Last Updated on November 10, 2019
Ankle arthrocentesis like other joint aspirations could be diagnostic or therapeutic. A good knowledge of ankle joint helps to perform the arthrocentesis more efficiently and safely.
Relevant Anatomy of Ankle Joint
The ankle joint is a hinged synovial joint formed by talar bone, tibia, and fibula. Plantar flexion and dorsiflexion are the main movements of the ankle joint.
[Detailed anatomy of ankle joint]
Indications of Ankle Arthrocentesis
Diagnostic
- Acute monoarticular [that affects a single joint] arthritis
- Suspected infection (eg, septic arthritis)
- Inflammatory joint effusion
- Gout
- Pseudogout
- Rheumatologic disorders
- Reactive arthropathies
Therapeutic
- To relieve a large painful effusion.
- Instillation of medications
- Repeated arthrocentesis for septic arthritis in carefully selected patients as a means of decreasing bacterial load
Contraindications
- Cellulitis in the overlying skin
- Overlying skin lesions (eg, dermatitis or psoriasis)
- Known bacteremia
- Bleeding disorders
- Patient on anticoagulation medication
Procedure of Ankle Arthrocentesis
- The patient is either in the sitting position or supine on a stretcher, with the knee flexed at 90º. The leg may hang from the side of the stretcher or bent with the heel resting against the stretcher.
- After skin preparation, draping, and identification of the needle insertion site, lidocaine 1% is used as local anesthetic into the subcutaneous tissue. Be careful not to go too deep or otherwise the anesthetic agent could be instilled in the joint. Anxious and uncooperative patients may need sedation.
- Anterolateral approach
- Preferred approach
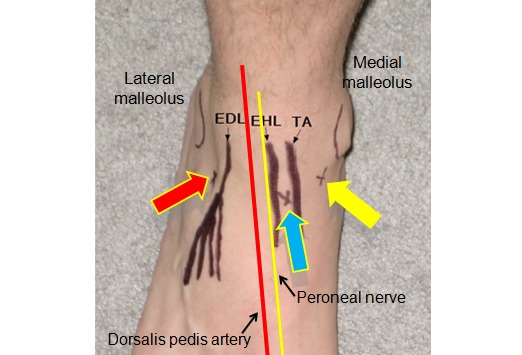
- Avoids potential injury to the dorsalis pedis and posterior tibial vessels or the deep peroneal nerve. These structures course through the medial aspect of the ankle and foot.
- The needle is inserted at the joint line midway between the base of the lateral malleolus and the lateral border of the extensor digitorum longus, advancing the needle perpendicular to the fibular shaft.
- Anteromedial approach
- Identify the ankle joint line, the medial malleolus, and the tendons of the extensor hallucis longus and the tibialis anterior. [To avoid injury to both the dorsalis pedis vessels and the deep peroneal nerves, remember these structures are immediately below and lateral to the extensor hallucis longus tendon.
- Identify the space
- Between the medial border of the extensor hallucis longus and the lateral border of the tibialis anterior or
- Between the base of the medial malleolus and the medial border of the tibialis anterior.
- Insert a needle at either insertion point in either of the spaces and advance the needle perpendicular to the tibial shaft.
- Repeated flexion/extension movement by the patient helps the identification of the spaces in either approach.
- Inverting and plantar flexing helps to identify space in anteromedial approach
- Using a sterile technique, attach the 18- or 20-gauge needle to the 20-mL syringe, and pull the plunger to break resistance.
- Insert the needle into the joint space while gently aspirating until synovial fluid enters the syringe (usually 1-2 cm)
- If a bone is encountered, pull the needle back, verify the anatomic landmarks and readvance the needle in a corrected direction.
- If removal of more fluid is desired, a hemostat can be used to secure the needle in place while the syringe is replaced with a new one.
- Remove the needle and apply a bandage.
- Divide the aspirated synovial fluid into the different specimen containers for synovial fluid analysis
Complications of Ankle Arthrocentesis
Dry tap
Dry tap causes are
- Improper needle placement
- Small amount of effusion
- Mechanical obstruction of the needle against cartilage
- Thickened synovium
Cartilage Injury
Infection
Intravenous antibiotics should be given immediately following the procedure when the infective focus is suspected.