Last Updated on February 12, 2024
Joint Hypermobility Benign Joint Hypermobility Syndrome
Joint hypermobility or double-jointedness is said to be present when a joint that can be stretched beyond what is called normal range is normal.
When generalized joint hypermobility is present with symptoms of muscle and joint pain, it is termed joint hypermobility syndrome.
Joint hypermobility could be due to
- Malaligned joints
- Joint with the abnormal shape of articular surfaces
- Connective tissue disorder (such as Ehlers-Danlos syndrome, Marfan syndrome)
- Abnormal joint proprioception
- Familial-joint hypermobility can run in families suggesting a genetic basis too.
Most of people with joint hypermobility do not have any problem but others especially those in sports may become prone to repeated joint injuries.

Benign joint hypermobility syndrome, thought to be a connective tissue disorder, is the occurrence of pain in multiple joints in hypermobile individuals in the absence of systemic rheumatologic disease.
The entity is different from the disorders that cause local joint hypermobility and generalized joint laxity, such as Marfan syndrome and Ehlers–Danlos syndrome.
Benign joint hypermobility syndrome has a strong genetic component with an autosomal dominant pattern.
Beighton Score For Joint Hypermobility
The Beighton score is used for assessing the presence of joint hypermobility. However, it must be noted that the diagnosis of Hypermobility Syndrome or HMS should be made using the Brighton Criteria.
Beighton scoring is based on testing the simple movements.
- Passive Dorsiflexion of Little Finger: In a normal individual, the little finger cannot be extended beyond 90 degrees, even passively- Score 0. If the passive extension [dorsiflexion] reveals this movement beyond 90 degrees – Score 1
- Passive Dorsiflexion of Thumb: If the thumb cannot be made to touch the flexor aspect of the forearm – Score 0. If the thumb can be made to touch the flexor aspect of the forearm – Score 1
- Hyperextension of the elbow: The common range of movement of the elbow is 0-120 degrees.( 0 signifies that arm can be made to straighten but a further movement is not possible. Any further extension movement of the elbow would result in arm bending backward.) Some normal individuals may have a slight backward bending movement. A cut-off point of 10 degrees is kept to look for a hypermobile joint.
If the elbow cannot be bent backward is less than 10 degrees [has less than 10 degrees of extension – Score 0
If the elbow can be bent backward more than 10 degrees [has more than 10 degrees of extension] – Score 1 - Hyperextension of Knee: The concept of the elbow, when applied to the knee, would provide scores of the knee In a normal individual, the knee can not be straightened beyond 0 degrees. Further extension is known as hyperextension.
Hyperextension of right knee beyond 10 degrees not present – Score 0
Hyperextension of right knee beyond 10 degrees present – Score 1 - Trunk Flexion: The individual is not able to rest the palms and hands on the floor with forward flexion [bending] of the trunk with knees fully extended – Score 0
The individual can rest the palms and hands on the floor with forward flexion [bending] of the trunk with knees fully extended – Score 1
The score is calculated by adding the scores of
- Both the thumbs
- Both the little fingers
- Both elbows
- Both knees
- One Trunk Movement
The maximum possible score thus becomes 9
A 4/9 score is considered significant.
Brighton Criteria For Benign Joint Hypermobility Syndrome
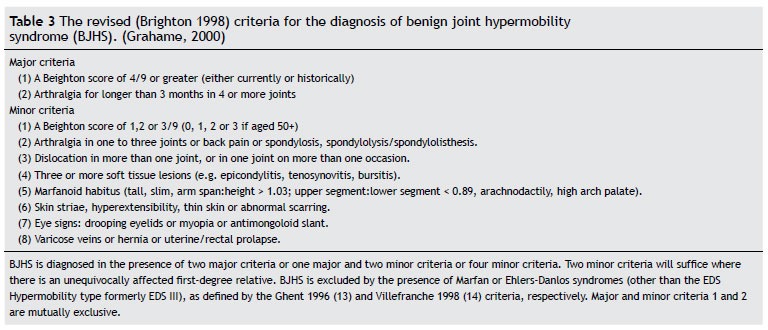
Major Criteria
- A Beighton score of 4/9 or greater (either currently or historically)
- Arthralgia >3 months in 4 or more joints
Minor Criteria
- A Beighton score of 3 or less
- Arthralgia (> 3 months) in one to three joints or back pain (> 3 months), spondylosis, spondylolysis/spondylolisthesis.
- Dislocation/subluxation in more than one joint, or in one joint on more than one occasion.
- Soft tissue rheumatism. > 3 lesions (e.g. epicondylitis, tenosynovitis, bursitis).
- Marfanoid habitus (tall, slim, span/height ratio >1.03, upper: lower segment ratio less than 0.89, arachnodactyly [positive Steinberg/wrist signs].
- Abnormal skin: striae, hyperextensibility, thin skin, papyraceous scarring.
- Eye signs: drooping eyelids or myopia or antimongoloid slant.
- Varicose veins or hernia or uterine/rectal prolapse.
The diagnosis of benign joint hypermobility syndrome is made if
- Two major criteria are present or
- There are one major and two minor criteria present or
- Four minor criteria are present
Pathophysiology of Benign Joint Hypermobility Syndrome
The cause is not clearly understood but the following factors have been suggested –
- The shape of the ends of the bones results in joint wear and tear
- Impaired proprioception
- Fatigue of surrounding tissues
Clinical Presentation
Pain in a hypermobile joint which may affect one or multiple joints is the most common symptom. This can occur at any age are often exacerbated by physical activity. Though it may occur in any joint but knee and ankle are most commonly involved.
Other symptoms that may occur are joint stiffness, myalgia, muscle cramps, and nonjoint limb pain.
There might be a history of double-jointedness or recurrent dislocations in the family. Easy bruising, ligament or tendon rupture, congenital hip dysplasia, and temporomandibular joint dysfunction may be associated findings.
On physical examination, there might be pain in joints during manipulation.
Other associated findings that might be present are [Suggesting some connective tissue disorder]
- Scoliosis
- Pes planus
- Genu valgum
- Lordosis
- Marfanoid habitus
- Varicose veins
- Rectal or uterine prolapse
- Thin skin
People with benign joint hypermobility syndrome may develop other conditions caused by their unstable joints. These conditions include frequent sprains, tendinitis, or bursitis when doing activities that would not affect the normal individual.
Diagnosis
Diagnosis of benign joint hypermobility syndrome is one of exclusion. Other causes like inflammatory, infectious, and autoimmune causes should be ruled out. Routine work should include
- Complete blood cell count
- Erythrocyte sedimentation rate
- Rheumatoid factor
- Antinuclear antibody tests
- Serum complement levels
- Serum immunoglobulin levels
By rule, all of these are within normal limits in benign joint hypermobility syndrome. Synovial fluid evaluation in case of joint effusion shows a noninflammatory pattern from meniscal and cartilage irritation.
Determining the Beighton score which is a measure of generalized joint laxity is essential for diagnosis making.
A Beighton score of 4 or more points is considered indicative of generalized joint laxity.
Brighton criteria which is based on the Beighton score helps to establish the diagnosis of benign joint hypermobility syndrome and also helps to distinguish it from other connective tissue disorders.
Treatment of Benign Joint Hypermobility Syndrome
Many individuals with benign joint hypermobility syndrome improve in adulthood. Treatments are individualized based on the manifestations.
The treatment of benign joint hypermobility syndrome consists of
- Lifestyle modification
- Change In Exercise Pattern
- Protection of joints
- Medication
Nonsteroidal anti-inflammatory drugs are used for pain control. Restraining from aggravating activities can relieve the symptoms.
In the long term, modification of activities that induce symptoms is part of the treatment. Vigorous and repetitive activities should be curtailed.
Patients need to be taught about the condition they have. Overtraining, poor pacing, too many performances or athletic competitions, and focusing on joint flexibility rather than stability may all increase joint pain and the risk of injury.
They should be avoided. But it cannot be possible in all cases [for example athletes] and alternatives can be explored.
Individuals with hypermobility must remain extremely fit – even more so than the average individual – to prevent recurrent injuries. Regular exercise and physical therapy or hydrotherapy can reduce symptoms of hypermobility because strong muscles help to stabilize joints.
Strengthening program to provide muscular stability and stabilization to the joint may be beneficial. Stretching techniques that are targeted to isolate tight muscles without stressing the surrounding joints may reduce symptoms.
Supportive splints along with appropriate footwear protect the joint, and supportive joint taping can improve joint proprioception.