Last Updated on November 22, 2023
Ankle sprain accounts for up to 40% of all athletic injuries and is most commonly seen in athletes participating in basketball, soccer, running, and ballet/dance. The ankle sprain is usually caused by an inversion-type twisting injury.
About eighty percent of acute ankle sprains recover completely, 20% develop mechanical or functional instability resulting in chronic ankle instability.
Chronic ankle instability can lead to early degenerative changes in the ankle due to unbalanced loading on the medial side of the ankle.
Most ankle sprains are never reported as they are self-treated.
Female athletes are 25% more likely to sustain ankle injuries than male athletes. But males have a higher risk of syndesmotic ankle sprains.
Lateral ligament sprains constitute 85% of ankle sprains [inversion sprains] out of which anterior tibiofibular ligament is most commonly involved, 5% are eversion sprains of the deltoid or medial ligament, and 10% are syndesmotic injuries.
Anatomy of Ankle Joint
The ankle joint is hinge joint formed by the contribution from the lower end of tibia, fibula, and talus.
Stability of the ankle is due to the bony configuration of the ankle mortise and talar dome, ligamentous structures, capsule, syndesmosis, and the crossing tendons.
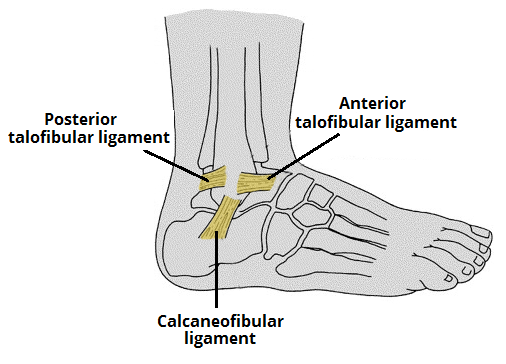
The lateral ankle complex is most commonly involved in the ankle sprain. It is composed of
- Anterior talofibular ligament (ATFL)
- Calcaneofibular ligament (CFL)
- Posterior talofibular ligament (PTFL)
The ATFL is the weakest of the lateral ankle ligaments and most common of the lateral ligaments to get injured. It originates 1 cm proximal to the distal tip of the fibula and inserts on the lateral talar neck just beyond the articular surface about 18 mm proximal to the tibiotalar joint. This ligament is It is contiguous to the ankle joint capsule and has been found to be a discrete capsular thickening. It measures 6 to 10 mm in width, 10 mm in length, and 2 mm in thickness.
Calcaneofibular ligament originates on the distal tip of the fibula, travels in an oblique direction plantarly and posteriorly towards its calcaneal insertion 13 mm distal to the subtalar joint. ATFL forms a 47° angle to the sagittal plane and 25° angle to the horizontal. It is the only extra-articular ligament within the lateral complex.
ATFL is the primary restraint against plantar flexion and internal rotation of the foot.
Calcaneofibular ligament measures 20 to 25 mm in length and 6 to 8 mm in diameter and crosses both the tibiotalar and subtalar joints. The CFL forms a 133° angle with the fibula and a 104° angle with the ATFL. The CFL also forms the floor of the peroneal tendon sheath. It is larger and stronger than the ATFL.
The calcaneofibular ligament is relaxed in plantar flexion and taut in dorsiflexion. It stabilizes the ankle and prevents talar tilt as the ankle moves from neutral into dorsiflexion.
The posterior tibiofibular ligament is the strongest of the lateral ankle ligaments and originates 10 mm proximal to the distal tip of the fibula and inserts onto nearly the entire nonarticular portion of the posterior talus up to the flexor hallucis longus groove. It is rarely injured in ankle inversion sprains This ligament is usually not involved in chronic ankle instability.
Pathophysiology of Ankle Sprain
The most common mechanism of injury in ankle sprains is forced plantar flexion and inversion of the ankle as the body’s center of gravity rolls over the ankle. The anterior tibiofibular ligament followed by calcaneofibular ligaments are the most commonly injured.
The ankle joint is a hinged synovial joint with plantar flexion and dorsiflexion as main movements. Subtalar joint [calcaneocuboid joint, talocalcaneal and talonavicular joints together] are responsible for other movements that add to the motion of ankle joint.
During forced dorsiflexion, the PTFL can rupture. With forced internal rotation, ATFL rupture is followed by the injury to the PTFL. Extreme external rotation disrupts the deep deltoid ligament on the medial side, and adduction in neutral and dorsiflexed positions can disrupt the CFL. In plantar flexion, the ATFL can be injured.
The deltoid ligament or tibiotalar ligament is the strongest ligament consisting of two parts superficial and deep that run to tarsal bones from medial malleolus. It is so strong ligament that the medial malleolus usually fractures before the deltoid ligament fails mechanically.
The syndesmotic ligament consists of many ligaments and is a distal tibiofibular ligament that holds the distal tibia and fibular bones together at the ankle joint and maintains the integrity of the ankle mortise. It is not commonly injured but a severe injury to this requires surgery.
A syndesmotic ligament tear is usually a part of an ankle fracture that needs to be treated specifically. This is not generally true of the other ankle ligament tears.
Classification of Ankle Sprain
Grade 1 injuries
- A stretch of the ligament with microscopic tearing
- No macroscopic tearing
- Little swelling is present
- No functional loss
- No joint instability
- Patient is able to fully or partially bear weight.
Grade 2 injuries

- Stretch the ligament with partial tearing
- Moderate-to-severe swelling
- Ecchymosis
- Moderate functional loss
- Mild-to-moderate joint instability
- Patients usually have difficulty bearing weight.
Grade 3 injuries

- Complete rupture of the ligament
- Immediate and severe swelling
- Ecchymosis
- Inability to bear weight
- Moderate-to-severe instability of the joint.
High and Low Ankle Sprains
Depending on the location ankle sprains can be called high ankle and low ankle sprains.
High ankle sprain
This refers to the injury of syndesmotic ligaments. It constitutes 1-10% of ankle sprains
Low ankle sprain
It denotes lateral [most common] and medial ligament injuries. Low ankle sprains are >90% of all ankle sprains.
Depending upon lateral or medial location, these can be subdivided into
Lateral ankle sprain or Inversion Ankle Sprains
This is the most common type of ankle sprain where the foot is inverted and injury occurs on the lateral side of the ankle because lateral, ligaments are stretched. The anterior talofibular ligament is one of the most commonly involved ligaments in this type of sprain. Approximately 70-85% of ankle sprains are inversion injuries.
Eversion Ankle Sprain or Medial Ankle Sprain
It is a less common type of ankle sprain that affects the medial side and is associated with eversion of the ankle resulting in stretching of medial deltoid ligament.
Causes and Risk Factors of Ankle Sprain
Ankle sprain occurs when mechanical forces exceed the tensile limits of the ankle joint capsule and supportive ligaments cause ankle sprains.
Acute Ankle Sprain
Predisposing factors
- Lack of physical conditioning
- Poor muscle tone
- Shortened and/or contracted joint capsule or tendons
- Poor proprioception
- Inadequate training or experience [athletes]
Provocative factors
- Accidents
- Unforeseen mechanical stresses that exceed the tensile limits
- Obesity [ kinetic energy exceeds joint- stress limits]
Recurrent sprains
These occur after an episode of acute injury
The exact etiology of recurrent ankle sprains is unknown
Following factors are thought to contribute
- Lengthening of ligaments due to intervening scar tissue healing in a lengthened position
- Scar tissue filling in the gap between the torn, separated ends.
- Inherent weakness of the scar.
- Persistent peroneal weakness.
- Unrecognized disruption of the distal tibiofibular ligament
- Loss of proprioception in the foot
- Disrupted mechanoreceptors and their afferent nerve fibers
- Dysfunction of the peroneal nerve
- Impingement of the capsular scar tissue in the talofibular joint
- Hereditary hypermobility of joints
This grading system fails to characterize ankle injuries involving 2 or more ligamentous structures and excludes consideration of nonligamentous injuries.
Clinical Presentation of Ankle Sprains
There would be a history of an inversion-type twist of the foot followed by pain and swelling. Details of the mechanism of injury would reveal the biomechanics of injury.
The patient is often able to walk on foot though with pain [walking usually excludes fracture]
After the injury, there is a sudden, intense pain and rapid onset of swelling and bruising.
On examination, there would be areas of tenderness and swelling on lateral [mostly[ or medial aspect [ in medial ankle sprain].
The maximal points of tenderness for a lateral ankle sprain should be at the ATFL and/or CFL ligament areas.
Ecchymosis may be present and may be tender. The blood usually settles along the medial or lateral aspects of the heels and therefore the location of ecchymosis may not correlate with the location of the injury.
Bony point tenderness should be looked for and excluded especially at medial malleolus, lateral malleolus, the base of the fifth metatarsal, and midfoot bones.
Any bony tenderness points to possible fracture.
The range of motion is assessed. The neurovascular examination is done in the detail.
Active range of motion must be assessed because Achilles tendon ruptures can mimic ankle sprains.
The patient record for the previous history of any illness and/or medication is sought.
Provocative Tests
The use of these tests in acute injuries is in question because of pain, edema, and muscle spasm.
Inversion-Eversion
In lateral sprains, passive inversion should reproduce the symptoms. The opposite is true for medial injuries. Plantar flexion should also exacerbate the symptoms because this motion stretches the ATFL to its maximum.
Anterior Drawer Test
The patient’s knee is flexed to relax the gastrocsoleus complex, and the foot should be in 10° of plantar flexion. Grasp the heel and pull forward while, with the other hand, providing counterpressure over the front of the tibia at the level of the ankle. A firm endpoint will be absent. Repeat these steps for the other ankle, and compare results.
[The normal amount of translation is 2 mm. Reports indicate that 4 mm of laxity in the ATFL provides a clinically apparent test result.]
The injured side has more movement than the uninjured one.
A dimple over the area of the ATFL on anterior translation. [Dimple (or suction) sign] indicating a compromise of the ATFL. It may be accompanied by pain, but muscle spasms are minimal.
The anterior drawer test is not very reliable.
In prone anterior drawer test is the patient lies prone with the feet extending over the end of the examining table. The examiner then pushes the heel steadily forward with one hand. A positive test result consists of excessive anterior movement and a dimpling of the skin on both sides of the Achilles tendon.
Talar tilt test or Inversion stress maneuver
The patient is supine or lateral. The gastrocnemius should be relaxed by flexion of the knee. The talus is then tilted from side to side into adduction and abduction. The findings should be compared with those for the contralateral side.
Fluoroscopy of the maneuver is more informative than the clinical test alone.
External Rotation Test
This is used to demonstrate the integrity of the syndesmotic ligaments.
The patient sits with the knee flexed to 90°. The foot is gently grasped and rotated laterally with the ankle locked in neutral. Pain over the syndesmosis signifies a positive test. Though this test is quite specific, it is not highly sensitive.
Kleiger test is a variation of this test to demonstrate the integrity of the deltoid ligament. The patient sits with the knee flexed to 90° and foot relaxed and non-weight bearing.
The foot is gently grasped and rotated laterally. A positive test result occurs when the patient has pain medially and laterally. The talus may displace from the medial malleolus, indicating a tear of the deltoid ligament.
Fibular Compression Test or Squeeze Test
This test is done in a suspected syndesmotic or fibular injury.
Place the thumb on the tibia and the fingers on the fibula at the midpoint of the leg. Squeeze the tibia and fibula together.
Pain down the length of the fibula indicates a positive test result. The pain should not be felt at the site of the pressure but rather in the lower leg. A positive test suggests an ankle sprain involving syndesmosis and tibiofibular ligaments. Another differential Maisonneuve fracture of the proximal fibula. This test also has high specificity but low sensitivity.
Evaluation for Chronic Instability
The symptoms are often vague.
There would be a history of giving-way symptoms of the foot during activity. There would be recurrent, pain, swelling, and stiffness.
Distinguishing between subtalar and tibiotalar instability is difficult.
Instability may result from tibiotalar laxity or subtalar instability.
Chronic medial ligament instability is rare and presents with discomfort on the medial side of the ankle. It is associated with slight valgus and abduction of the ankle with each step.
Differential Diagnoses
- Achilles Tendon Injuries
- Achilles Tendonitis
- Ankle fractures
- Distal Fibula Fracture
- Fifth Metatarsal Fracture
- Navicular Fracture
- Calcaneus Bone Injuries
- Ankle Impingement Syndrome
- Chronic Ankle Instability
- Complex Regional Pain Syndrome
- Tendon Injuries
- Flexor Hallucis Longus Tendon Injury
- Peroneal Tendon Syndrome
- Tibialis Posterior Tendon Injury
- Gout and Pseudogout
- Postexercise Muscle Soreness
- Subtalar Joint Sprain or Instability
Imaging
X-rays
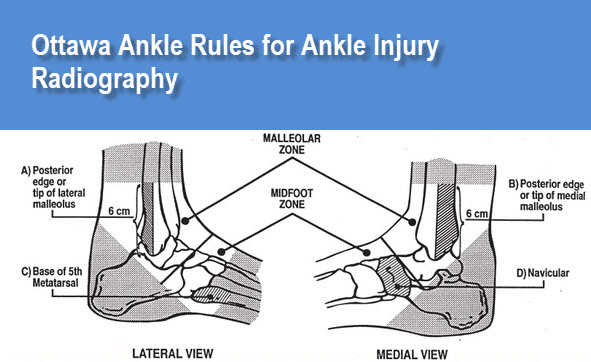
X-rays in ankle injuries is guided by the Ottawa Ankle Rules.
According to these rules, ankle x-rays are required only if the patient has pain in the malleolar zone and any of the following 3
- Bone tenderness at the posterior edge or tip of the lateral malleolus (ie, the lower 6 cm of the fibula)
- Bone tenderness at the posterior edge or tip of the medial malleolus (ie, the lower 6 cm of the tibia)
- Inability to bear weight immediately after the injury and in the emergency department
In addition, the Ottawa Ankle Rules state that foot x-rays are required only if the patient has any pain in the midfoot zone and any of the following
- Bone tenderness at the base of the fifth metatarsal
- Bone tenderness at the navicular bone
- Inability to bear weight immediately after the injury and in the emergency department
The Ottawa Ankle Rules are applicable when the patient presents within 10 days of the injury and can be considered for use in ages higher than 5 years
Radiographic Series
- An anteroposterior (AP) film with the ankle in 5-15° of adduction
- A true lateral film
- A 45° oblique film with the ankle in dorsiflexion (ie, Mortise view)
The basic purpose of x-ray series is to look for any bony injury or subluxation of the joint including syndesmosis.
Stress Views
Stress radiography is not reliable in acute injuries because of pain.
Moreover, ankle stress radiographs contribute little to the management of acute ankle sprains because the surgical treatment of the acute sprain is rarely indicated.
Stress views are important for determining ankle instability. In case of pain, the views should be done under local anesthesia for better accuracy. The opposite limb may be viewed for comparison.
CT
CT provides better image quality than the x-ray. It is useful in osteochondritis dissecans and stress fractures..
MRI
MRI is useful in high ankle sprain [syndesmotic sprain], talar osteochondral lesions, peroneal tendon pathology and in detail assessment of tears. MRI is highly sensitive, specific, and accurate after acute trauma.
MRI can be considered if pain persists for 8 weeks following a sprain.
Bone Scanning
A bone scan can detect subtle bone abnormalities like the stress fracture, osteochondral defects. It is also helpful for detection of syndesmotic disruption.
Treatment of Ankle Sprains
The aim of the treatment in acute ankle sprain is to reduce pain, provide an optimum healing environment, restore range of motion, strength, and proprioception.
Most of the treatment in acute ankle sprains is conservative. Even in third-degree ATFL tears and medial ankle ligament tears, surgery does not improve the outcome.
Non-Operative Treatment for Ankle Sprain
Acute Injury
This treatment can be extended to all grades of sprain. The treatment includes RICE [rest, ice, compression and elevation] and protection.
Protection is provided for a short period [4-21 days depending on severity, average around a week). It is in form of weight-bearing immobilization in a walking boot or walking cast or splint.
The patient is advised to avoid activities that cause increased pain or swelling and use ice to control swelling, pain, and muscle spasm. Elevation of the injured ankle will facilitate the reduction of swelling. Ideally, the ankle should be above the level of the heart.
Early mobilization facilitates a better recovery and the patient is asked to carry pain-free movements [guided by pain] by taking their ankle out of the brace.
Once swelling and pain have subsided and the patient has a full range of motion, the patient should begin neuromuscular training. The focus is on peroneal muscles strength and proprioception training
A brace that controls inversion and eversion is typically used during the strengthening period.
If the patient is an athlete the same type of brace can be used for used as prophylaxis during high-risk activities after return to physical activity.
Recurrent Sprain
The treatment of the recurrent lateral ankle begins with a trial of non-operative therapy for approximately 2-3 months. It consists of strength exercises [esp peroneal muscles which act as a dynamic stabilizer of ankle], protective support, sports-specific functional progression and proprioceptive/coordination exercise.
Treatment of medial recurrent sprains includes ankle stirrup bracing, casting, and orthoses in addition to physical therapy. Surgery is indicated if these measures are not effective.
In the case of the sportspersons, the treatment is seldom accepted and surgical stabilization is required.
In most cases, arthroscopic evaluation of the ankle joint is helpful in determining the best course of management.
In syndesmotic injuries, when a diastasis has been present for longer than 3 months, significant arthritic changes
Operative Treatment
Indications for Surgery in Acute sprain are
- Third-degree sprain with the widening of the ankle mortise
- Intra-articular trapping of deltoid ligament after third-degree sprain
- Grade I-III that continue to have pain and instability despite extensive nonoperative management
- Grade I-III with a bony avulsion
Consider arthroscopic evaluation prior to reconstruction for intra-articular evaluation.
The surgical option in acute injury is anatomic reconstruction [Brostrom].
In old cases, tendon transfer and tenodesis [Watson-Jones, Chrisman-Snook] is considered. It is a nonanatomic reconstruction using a tendon transfer. Subtalar stiffness is a common complication
Arthroscopic debridement/removal of impingement in chronic pain caused by impingement as in anterior-inferior tibiofibular ligament impingement
Return to Play
It depends on, grade of sprain, syndesmosis injury, associated injuries, and compliance with rehabilitation
- Grade I and II injuries take 1-2 weeks for return.
- Grade II several weeks
- High ankle syndesmotic sprains take several weeks to several months
Complications of Ankle Sprain
Chronic Pain is the most common issue. Experienced in up to 50%. Most common cause of chronic pain is a missed injury, including injury to
- Anterior process of the calcaneus
- Lateral or posterior process of the talus
- Base of the 5th metatarsal
- Osteochondral lesion
- Injuries to the peroneal tendons
- Injury to the syndesmosis
Other causes are tarsal coalition and impingement syndromes.
Therefore, if pain persists despite rehabilitation, further workup is indicated.
Other complications of an acute ankle sprain are
- Chronic lateral ankle instability
- Intra-articular meniscoid lesions [ impingement syndrome.]
- Peroneal tendon subluxation
- Talar dome fracture
- Anterior process fracture of the calcaneus occurs with inversion injuries. Patients commonly display bony tenderness rather than ligamentous point tenderness.
- Complex regional pain syndrome
Prevention of Ankle Sprain
Following precautions in athletes with prior sprains can help in prevention
- High-top shoes
- Using a Semirigid orthosis like ankle braces
- Evertor muscle strengthening
- Proprioception exercises
- Adequate training and conditioning to
- An adequate warm-up period
- A gradual transition into activity
- Shoes with good stability
- Exercise on even surfaces.
Prognosis of Ankle Sprains
The prognosis for isolated and adequately treated ankle sprains is excellent. After 12 months, the risk of recurrent ankle sprain returns to pre-injury levels.
Participation in competitive sports is a risk factor for residual symptoms.
Early treatment of recurrent ankle sprains also carries an excellent prognosis.
Posttraumatic osteoarthritis is common in patients with repetitive ankle injuries.
References
- Ivins D. Acute ankle sprain: an update. Am Fam Physician. 2006 Nov 15. 74(10):1714-20
- Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000 May. 29(5):361-71.
- Mahaffey D, Hilts M, Fields KB. Ankle and foot injuries in sports. Clin Fam Pract; 1999. 1(1):233-50.
- Kannus P, Renström P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991 Feb. 73(2):305-12.
- Lohrer H, Alt W, Gollhofer A. Neuromuscular properties and functional aspects of taped ankles. Am J Sports Med. 1999 Jan-Feb. 27(1):69-75.
- Ankle sprains in soccer: a prospective study on 100 professional players. Am J Sports Med. 2012 Aug. 40(8):1842-50.
- Lynall RC, Mauntel TC, Padua DA, Mihalik JP. Acute Lower Extremity Injury Rates Increase following Concussion in College Athletes. Med Sci Sports Exerc. 2015 Jun 8.