Last Updated on November 22, 2023
Anterior cruciate ligament injury is a very common injury of the knee. It may occur in isolation or along with other soft tissue or bony injury of the knee.
Anterior cruciate ligament injury or ACL injury most commonly results from a low velocity, noncontact deceleration injuries or pivoting injuries and contact injuries with a rotational component.
50% of the injured ACLs also have meniscal tears.
The incidence of ACL injury is higher in people who participate in high-risk sports such as basketball, football, skiing, and soccer.
The anterior cruciate ligament provides stability in running, cutting and kicking.
Knees which are deficient in anterior cruciate ligament are associated with chondral injuries, complex unrepairable meniscal tears.
Anterior cruciate ligament injury is common in young persons. Age of getting an ACL injury is younger in females than males [female athletes are generally younger].
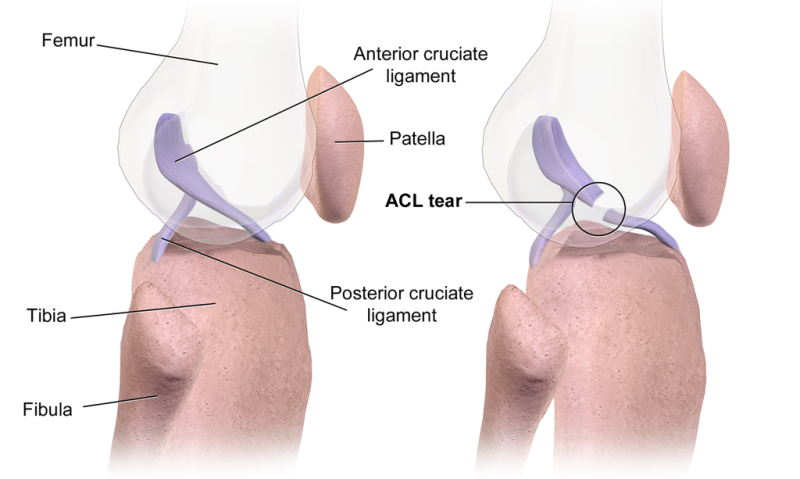
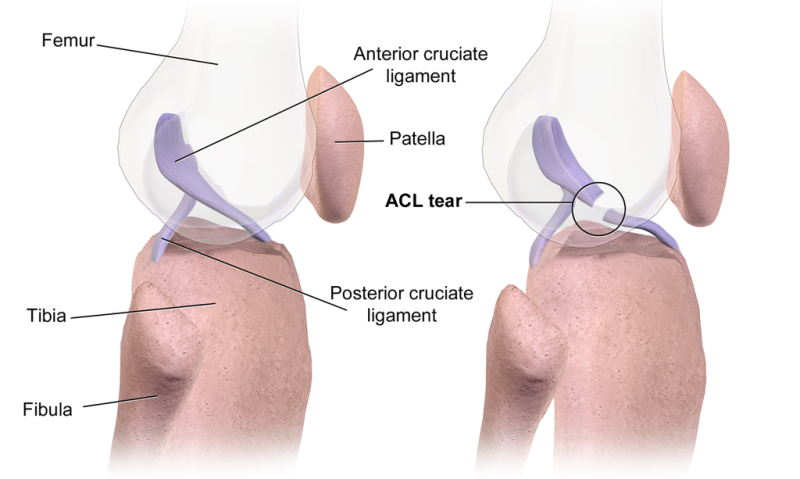
Relevant Anatomy
The anterior cruciate ligament is intracapsular and extrasynovial. It courses anteriorly, medially, and distally as it runs from the femur to the tibia.
Anterior cruciate ligament arises from the posteromedial corner of the medial aspect of the lateral femoral condyle in the intercondylar notch. It attached by interdigitation of collagen fibers & rigid bone through the transitional zone of fibrocartilage and mineralized fibrocartilage.
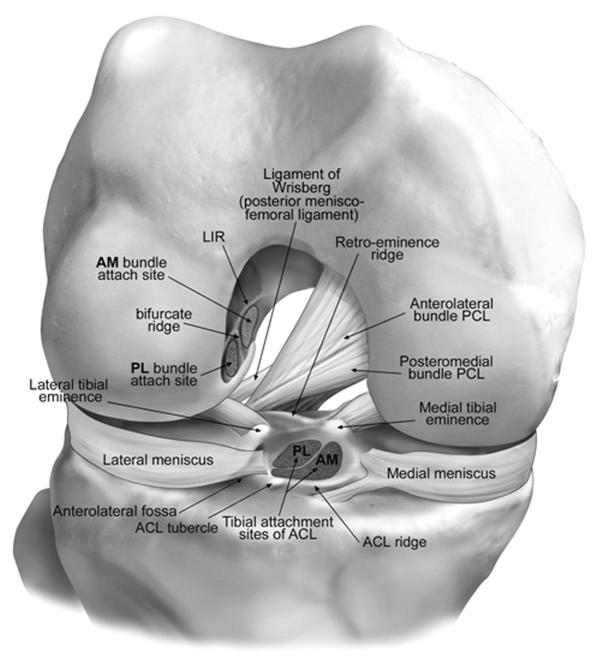
Femoral attachment is on the posterior part of the medial surface of lateral condyle well posterior to a longitudinal axis of the femoral shaft whereas the tibial attachment is in a fossa in front of & lateral to anterior spine. Anterior fibers also insert into the interspinous area of the tibia and towards transverse meniscal ligament.
Tibial attachment is 11-17 mm in width in the anteroposterior direction in AP direction.
The ligament has a small anteromedial band or bundle and a larger bulky posterolateral band. The anteromedial bundle is tight in flexion and the posterolateral bundle is tight in extension.
In extension both the bands are parallel whereas in flexion both the bands are crossed as insertion site of posterolateral band move anteriorly.
In extension anteromedial band tightens and posterolateral bundle loosens.
Posterolateral bundle represents posteriorly directly directed fibers and is attached just lateral to the midline of the intercondylar eminence and slightly lateral to most lateral attachment of the other bundle. It limits anterior translation, hyperextension, and rotation. It provides resistance to the anterior drawer test in the extended knee.
The posterolateral bundle provides more rotational control than the anteromedial bundle, the latter being more axial.
This band is less isometric and undergoes more length changes.
Hyperextension and internal rotation place the posterolateral bundle at greater risk for injury.
Anteromedial bundle inserts on the medial aspect of the intercondylar eminence of the tibia and acts as a primary check against anterior translation of the tibia on femur [as in drawer test in flexion].
The anteromedial band has isometric behavior as compared to posterolateral and its femoral insertion is the center of rotation of ACL.
Length of ACL is about the length of 38 mm (25 – 41 mm) and width is 10 mm (range 7 to 12 mm). Structurally, it is composed of multiple collagen fascicles surrounded by an endotendineum
Nerve supply is from posterior tibial nerve which infiltrates the capsule posteriorly. The main function is proprioception.
Majority of the blood supply is from the middle genicular artery.
The anterior cruciate ligament is composed of 90% Type I collagen and 10% Type III collagen.
Biomechanics and Mechanism of Injury
The anterior cruciate ligament is responsible for primary (85% contribution) restraint to limit anterior translation of the tibia. The greatest restraint is in full extension.
The ACL also serves as a secondary restraint to the tibial rotation and varus/valgus angulation at full extension.
The average tensile strength for the ACL is 2160 N. This is slightly less than the strength of the posterior cruciate ligament and approximately half as strong as the medial collateral ligament (MCL).
The broad mechanism of injury is Mechanism is a non-contact pivoting injury
The ACL is usually torn as a result of a quick deceleration, hyperextension or rotational injury [non-contact injury]. This injury often occurs following a sudden change of direction. A person typically reports feeling a popping sensation in the knee. When hit from the side, injuries to the ACL are often associated with medial meniscus and medial collateral ligament) tears [unhappy or terrible triad].
In adolescents, the ACL may avulse from the tibial spine instead of be rupturing.
Risk factors for Anterior Cruciate Ligament Injury
High-risk sports
High-risk sports are football, baseball, soccer, skiing, and basketball which account for up to 78% injuries related to sports.
Gender
Female athletes are more susceptible to ACL injuries. The factors responsible for the increased occurrence of ACL injury in females are
- The difference in landing biomechanics
- Females land with their knees in more extension and valgus due to the hip internal rotation
- Structural Differences
- smaller notches
- smaller ACL size
- Cyclic hormonal levels
- Greater risk for injury during the first half (preovulatory phase) of the menstrual cycle
- Neuromuscular Differences
- Lower hamstring quadriceps ratio
- Weaker core stability
- Genetic
- underrepresentation of COL5A1 gene sequence in females with ACL ruptures.
- The gene is collagen producing.
Femoral Notch Stenosis
It is defined as the ratio of the femoral notch width to the width of the femoral condyles.
The value less than 0.2 is defined as notch stenosis.
Individuals with notch stenosis have a higher risk of noncontact ACL injuries.
Footwear
Cleats on artificial turf are known to be associated with a higher incidence of ACL injuries.
Clinical Presentation of Anterior Cruciate Ligament Injury
In case of acute non-contact injury, the patient may report a popping sound. Often hemarthrosis develops [70%]. Usually, the patients are unable to return to play due to pain, swelling, and instability or giving way of the knee.
Contact injuries are generally part of a larger injury profile and are associated with other ligamentous and meniscal injuries.
In chronic cases, the patient may seek consultation because of the instability of the knee experienced. The patient may report knee giving way or wobbliness of the knee, especially when walking on rough surfaces.
In acute cases, the examination may be very limited due to pain, apprehension and guarding by the patient.
There may be quadriceps avoidance gait [patient does not extend the knee]
The knee is examined for effusion or bony abnormality.
Palpation of bony structures may suggest an associated tibial plateau fracture or meniscal tear.
Palpation over the collateral ligaments may reveal sprain. Ligamentous laxity may be difficult to detect in the acute situation.
Range of motion is assessed and noted for lack of complete extension [suggests possible associated meniscus tear or associated loose fragment.]
Lachman test
It is the most sensitive test for acute ACL tear.
For this test, the knee is placed in a position of 20-30° of flexion. The femur is stabilized with a nondominant hand, and an anteriorly-directed force is applied to the proximal calf.
Two things are assessed
- Amount of displacement (in mm)
- Quality of endpoint is assessed
- Firm
- Marginal
- Soft
Asymmetry in side-to-side laxity or a soft endpoint is indicative of an ACL tear. A side-to-side difference of greater than 3 mm is considered abnormal.
Grading [A= firm endpoint, B= no endpoint]
- Grade 1: 3-5 mm translation
- Grade 2 A/B: 5-10mm translation
- Grade 3 A/B: > 10mm translation
PCL tear may give “false” Lachman due to posterior subluxation
Pivot shift test
In an ACL-deficient knee, a small amount of anterior translation of the tibia in relation to the femur occurs. During flexion, the translation reduces, resulting in the shifting of the tibia back into its proper alignment.
For performing the test, with the leg extended, the foot in internal rotation, a valgus stress is applied to the tibia. Flexion causes a reduction of the anteriorly subluxed tibia at approximately 20-30° mimicking actual give away event.
Anterior drawer test
The test may be influenced by hamstring spasm in the acutely injured knee; thus, this test is considered the least reliable.
This test is performed with the patient supine and the knee flexed to 90°. The examiner can sit on the patient’s foot and grasp around the patient’s calf with both hands. An anterior force is applied, and the tibial excursion is compared to the unaffected knee.
KT-1000 Arthrometer
The KT-1000 test is performed to provide an objective assessment of the amount of increased anterior knee translation between 20 and 30 degrees of knee flexion.
It compares the difference in tibial excursion between the injured and the unaffected knee of a patient.
An excursion greater than 3 mm as measured by the KT-1000 is classified as pathologic.
Differential Diagnoses
- Medial Collateral Knee Ligament Injury
- Posterior Cruciate Ligament Injury
Lab Studies
Lab studies are not generally required for the diagnosis of ACL tear. In acute cases, arthrocentesis may reveal blood with fat globules indicating an osteochondral or tibial fracture. But knee aspiration is rarely done
Imaging
Plain radiographs
X-rays are usually normal but are helpful to reveal bony injuries or instability.
Anteroposterior, lateral, merchant, sunrise views are done.
Notch view can be done to assess the femoral notch adequacy.
Important radiological Signs on X-rays
Segond Fracture
Segond fracture is lateral capsular avulsion fracture and represents a disruption of the meniscotibial portion of the lateral capsule due to bony avulsion the anterolateral ligament.
It provides a direct evidence of a lateral capsule injury and indirect evidence of an ACL injury.
It is associated with ACL tear 75-100% of the time
Some consider Segond fracture to be pathognomonic for an ACL tear
Deep Lateral Sulcus Sign or Deep Sulcus (terminalis) Sign
This refers to a depression on the lateral femoral condyle at the terminal sulcus, a junction between the weight-bearing tibial articular surface and the patellar articular surface of the femoral condyle.
Anterior Tibial Translocation or Translation
It is also called the anterior drawer sign. It refers to anterior tibial subluxation) of the tibia relative to the femur of more than 7 mm. It signifies complete rupture of the anterior cruciate ligament.
Arcuate Sign
The avulsion fracture is usually small, <1 cm in size, and involves the styloid process of the fibula. It is displaced superiorly and medially. It signifies avulsion of arcuate complex or posterolateral ligament complex.
Joint Effusion
CT arthrography
CT arthrography is considered to have high specificity and sensitivity in detecting ACL disruption. CT is helpful in characterizing the avulsion bone fragment when it is present.
MRI
Imaging of ACL tears can be divided into primary and secondary signs.
Primary signs are those that pertain to the ligament itself. Secondary signs are those which are closely related to ACL injuries.
Primary signs
- swelling
- increased signal on T2
- fiber discontinuity/ non-visualization of ACL – Typically occur in the middle portion of the ligament
- change in the expected course of ACL
Secondary signs
These include:
- Bone contusion in lateral femoral condyle and posterolateral tibial plateau[seen in 90%]
- >7 mm of anterior tibial translation [Anterior tibial translocation sign]
- Uncovered posterior horn of the lateral meniscus
- Segond fracture, and to a lesser degree arcuate sign
- Reduced posterolateral cruciate ligament angle due to buckling of PCL
MRI has a sensitivity of 90-98% for ACL tears.
Treatment of Anterior Cruciate Ligament
Decision of the Treatment
A torn ACL ligament needs surgical treatment to restore the function. Following factors determine if patient require to undergo surgery
- Preinjury activity level
- Associated injuries
- Abnormal laxity
- Patient’s expectations
- Age of the patient
Activity level is the biggest determinant of the need for surgery followed by age.
International Knee Documentation Committee Classification of Activity Levels
divides the activity levels into four types
Level I
Activities like jumping, pivoting, and hard cutting
Level II
Heavy manual work or side-to-side sports
Level III
Light manual work and noncutting sports (eg, running and cycling)
Level IV
Sedentary activity without sports
Generally speaking, nonsurgical treatment may be considered, with due inputs for other factors in patients with level III or IV activities.
All others should be considered as candidates for surgery.
Young patients should always be considered for surgery because of potential complications from recurrent instability.
Surgical intervention is recommended to be delayed at least 3 weeks following injury to prevent the complication of arthrofibrosis but very prolonged delay [>6 months] is strongly associated with a higher risk of medial meniscus injury and decreased repair rate.
Nonoperative Treatment
This includes symptomatic treatment, physical therapy, and lifestyle modification. It is considered for patients with low demands.
It should be avoided in patients with loss of meniscal integrity and increased buckling episodes. In such cases, the higher chondral damage is associated with non-operative treatment. The goal is to obtain a full ROM and strength compared with the uninjured knee.
Arthroscopy may also be considered for persons who are poor candidates for reconstruction but have a mechanical block to range of motion.
Surgical treatment
ACL reconstruction
It is the criterion standard for treating ACL tears. It involved taking a suitable tendon graft and reconstruction of the ligament. It is indicated in
- Younger, more active patients including children
- older active patients
- Prior ACL reconstruction failure
- In presence of associated injuries
- MCL injury – allow MCL to heal and then ACL reconstruction is done
- Meniscal tear – Both operated at the same time
- Posterolateral corner injury– Simultaneous reconstruction or repaired in the first stage before anterior cruciate ligament surgery which is done at a later stage.
Ligament Repair
Intraarticular repair traditionally has a high failure rate and is not recommended except for bony avulsions
Extra-articular repair involves a tenodesis of the iliotibial tract. This may prevent a pivot shift but has not been shown to decrease anterior tibial translation.
Grafts used in ACL Reconstruction
Autografts
These grafts use patient’s own tissues
Bone-patellar-bone autograft
This is currently popular because they yield a significantly higher percentage of stable knees with a higher rate of return to preinjury sports. It has the longest history of use and considered the “gold standard. It provides bone to bone healing and ability to rigidly fix the screws.
Maximum load to failure is 2600 Newtons (intact ACL is 1725 Newtons)
Complications are
- patella fracture
- patellar tendon rupture
- re-rupture of ACL
- postop anterior knee pain
Quadruple hamstring autograft
Taken from ipsilateral side in fresh surgery and contralateral side in revision.
It requires a smaller incision. It is associated with less perioperative pain, less anterior knee pain though fixation strength may be less than Bone-Patellar tendon-Bone.
Maximum load to failure is approximately 4000 Newtons.
Moreover, there are concerns about hamstring weakness in female athletes leading to increased risk of re-rupture.
Complications include residual hamstring weakness
Quadriceps tendon autograft
It is taken with patella bone plug but us used much less common
Allograft
Allografts are useful in revisions [one host tissue has already been already used ] but are associated with longer incorporation time.
Allografts are associated with risk of disease transmission especially HIV, hepatitis [a risk across all allograft tissues, not only musculoskletal]
There is also increased risk of re-rupture.
The type of processing used may affect the strength of the graft.
Treatment Considerations in Pediatric Patients
These are the patients where physis are open. [< 14 yrs, generally speaking, maybe earlier in females (onset of menarche is the best determinant of skeletal maturity)] physis
Nonoperative treatment may be considered in compliant, low demand patient with no additional intra-articular pathologies and those with partial ACL tear (60% of adolescents have partial tears) with near normal Lachman and pivot shift
Surgery is indicated in complete ACL tear.
Repair has a greater role in this population.
Postoperative rehabilitation
Immediate
- Aggressive cryotherapy (ice application)
- Immediate weight bearing (shown to reduce patellofemoral pain)
- Emphasize early full passive extension(especially if associated with MCL injury or patella dislocation)
Early rehabilitation
The focus is on exercises that do not place excess stress on graft
- Eccentric strengthening at 3 weeks has been shown to result in increased quadriceps volume and strength
- Isometric hamstring contractions at any angle
- Isometric quadriceps, or simultaneous quadriceps and hamstrings contraction
- Active knee motion between 35 degrees and 90 degrees of flexion
- Emphasize closed chain exercises
Following should be avoided
- isokinetic quadricep strengthening (15-30°) during early rehab
- open chain quadriceps strengthening
Overall Rehabilitation Therapy Protocol
It may be divided into the following 4 phases
Phase I
- Preoperative period
- The goal is to maintain full ROM.
Phase II
- (0-2 wk – post surgery)
- The goal is to achieve full extension, maintain quadriceps control, minimize swelling, and achieve flexion to 90o.
Phase III
- (3-5 wk)
- Maintain full extension and increase flexion up to full ROM.
- Stair-climbers and bicycles may be used.
Phase IV
- (6 wk)
- Increase strength and agility, progressive return to sports.
- Return to all sports may take 6-9 months
- The use of knee braces remains a highly controversial
Drugs used in ACL injuries
Medication for ACL injuries mainly consists of analgesics. Antibiotics may be needed during perioperative period.
Return to Play
Once quadriceps strength reaches 65% of the opposite leg, sports-specific activities may be performed usually within 5-8 weeks postsurgery.
The athlete may return to activity when the quadriceps strength has reached 80%, which is usually after at least 3-4 months of sports-specific therapy but may go as long as 6-9 months.
Complications of Anterior Cruciate Ligament Injury
Graft Failure
The current failure rate for ACL reconstruction is approximately 8%.
Recurrent instability, secondary to significant laxity in the reconstructed ligament is the most common cause of graft failure. [Most common factor is tunnel malposition – femoral or tibial or both. Other factors like misplaced hardware and inadequate notchplasty may be responsible.]
Inadequate graft fixation, arthrofibrosis due to inflammation of the synovium and fat pad and pain that limits motion may also lead to graft failure too.
A missed diagnosis [ For example in combined ACL and PLC injuries, failure to treat the PLC will lead to failure of ACL reconstruction] or overaggressive rehab may also cause graft failure.
A graft also may fail due to a lack of incorporation, secondary to rejection or stress shielding.
Trauma from re-injury or aggressive rehabilitation also may cause graft failure. The incidence of graft re-rupture is approximately 2.5%.
Graft Impingement may result from anterior placement of a tibial tunnel or too posteriorly on the femoral side and impingement may lead to graft failure.
Infection
Infection though rare may lead to septic arthritis and is caused by coagulase negative Staph (S. epidermidis) and Staph aureus commonly.
The patient would present with pain, swelling, erythema, and increased WBC between 2-14 days.
Infection requires aggressive treatment with antibiotics, open or arthroscopic incision and drainage. Repeated drainage may enable graft retention, more so with staph epidermidis.
Loss of motion & Arthrofibrosis
To prevent this, it is prudent to wait until swelling (inflammatory phase) has reduced and the patient should be put on the range of motion exercises [pre-hab].
Proper tunnel placement and postop aggressive cryotherapy are also preventive measures.
In established cases, < 12 weeks, then treat with aggressive PT and serial splinting. Cases > 12 weeks, should be treated with lysis of adhesions/manipulation under anesthesia
Infrapatellar contracture syndrome
It is an uncommon complication following knee surgery or injury which results in knee stiffness. The physical exam will show decreased patellar translation
Patella Tendon Rupture
Patellar tendon rupture would lead to patella alta on the lateral radiograph.
Patella fracture
Most of the fractures occur 8-12 weeks postop.
Cyclops Lesion
Here the fibroproliferative tissue blocks extension
Other Complications
- Hardware failure
- Tunnel osteolysis
- Late arthritis [related to meniscal integrity]
- Local nerve irritation [saphenous nerve]
- Complex regional pain syndrome
Prognosis
Patients treated with surgical reconstruction of the ACL have long-term success rates of 82-95%.
Recurrent instability and graft failure is seen in approximately 8% of patients.
Patients with ACL ruptures, even after successful reconstruction, are reported at risk for osteoarthrosis.
The timing of surgery is an important factor in prognosis.
Patients who underwent surgery 6-12 weeks after injury had 1.45 times higher risk of the lateral meniscus injury and those who underwent surgery more than 12 weeks after injury had a 2.82-fold increased risk when compared with those who had surgery within 6 weeks after an ACL injury.
Other risk factors for secondary knee injuries were younger age, resumption of participation in sports before surgery, and earlier episodes of knee instability.
References
- Steckel H, Musahl V, Fu FH. The femoral insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: a radiographic evaluation. Knee Surg Sports Traumatol Arthrosc. 2010 Jan. 18(1):52-5.
- Duquin TR, Wind WM, Fineberg MS, Smolinski RJ, Buyea CM. Current trends in anterior cruciate ligament reconstruction. J Knee Surg. 2009 Jan. 22(1):7-12.
- Wipfler B, Donner S, Zechmann C, Springer J, Siebold R, Heinrich Paessler H. Anterior Cruciate Ligament Reconstruction Using Patellar Tendon Versus Hamstring Tendon: A Prospective Comparative Study With 9-Year Follow-Up. Arthroscopy. May 2011. 27(5):653-65.
- Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012 Mar. 40(3):595-605.
- Geib TM, Shelton WR, Phelps RA, Clark L. Anterior cruciate ligament reconstruction using quadriceps tendon autograft: intermediate-term outcome. Arthroscopy. 2009 Dec. 25(12):1408-14.