Last Updated on November 22, 2023
Posterior cruciate ligament injury or PCL injury is less common than the anterior cruciate ligament injury. A posterior cruciate ligament tear may result in disability ranging from no impairment to severe impairment.
The primary function of the PCL is to prevent posterior translation of the tibia on the femur. The posterior cruciate ligament is also important in providing and controlling rotational stability to the knee.
True incidence of the injury is not known. It constitutes 5-20% of all knee ligamentous injuries.
Injuries may be isolated or combined and often go undiagnosed in the acutely injured knee.
Relevant Anatomy
Read more about knee anatomy
Read more about knee ligaments
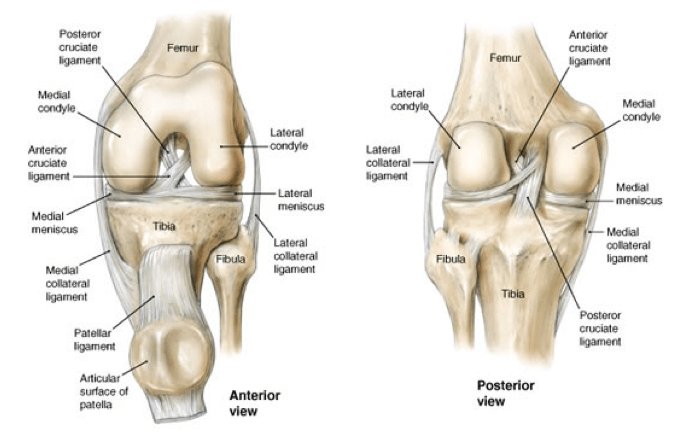
Posterior cruciate ligament an extrasynovial structure that lies behind the intra-articular portion of the knee.
Posterior cruciate ligament originates from posterior tibial sulcus below the articular surface [posterior aspect of the tibial plateau, on a depression between the tibial plateaus, extending 1 cm below the articular surface] and inserts into anterolateral medial femoral condyle by a broad, crescent-shaped attachment.
It is 38 mm in length and 13 mm in diameter, thus larger than anterior cruciate ligament.
It has an anterolateral bundle that tightens in flexion. It is the strongest of the two and is most important for posterior stability at 90° of flexion.
The other bundle is posterolateral bundle which gets tightened in extension.
Thus, its function is reciprocal to the anterolateral bundle.
Posterior cruciate ligament lies between meniscofemoral ligaments [Ligament of Humphrey (anterior) and ligament of Wrisberg (posterior)] which originate from the posterior horn of the lateral meniscus and insert variably into PCL substance
Blood supply to a posterior cruciate ligament is by branches of the middle geniculate artery and fat pad.
Biomechanics and Pathophysiology
The strength of the posterior cruciate ligament is 2500 to 3000 N. It minimizes posterior tibial displacement of the knee by acting as primary restraint to posterior tibial translation.
It also prevents hyperflexion/sliding. Isolated injuries are known to cause the greatest instability at 90° of flexion.
Most of the PCL injuries occur by a direct blow to direct blow to proximal tibia with a flexed knee as in dashboard injury, during a football tackle.
Both these examples result in a posteriorly directed force and a varus hyperextension force, leading to a posterolateral cruciate ligament injury and posterolateral capsular ruptures.
The injury may also result from noncontact hyperflexion with a plantar-flexed foot. Hyperextension injury is also known.
The injuries can occur in isolation but may be associated with posterolateral corner (PLC) injuries, multiligamentous knee injuries and knee dislocation
A deficient chronic posterior cruciate ligament leads to increased contact pressures in the patellofemoral and medial compartments of the knee due to varus alignment.
Classification of Posterior Cruciate ligament Injury
The classification is based on posterior subluxation of the tibia relative to femoral condyles (with the knee in 90° of flexion)
Grade I (Partial)
- Limited damage to the ligament. Indicates microscopic tears in the ligament.
- 1-5 mm posterior tibial translation
- Tibia remains anterior to the femoral condyles
Grade II (Complete isolated)
Mild instability present
Shows isolated complete injury
- 6-10 mm posterior tibial translation
- complete injury in which the anterior tibia is flush with the femoral condyles
Grade III (Combined Injury)
- >10 mm posterior tibial translation
- tibia is posterior to the femoral condyles and often indicates an associated ACL and/or PLC
- Combined PCL and capsuloligamentous injury
Clinical Presentation
A patient can present as acute or chronic injury.
Both have different presentations.
In an isolated acute posterior cruciate ligament injury, the symptoms will often be vague and minimal. The patient may or may not complain of pain. There is hardly any swelling, instability, and decrease in range of motion.
The gait pattern would also be normal.
When the injury is in combination with other ligamentous injuries, there would be variable swelling and in the knee. The patient may complain of knee instability and stiffness of the knee.
In chronic presentation, a history of injury may or may not be available.
Vague discomfort of the knee is a common presentation especially during weight bearing in flexion such as ascending or descending stairs or squatting.
Discomfort may be experienced with the following positions or activities:
- A semiflexed position, as with ascending or descending stairs or an incline
- Starting a run
- Lifting a load
- Walking longer distances
Long walks may cause pain/discomfort of the knee. There could be a sense of instability especially when walking on an uneven surface.
Swelling and stiffness depend on the degree of associated chondral damage.
Retropatellar pain symptoms may be reported as a result of posterior tibial sagging. Medial joint line pain may be reported.
Special Tests
Varus/valgus stress
This test is done to check laxity in response to varus valgus forces.
The comparison should be made to the opposite side.
Laxity at 0° indicates medial collateral ligament and posterior cruciate ligament injury.
But laxity at 30° alone indicates Medial or lateral collateral ligament injury of only.
Posterior Tibial Sag
The basis of the test is that the medial tibial plateau of a normal knee at rest is 10 mm anterior to the medial femoral condyle. A posteriorly-directed tibial step-off indicates a positive sign
The patient lies supine with hips and knees flexed to 90°, the examiner supports ankles and observes for a posterior shift of the tibia as compared to the uninvolved knee. In such a position, gravity pulls posteriorly on the tibia, and in the case of PCL disruption, the tibia falls even or behind the femoral condyles. The comparison should be made to the opposite knee.
Posterior sag sign can be observed in extension too.
With the patient in supine, the examiner supports both of the patient’s heels simultaneously with legs in full extension.
A posterior sag on the injured side indicates injury to the posterior cruciate ligament and some secondary restraint like medial collateral ligament, lateral collateral ligament, posterolateral corner.
A patient with positive posterior tibial sag may also have false-positive Lachman and anterior drawer tests.
Positive quadriceps active test
The patient is placed supine with the knee flexed to 90 degrees and the foot placed flat on the examining table.
[In intact PCL, in this position with the quadriceps relaxed, the tibia is 10 mm anterior to the femoral condyles.
The gravity pulls the tibia even or behind the femoral condyles when quadriceps relaxed.]
The examiner restrains the ankle from moving, and the patient is asked to contract the quadriceps.
When tibia is deficient and pulled, the contraction of the quadriceps has to lift the tibia forward. If the tibia moves forward more than 2 mm, the quadriceps active test is positive.
Posterior drawer test
It is the most accurate test for diagnosis of posterior cruciate ligament injury.
The patient is placed supine with both knees flexed to 90° and the feet in neutral rotation placed flat on the table. The normal tibial plateau in this position is about 10 mm anterior to the femoral condyles.
The examiner imparts a posterior force to the proximal tibia, and if the tibial displacement is noted and compared for side to side asymmetry.
This test is also used to grade the injury. [see classification]
By rotating the foot, the posterior drawer test can test other structures too.
- Internal rotation, the PCL and tibial collateral ligaments are tested.
- External rotation, the PCL, LCL, and posterolateral corner are tested.
Assessment of the posterolateral corner
[Read more about PLC Injury]
Assessment of PLC is important as injury to PLC combined with PCL has a worse prognosis than PCL alone.
Reverse pivot shift test
The reverse Pivot shift test begins with patient supine with the knee in 90 degrees of flexion.
Valgus stress is then applied to the knee with an external rotation force and the knee is brought into full extension from the previous flexion.
This maneuver would make tibia reduce from the posterior subluxed position at about 20 degrees of flexion, as it moves anteriorly, felt as a clunk.
[Note: The true Pivot shift test is seen in ACL injury]
The reverse Pivot shift test helps to diagnose acute or chronic posterolateral instability of the knee.
Posterolateral Drawer Test in 90° of Flexion
This test is performed with the patient sitting with thighs supported by the examining table and legs lying off the end of the examining table.
The examiner performs a posterior drawer test. If the posterolateral structures are injured, the lateral tibial plateau rotates posteriorly as the posterior force is applied.
External Rotation Recurvatum Test
The test is done similar to the posterior sag sign, except the examiner notices significant subluxation of the lateral tibial plateau.
Dial Test
This test is done in prone or supine position. The external rotation at the knee joint is noted while the knees are at 30° and 90° of flexion by measuring the foot-thigh angle.
In the prone position, the clinician flexes the patient knees to 30° and places both hands on the feet of the patient, cupping his heels. A maximal external rotation force is then applied, and the foot-thigh angle is measured and compared with the other side. The knees are then flexed to 90°, and again an external rotation force is applied and the foot-thigh angle is measured again
In the other method, the knee is flexed over the side of the bed. The thigh is stabilized and external rotation force is applied.
The measurement is compared with the uninjured knee.
-
-
- > 10° ER asymmetry or difference from opposite knee at 30° & 90° consistent with PLC and PCL injury
- > 10° ER asymmetry at 30° only consistent with isolated PLC injury
-
Differential Diagnoses
- Anterior Cruciate Ligament Injury
- Lateral Collateral Knee Ligament Injury
- Medial Collateral Knee Ligament Injury
- Meniscus Tears
- Talofibular Ligament Injury
Lab Studies
No special tests are needed. Special tests as required can be done.
Imaging
X-rays
X-rays help to rule out bony lesions but are normal in most of the cases of acute injuries.
In chronic injuries, medial joint arthrosis or patellofemoral arthrosis may be seen.
Lateral stress view of the knee is fast becoming an easy method to diagnose and quantify posterior cruciate ligament injuries.
For this x-ray, stress is applied to the anterior tibia with the knee flexed to 70°. X-rays are taken for both the knees. Asymmetric posterior tibial displacement indicates PCL injury.
Differences >12 mm on stress views suggest a combined PCL and PLC injury
Magnetic Resonance Imaging
MRI helps identify and confirm the location of the lesion. It also identifies occult osteochondral lesion/fractures and meniscal lesions.
It can visualize completeness of the tear and MRI is used to identify whether the tear is complete or incomplete and whether the PCL injury is isolated or associated with injury to other structures.
The sensitivity and specificity of MRI in acute PCL injury is high.
MRI may be normal in grade I and II tears.
It must be noted that many isolated posterior cruciate ligament injuries are missed at the time of initial injury especially the isolated ones as the patient does not seek medical attention immediately and does not remember the initial mode of injury and signs present are minimum/equivocal.
In such situations, MRI is the best method for evaluation of the injury.
Arteriograms
An arteriogram should be performed in case of vascular injury.
Arthroscopic posteromedial Drive-through Test
The test is considered positive if it is easy to pass the arthroscope between the medial femoral condyle and the PCL.
Treatment of Posterior Cruciate Ligament Injuries
Non-operative treatment
Non-operative treatment consists of symptomatic treatment, local RICE measures followed by protected weight bearing & rehabilitation.
It is indicated in isolated Grade I and II injuries. Some grade III can be considered as well.
Electrical stimulation and cold whirlpool may be used to control swelling and inflammation.
Patients with grade I and grade II injuries can bear weight as tolerated immediately with or without support, varying from individual to individual.
Axillary crutches and a long leg brace are recommended for grade III injuries and with another associated ligamentous laxity (ie, posterolateral corner injury) or intra-articular damage.
Details of rehabilitation are given below.
1-14 days
- Quadriceps and hip strengthening
- Avoid open kinetic chain hamstring exercises as these cause posterior tibial translation at the knee.
14-21 days
- Grade III injuries continue to wear a brace followed by a functional knee brace.
- Progressive w and gradual discontinuation of crutches.
- Light resistance exercises as tolerated.
- Range of Motion exercises
- Bicycling
- Aquatic exercises
3 weeks and Further
Progression to closed kinetic chain exercises like leg press, mini squats, stair stepper, step-ups).
Gradual increase of resistance and strengthening exercises.
Light jogging program may be initiated.
Operative treatment
The surgical treatment employed would depend on the nature of the injury, duration since the injury and any arthritic changes.
The results of operative reconstruction are variable and sometimes not better than nonoperative treatment.
Ligament Repair/ Reconstruction
This may include repair of the ligament or fixation of the bony avulsion or reconstruction.
It is indicated in
- Combined ligamentous injuries
-
- PCL + ACL or PLC injuries
- PCL + Grade III MCL or LCL injuries
- Isolated Grade II or III injuries with bony avulsion
- Isolated chronic PCL injuries with a functionally unstable knee
- Persistent pain, instability, or disability despite conservative treatment
Bony posterior cruciate ligament avulsion injuries are amenable to surgical repair of the avulsed bony fragment.
For reconstruction, the graft is used which could be single bundle or double bundle depending on the graft used.
The reconstruction can be tibial inlay [open technique] or transtibial [arthroscopic technique].
Autograft
-
- Patellar tendon
- Quadriceps tendon
- Hamstring tendons
- Medial head of gastrocnemius
Allograft
-
- Achilles tendon
- Patellar tendon
- Quadriceps tendon
- Hamstring tendons
High Tibial Osteotomy
High tibial osteotomy is indicated in chronic PCL deficiency with joint changes. Medial wedge osteotomy to treat both varus malalignment and PCL deficiency.
Increase in tibial slope during osteotomy also reduces the posterior sag of the tibia.
Postoperative Rehabilitation
1-7 days
- Cold therapy, compression, and elevation in the immediate postoperative period.
- Assisted weight bearing with crutches and long leg brace.
- Mobilization exercises for the knee to prevent scar and fibrosis.
- Range of motion exercises for knee leg ankle and hip joint
Further rehabilitation
- Progressive weight bearing is progressed as tolerated
- Gradual discontinuation of crutches
- Functional knee brace at 4-6 weeks after removal of a long leg brace
- Strengthening exercises
- Proprioception exercises
Athletes may return to play when isokinetic and functional parameters are satisfactory..
Complications
- Instability
- Progressive arthritis
- Postoperative complications
Prognosis
Prognosis of posterior cruciate ligament injuries treated nonoperatively is quite good. 84% had returned to their previous sport. But 68% have the same level of performance, about 16% at a decreased level of performance.
Good results achieved with primary repair of bony avulsions
Primary repair of midsubstance ruptures is typically not successful.
When compared to ACL, the results of PCL and residual posterior laxity often exists.
Concomitant ligament injuries worsen the prognosis.
No clear difference has been found to support one reconstruction technique over the other.
References
- Sheps DM, Otto D, Fernhout M. The anatomic characteristics of the tibial insertion of the posterior cruciate ligament. Arthroscopy. 2005 Jul. 21(7):820-5.
- Amis AA, Gupte CM, Bull AM, Edwards A. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2006 Mar. 14(3):257-63.
- Servant CT, Ramos JP, Thomas NP. The accuracy of magnetic resonance imaging in diagnosing chronic posterior cruciate ligament injury. Knee. 2004 Aug. 11(4):265-70.
- Nha, KW, Bae, JH, Kwon, JH, et al. Arthroscopic posteromedial drive-through test in posterior cruciate ligament insufficiency: a new diagnostic test. Knee Surg Sports Traumatol Arthrosc. February 2014.
- Lenschow S, Zantop T, Weimann A, Lemburg T, Raschke M, Strobel M. Joint kinematics and in situ forces after single bundle PCL reconstruction: a graft placed at the center of the femoral attachment does not restore normal posterior laxity. Arch Orthop Trauma Surg. 2006 May. 126(4):253-9.
- Kim SJ, Kim TE, Jo SB, et al. Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques. J Bone Joint Surg Am. 2009 Nov. 91(11):2543-9
- Ahn JH, Nha KW, Kim YC, Lim HC, Nam HW, Wang JH. Arthroscopic femoral tensioning and posterior cruciate ligament reconstruction in chronic posterior cruciate ligament injury. Arthroscopy. 2006 Mar. 22(3):341.e1-4.
- Hermans S, Corten K, Bellemans J. Long-term results of isolated anterolateral bundle reconstructions of the posterior cruciate ligament: a 6- to 12-year follow-up study. Am J Sports Med. 2009 Aug. 37(8):1499-507.
- Bergfeld JA, McAllister DR, Parker RD, et al. The effects of tibial rotation on posterior translation in knees in which the posterior cruciate ligament has been cut. J Bone Joint Surg Am. 2001 Sep. 83-A(9):1339-43.
- Cosgarea AJ, Jay PR. Posterior cruciate ligament injuries: evaluation and management. J Am Acad Orthop Surg. 2001 Sep-Oct. 9(5):297-307.
- Delee JC. Orthopaedic Sports Medicine, Principles and Practice. Philadelphia, Pa: WB Saunders Co; 1994. Vol 2:
- Veltri DM, Warren RF. Isolated and combined posterior cruciate ligament injuries. J Am Acad Orthop Surg. Nov 1993. 1(2):67-75.