rather thin inflammation, though new studies have documented the presence of neurogenic inflammatory substances.
Usually, pure Achilles tendinosis is not painful. The pain, when occurs, is almost always from paratendinosis, an involvement of paratenon [a membrane around the tendon]
Mid-portion of the tendon is the most common site of tendinosis but it also occurs at the bone-tendon junction [insertion].
The true incidence of Achilles tendinosis is unknown but has been found to affect one-fifth of runners and one-tenth of dancers. Males are six times more affected than females and injuries are more common after 30 years of age.
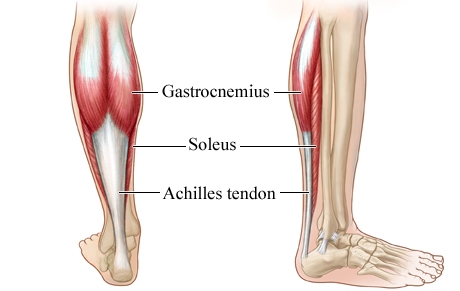
Relevant Anatomy of Achilles Tendon
The entire gastrocsoleus unit originates at the posterior aspect of the femoral condyle, spans the knee joint, ankle joint, and talocalcaneal (subtalar) joint to insert at the calcaneum.
The Achilles tendon is formed by coalescing of gastrocnemius and soleus muscle contributions about six inches before insertion.
It spirals 30-150 degrees in its course before it inserts into the calcaneal tuberosity. This spiraling helps in elastic recoil and elongation allowing greater instantaneous muscle power and increased shortening speed.
Tendon is covered by paratenon which helps in gliding. Paratenon is a two-layered structure, a visceral layer, and a parietal layer.
A bursa lies anterior to Achilles tendon and is called retrocalcaneal bursa [means bursa behind the calcaneum].
Both paratenon and bursa can become painful on inflammation and need to be differentiated from tendinosis.
Achilles tendons in women have a smaller cross-sectional area than in men.
The blood supply to the Achilles tendon is derived mainly from vessels traversing the mesotendon, small longitudinal supplies from the muscle bellies and the distal insertion.
This gastrocsoleus unit flexes the knee, plantarflexes the ankle and supinates the subtalar joint. During running, the tendon is subjected to forces equivalent to 10 times the body weight during running.
Pathophysiology of Achilles Tendinosis
Paratenonitis is inflammation of paratenon leading to thickening and adhesions. Tendinosis represents degeneration of the tendon. Paratenonitis may occur independently or along with tendinosis.
Partial or full tendon ruptures may result from end-stage paratenonitis.
Though Achilles tendinosis is considered non-inflammatory in nature, there are, however, signs of neurogenic inflammation suggested by the presence of neuropeptides such as substance P and calcitonin.
Changes are noted in tendinosis include collagen degeneration, fiber disorientation, and increased mucoid ground substance.
However, no increase in inflammatory cells is found. Increase in a number of cells vascular proliferation is usually present along with an increase in the number of tenocytes or tendon cells.
There is an increase in apoptotic cells [dead cells] and there is an increase in the proportion of type III collagen is also increased in the degenerated tendon. [Aging also causes the same change to a lesser degree]
Tendon degeneration is of two types
- Lipoid – There is increased lipid content in tendon tissue
- Mucoid – The tendon has mucoid patches and turns brown or gray
Neovascularization [formation of new blood vessels] when occurs is associated with painful tendinosis.
Causes of Achilles Tendinosis
Tendinosis occurs due to multiple causes and exact causation is not completely understood
Excessive load on running and pronation associated with the process or excess dorsiflexion of the ankle with pedaling in cyclists are thought to contribute to the causation.
There are intrinsic or patient-related factors and extrinsic factors which are due to external influences like training or medication.
Intrinsic factors
- Increased age
- Varus alignment with functional hyperpronation of foot
- high arched foot
- Tibia vara (Blount disease)
- Weak gastrocsoleus
- Stiff ankle dorsiflexion
- Family history
In addition to these factors, diseases like gout, collagen disorders, infectious diseases, metabolic disorders, systemic lupus erythematosus, rheumatoid arthritis, renal failure, psoriasis, and seronegative arthritis can affect the Achilles tendon
Blood group O is also associated with a higher risk of Achilles tendinosis.
Extrinsic factors
- Athletic activities esp jumping and running
- Overuse – increased intensity or duration of activity
- Participation in a new activity
- Stairs and hill climbing
- Poor footwear
- Irregular or hard training surfaces
- Insufficient or improper stretching exercises
Drugs like steroids [oral or intratendinous injections] and quinolones appear to increase the tendon degeneration and rate of rupture
Because tendinosis also occurs in inactive people, the theory of overuse is being challenged.
Clinical Presentation of Achilles Tendinosis [Signs and Symptoms]
Paratenonitis is characterized by localized pain during or following activity occurs and as the disease progresses, pain onset may occur earlier during activity.
Tendinosis only is not painful but may cause a sensation of fullness or nodule.
Paratenonitis with tendinosis causes activity-related pain and diffuse swelling of the tendon sheath with nodularity.
But overlap of symptoms can occur because both things can occur together to varying degree.
Pain and stiffness which are worse in the morning after getting up, are the main complaints in the affliction of Achilles tendon.
Initially, pain occurs after the activity and becomes tolerable with a continuance of activity. Later on, the pain may occur at the beginning of the activity.
In the examination, it is to be confirmed that one is not dealing with a case of Achilles tendon rupture than Achilles tendinosis. The rupture can be excluded by the calf squeeze test.
[Read more on Achilles Tendon Rupture]
If the tendon is found intact, the patient is examined for pain provocation. Mostly, it can be accomplished by a simple heel raise. In other patients, repeated hopping might be required
Gastrocsoleus muscle and Achilles tendon are checked for swelling, warmth, tenderness, and nodules. If nodules are present Individual nodules should also be palpated and checked for size, border, mobility, and tenderness.
Comparison with contralateral side would provide a fair assessment of calf wasting, a sign of chronicity.
The range of motion should be checked in the knee, ankle, and subtalar joints.
The limb should be checked for problems that can increase the risk of Achilles tendinosis [mentioned above]
Differential Diagnosis of Achilles Tendinosis
- Retrocalcaneal bursitis
- Osteoarthritis of Ankle
- Calf injuries
- Fascial tears
- Gastrocsoleus muscle strain or rupture
- Arthropathies such as psoriatic arthritis
- Partial Achilles tendon rupture
- Tendinous xanthomas
- Vascular injuries
- Ankle Impingement Syndrome
- Ankle Sprain
- Chronic Exertional Compartment Syndrome
- Deep Venous Thrombosis
Lab Studies
For diagnosis, laboratory studies are not required in cases of Achilles tendinosis. Following lab studies though may help to rule out other possibilities:
- Complete and differential blood count
- Erythrocyte sedimentation rate
- C-reactive Protein
- S. uric acid
- Coagulopathy panel
- Arthritis panel
Imaging
Role of imaging is similar to lab studies.
X-rays may reveal tendon calcifications or spurs but neither is diagnostic.
MRI can differentiate complete and partial tear of the Achilles tendon. It can also distinguish between paratenonitis, tendinosis, and bursitis.
Treatment of Achilles Tendinosis
In the acute phase, rest from sporting activities, medication like NSAIDs and ice packs are used to relieve the symptoms.
An ice pack should be applied for 10-30 minutes 3-4 times a day.
After acute symptoms have subsided the patient is put on physical therapy.
[Read Exercises for Achilles Tendinosis]
In the beginning, pain is used to guide the intensity of exercises which consist of active ankle dorsiflexion with gentle calf stretching.
It is followed by strengthening exercises and neuromuscular control programs are initiated.
In the last phase, progressive stress is applied to allow the collagen to form appropriately and aggressive stretching and active resisted motion when pain reduces. These are called eccentric musculotendinous training provide relief up to 60-90 %.
The idea is to progressively load them until the exercises provoke pain. Insertional Achilles tendon pain is not as responsive to eccentric musculotendinous training.
Eccentric exercise affects type I collagen and may increase the tendon volume and tensile strength in the tendon over time.
The athlete can begin sport-specific training after this and activity should be decreased on pain.
All the preventive measures [see below] should be taken to not subject the tendon to erroneous loading again.
Orthotics
The night splint can be used in cases with tight Achilles tendon. This keeps the ankle at 5° dorsiflexion. In cases with hyperpronation, custom orthotics with medial heel lift may be tried.
Achilles tendinosis usually heals within 3-6 months of these treatments but if symptoms have not improved after 3-6 months, following treatments may be considered.
Extracorporeal Shock-wave therapy
Special sound waves are passed through your skin to Achilles tendon. The data seems positive but still, it is uncertain how effective this treatment is and how well it works.
Autologous Blood Injection
In this patient’s own blood is taken and injected around Achilles with an idea to promote healing by encouraging the growth of cells involved in the healing process. Long-term effects and efficacy are not very clear.
Similarly, the effects of platelet-rich plasma are also not clear very well.
Glyceryl Trinitrate Patch
Glyceryl trinitrate skin patch may be used as an adjunct to exercise program. Nitric oxide stimulates collagen synthesis and promotes tendon remodeling
Corticosteroid Injection
Intradentinous injection is contraindicated as it can increase the risk of rupture. Paratendinous injection though not that effective, can serve as the adjunct to relieve pain during exercises programs.
Sclerosing Injections
Polidocanol has a sclerosing and anesthetic effect and its injection into Achilles tendon decreases neovascularisation.
Sclerosing therapy is used in those who fail to respond to eccentric exercise.
Surgery for Achilles Tendinosis
About 25% of people may need surgery. The frequency of surgery increases with patient’s age and duration of symptoms.
In paratenonitis, surgery involves either removal of the nodule or adhesion or make the longitudinal cut in the tendon to stimulate tendon healing.
In tendinosis, the following procedures may be added
- Excision of degenerated portions of the tendon and any osteophyte
- In case the remaining tendon thins out, augmentation by plantaris or flexor hallucis longus tendon can be done.
Surgeries are less successful in nonathletic persons.
Prevention of Achilles Tendinosis
Following cautions should be taken to decrease chances of occurrence of Achilles tendinosis.
- Appropriate footwear.
- Gradually add intensity or duration to training
- Proper warm and stretch of calf muscles
- strengthening of calf muscles and Achilles tendon [Eccentric training]
- Wear orthotics to correct biomechanical abnormalities
- Preventive exercises are aimed at strengthening the gastrocnemius and soleus muscles,
Prognosis of Achilles Tendinosis
Achilles tendon injury has an excellent prognosis. If well treated, it does not have any long-term effects and most athletes with a return to their previous activity levels.
Untreated, it can lead to prolonged pain and dysfunction.
Achilles tendinosis carries a risk of rupturing the tendon.