Last Updated on November 22, 2023
Term shoulder pain refers to any pain that arises in or around the shoulder. The origin of the pain may be in the shoulder joint or from surrounding structures like muscles, ligaments or tendons.
Shoulder pain is the third most common musculoskeletal pain after low back pain and neck pain.
This kind of pain usually becomes worse with movements or activities of shoulder.
Sometimes a distant disease or pathology may cause pain being referred to shoulder. This may happen in pathologies of neck, chest or abdomen. For example, conditions such as heart disease or gallbladder disease, also may cause shoulder pain. This kind of pain is termed as referred shoulder pain. Referred shoulder pain does not become worse with movements or activities of the shoulder.
Common shoulder problems share overlapping clinical features. Therefore it is important to understand the underlying causes and their differentiation.
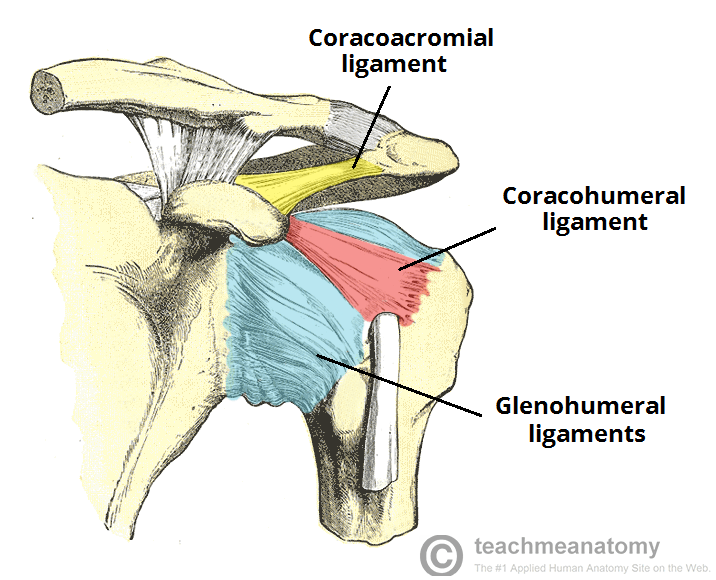
Anatomy of the Shoulder Joint
Shoulder joint is made by
- Head of Humerus
- Glenoid of scapula
- Acromion process of scapula
- Clavicle
- Muscles and Ligaments
Following are important articulations of shoulder joint
- Sternoclavicular joint
- Acromioclavicular joint
- Glenohumeral joint.
Rotator cuff, which is composed of supraspinatus, infraspinatus, teres minor and subscapularis muscles that function as one unit by forming common tendon, also called as rotator cuff tendon. Rotator cuff helps with internal and external rotation of the shoulder and depresses the humeral head against the glenoid on elevation of arm.
The common rotator cuff tendon passes through subacromial space. A bursa called subacromial bursa separates the acromion from the rotator cuff tendon.
Read detailed anatomy of shoulder here
Who is at Risk for Shoulder Pain
There are certain risk factors which increase the likelihood of shoulder pain. These are
- Physical factors
- Occupation that requires repetitive shoulder movements – garment makers, construction workers, welders, food processing, painters and decorators, workers using computer keyboards
- Exposure to vibration from machine tools.
- Sportsperson
- Overhead activities
- High-impact contact sports
Causes of Shoulder Pain
Shoulder pain can be result from injury or disease of the shoulder join and surrounding structures or pain could be referred from elsewhere.
Following are the main causes of shoulder pain.
Causes Intrinsic to Shoulder
- Shoulder Trauma
- Fractures of humeral head, glenoid, clvicale, scapula
- Ligament injury
- Rotator cuff Conditions
- Injury to rotator cuff
- Subacromial bursitis
- Rotator cuff tendinopathy.
- Adhesive capsulitis
- Shoulder Arthritis.
- Acromioclavicular Arthritis.
- Biceps tendonitis.
- Infection
- Shoulder Instability
Causes Extrinsic to Shoulder
- Referred pain
- Neck pain
- myocardial ischaemia
- Referred diaphragmatic pain
- Gall bladder disease
- Subphrenic abscess
- Polymyalgia rheumatica.
- Malignancy
- Apical lung cancers
- Metastases
Barring acute injuries, rotator cuff disorders, glenohumeral disorders, acromioclavicular joint disease and referred neck pain are most common causes of shoulder pain.
Rotator Cuff Disorders
In shoulder there is impingement of tendons of rotator cuff and/or bursa in the shoulder in subacromial space. Repeated impingement leads to irritation and inflammation of the structures irritated and inflamed as they pass through the subacromial space causing pain and stiffness of the shoulder.
Pain initially occurs on overhead activities. Night pain on lying on affected side is common complaint. Sometimes, the patient complains of grinding or popping sensation during movement.
A painful arc of movement may be present during forward elevation of the arm from 60° to 120°. [Also called painful arc syndrome]
[Read shoulder impingement syndrome in detail]
Supraspinatus Tendonitis or Rotator cuff tendonitis
Rotator cuff tendonitis [also termed as supraspinatus tendonitis] is inflammation of the supraspinatus/rotator cuff tendon and/or the soft tissues around them. Rotator cuff tendonitis is a common cause of shoulder pain in sportspersons and laborers whose profession involve throwing and repetitive overhead motions.
If rotator cuff tendonitis is not diagnosed and treated promptly and correctly, it can progress to rotator cuff degeneration and eventual tear. Adhesive capsulitis, cuff tear arthropathy, and reflex sympathetic dystrophy may also occur.
Impingement implies compression of the rotator cuff in the supraspinatus outlet space and is thought to be an important cause of rotator cuff tendonitis.
[Read full article on Rotator Cuff Tendonitis]
Rotator cuff injury is a condition characterized by partial or complete tearing of one or more of the rotator cuff muscles. The rotator cuff is formed by supraspinatus, infraspinatus, subscapularis and teres minor. The supraspinatus is most commonly affected. Rotator cuff tears are usually found in persons aged 55-85 years.
[Read full article on Rotaor Cuff tendonitis]
Calcific Tendonitis
There is deposition of crystalline calcium phosphate in the rotator cuff tendon.
The cause is not known. It is more common in women and affects people between age 30-60 years.
The calcium eventually resorbs but may take many years and make the shoulder symptomatic
Adhesive Capsulitis
Adhesive capsulitis si commonly known as frozen shoulder. It is a condition where soft tissue surrounding the shoulder – shoulder capsule, the surrounding connective tissue surrounding becomes inflamed and results in restriction of motion and pain.
Adhesive capsulitis is more common in people with diabetes and may also occur after prolonged immobilisation.
It most commonly occur in age 40-65 years.
Osteoarthritis of the Shoulder
Osteoarthritis of the shoulder is a degenerative condition of the shoulder where joints undergo degenerative changes due to loss of cartilage surface and causes pain first on activity and then on rest. It is more common in patients >60 years of age.
Other arthritis can also involve the shoulder and be a cause of the shoulder joint pain.
Acromioclavicular Conditions
Trauma to acromiclavicular joint or osteoarthritis of acromioclavicualr joint can cause shoulder pain. The pain and tenderness are localized to the acromioclavicular joint. One of the signs is the restriction of passive, horizontal movement of the arm across the body when the elbow is extended.
Acromioclavicular osteoarthritis may cause subacromial impingement.
Referred Neck Pain
Conditions of neck such as cervical spondylosis or muscle spasm may cause pain in the shoulder as well.
The typical presentation is pain and tenderness of the lower neck and suprascapular area, with pain referred to the shoulder and upper arm.
Usually the activities of shoulder are not affected. Sometimes, the active movement may be difficult due to muscle spasm but passive motion is feasible.
Upper limb paraesthesia may be present.
Signs Suggesting Serious/Emergent Conditions of the Shoulder
Following suggest a serious underlying pathology or emergency condition needing immediate attention.
- History of injury, convulsions or electric shock
- Any previous history of malignancy
- Any mass or selling on the shoulder
- Recent history of weight loss
- Fever and other systemic signs
- Redness of overlying skin erythema may suggest tumour or infection.
- Symptoms suggestive of polymyalgia rheumatic or giant cell arteritis.
- Loss of shoulder contour
- Neural deficit
- Shoulder deformity
- Crepitus
- Acute loss of function of shoulder
Diagnosis of Shoulder Pain
The physician when encountered with a case of shoulder pain needs to look for the following answers to be established
- What is source of pain – shoulder or something else?
- If shoulder is involved what is most likely condition responsible
Following history, examination and investigations are aimed at reaching at the diagnosis.
History
Establish whether the affected extremity is dominant or non dominant
- Details of pain
-
- How did pain start – acute or insidious
- Any precipitating activity
- Any history of injury.
- Effect of pain on daily life
- Is there a pain at rest
- Is the movement painful
- Is there any associated pain – for example, neck, chest or other upper limb or joint pain.
- Any previous history of shoulder instability or dislocation.
- Occupation.
- Whether one participates in overhead sports
- Any fever or other systemic sign
- Past medical history – diabetes, coronary heart disease, cancer or any other medical ailment
Examination
For shoulder pain, apart from shoulder adjoining areas such as the neck, axilla and chest wall should be examined as well.
For shoulder examination, the steps of examination are
- Inspection – Look for muscle wasting, swelling and deformity, or for bruising on all aspects of shouder. Compare with opposite shoulder
- Palpation – Palpate sternoclavicular, acromioclavicular and glenohumeral joints. Look for tenderness, swelling, warmth and crepitus.
- Assess the power, stability and range of movement (active, passive and resisted) in both shoulders. Specifically look for painful arc (pain between 70-120° of abduction).
Special Tests
Neer Test
The examiner performs maximal passive abduction in the scapula plane, with internal rotation, while scapula is stabilised.
This causes impingement of supraspinatus tendon against anterior inferior acromion.
Hawkins-Kennedy Test
With patient sitting, the the arm and elbow is flexed at to 90°, supported by the examiner. The examiner then stabilizes proximal to the elbow with their outside hand and with the other holds just proximal to the patient’s wrist. It is then quickly move the arm into internal rotation Pain and a grimacing facial expression indicate impingement of the supraspinatus tendon, and this is a positive Hawkins-Kennedy impingement sign.
Impingement Test
10 mL of a 1% lidocaine solution into the subacromial space and then repeats the tests for the impingement sign. Reduction of pain constitutes a positive impingement test result.
Drop Arm test
This evaluates for a supraspinatous muscle tear. In this test, shoulder is abducted 90 degrees, flexed to 30 degrees and point thumbs down. The test is positive if the patient is unable to keep arms elevated after the examiner releases.
Supraspinatus Isolation Test
It is also known as empty can and full can test. The original test described by Jobe and Moynes to test integrity of the supraspinatus tendon is called empty can test. Full Can Test was later suggested by Kelly as it was less provocative and tested in same manner.
Empty can and full can represent the position . The patient is tested at 90° elevation in the scapula plane and full internal rotation (empty can) or 45°external rotation (full can).
In these positions downward pressure exerted by examiner at patients elbow or wrist. Muscle weakness or pain or both represent a positive test.
Sulcus sign
In this test, the examiner grasps the patient’s elbow and applies downward traction. Dimpling of the skin below he acromion (the sulcus sign) indicates inferior humeral translation. This indicates instability of the shoulder joint.
Anterior Drawer Test
With patient in sitting position, one hand stabilizes the shoulder by holding coracoid and spine of scapula, and the other hand moves the humeral head anteriorly and posteriorly. Any abnormal movement is noted.
The Apprehension and Relocation Test
With patient in supine position, the examiner brings the affected arm into an abducted and externally rotated position. If patient apprehensively guards and does not allow further motion, it indicates a positive anterior shoulder instability.
The test is repeated with shoulder supported anteriorly. The absence of guarding and pain confirms the instability.
Cross Arm Test
This isolates the acromioclavicular joint. Ask the patient to raise the arm to 90° straight in front of them. Then ask the patient to adduct the arm across the chest. If there is an acromioclavicular joint problem, there will be pain in the area of the joint.
Investigations
Xrays are basic investigations. These help to rule out bony pathologies and injuries to the shoulder.
Ultrasonography might tell more about soft tissues in shoulder.
In desired cases where further imaging is required MRI is generally ordered as it provides a detailed view.
Lab investigations such as blood count, ESR, CRP may help in confirming presence of infection.
Treatment of Shoulder Pain
As a primary care of shoulder pain, following measures help –
- Decrease or stop overhead activities
- Drugs for relief of pain
- Hot/cold Compresses
Specific treatments are indicated for specific causes.
Rotator cuff Tendonitis
- Activity modification
- Analgesics such as NSAIDS
- Subacromial corticosteroid injection. Injections may be repeated if the initial response is good.
Rotator Cuff Tears
- Minor tears can be managed by physiotherapy and medication
- Larger tears need surgical treatment which could be involves arthroscopic rotator cuff tendon repair.
Calcific Tendonitis
- Drugs – NSAIDs, corticosteroids
- Physiotherapy
- Aspiration or surgical lavage.
- Open or arthroscopic excision of the deposits
Adhesive Capsulitis
- Drugs, steroid injections.
- Physiotherapy and exercises.
Arthritis Shoulder
For osteoarthritis of shoulder, refer to this article. General treatment is activity modification, drugs and occasional steroid injections. Topical analgesics also provide pain relief.
For rheumatoid arthritis, specific treatment of rheumatoid arthritis [DMARDs] is required along with other supportive measures
Patients who do not respond to conservative treatments may need surgery which is shoulder arthroplasty or fusion of the joint.
Acromioclavicular Conditions
- Injury usually responds to rest, simple analgesia and physiotherapy
- Significant disruption of the joint may require surgical fixation
Prognosis of Shoulder Pain
The prognosis of chronic shoulder pain depends on the underlying cause. Following factors are associated with worse outcome
- Higher age
- Female sex
- Chronic or recurrent symptoms
Shoulder pain is slow to recover and may take up to 18 months to recover in some cases.